and, rarely, seizures
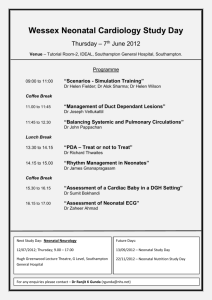
advertisement

Neonatal seizures Dr Naeeme Taslimi Taleghani Assistant Professor of Pediatrics (Neonatologist) Shahid Beheshti University of Medical Sciences 3/15/2016 • “Neonatal seizures continue to pose a challenge for clinicians worldwide because they are difficult to diagnose and treat and are associated with poor outcomes.” 3/15/2016 The immature brain is prone to seizures • The sensitivity to seizures is higher in the developing brain than during the rest of life: 1. External factors increase the susceptibility of the immature brain to seizures: birth trauma, hypoxicischemic insults, perinatal acquired infections, intracranial hemorrhage, fever and metabolic disturbances 2. In addition to insults, several neonatal disorders such as congenital brain anomalies, inborn errors of metabolism, and genetic factors can be initially present with seizures or can lead to recurrent seizures during the neonatal period. 3/15/2016 The immature brain is prone to seizures • Developmental factors predispose the immature brain to seizures • Besides external factors, various intrinsic factors make the immature brain more susceptible to seizures than the adult brain: 1. early development of excitatory neurotransmitter systems 2. delayed development of inhibition 3/15/2016 Effects of seizures in the immature brain • Whether or not the effects of seizures add to the long-term effects of their underlying cause is still not clear. • seizures may also produce indirect harmful effects on brain function. • The presence of seizures can alter these developmental sequences and lead to persistent deleterious effects. 3/15/2016 Epidemiology and etiology of neonatal seizures 3/15/2016 Epidemiology and etiology of neonatal seizures • Seizures constitute the most frequent and distinctive manifestation of neurological disturbance in the neonatal period . • The exact incidence of neonatal seizures in the general newborn population is difficult to estimate for a number of reasons: 1) clinical presentation of seizures in the neonatal period is subjective 2) In preterm infants, presentation is often subtle 3) The phenomenon of electro clinical dissociation or the ‘uncoupling’ of neonatal seizures is now well recognized. 3/15/2016 Epidemiology and etiology of neonatal seizures Timing of seizures: • Most neonatal seizures occur very early in life with nearly a third occurring within the first day, and another third occurring within the first week. 3/15/2016 Epidemiology and etiology of neonatal seizures Risk factors for neonatal seizures: 3/15/2016 Etiology of neonatal seizures Etiology of neonatal seizures 3/15/2016 3/15/2016 Clinical types of seizures in infants 3/15/2016 Clinical types of seizures in infants 3/15/2016 Selected Major Manifestations of Subtle Seizure Subtle Seizure Activity : a) b) c) d) e) orbital-ocular movements bucco-lingual movements unusual bicycling or pedaling autonomic findings :changes in heart rate, blood pressure, oxygenation Others: penile erections, skin changes, salivation, and tearing,… Autonomic expressions may be intermixed with motor findings. 3/15/2016 Differential diagnosis of epileptic seizures in infancy including the neonatal period 3/15/2016 Jitteriness ( recurrent tremors) Jitters are the most frequently occurring in the neonatal period 1. 2. 3. 4. 5. 6. It occurring in up to two-thirds of newborn babies in the first three days of life. It is seen most frequently in sleepy or active infants, and least frequently in quietly wakeful infants. They are most pronounced during vigorous crying, and diminish during the course of the first weeks. Tremors are stimulus sensitive, diminish with passive flexion of the extremity. Tremors are not associated with abnormality of gaze or eye movements. Tremors associated with metabolic conditions are usually of high frequency and low amplitude, whereas the tremors associated with CNS disorders are low frequency, high amplitude movements. 3/15/2016 cause of Jitteriness ( recurrent tremors) • The exact cause of jitteriness is not established. one theory is that neonatal tremor is due to immaturity of spinal inhibitory interneuron's causing an excessive muscle stretch reflex. Another theory is that elevated levels of circulating catecholamines account for the tremor. Jitteriness in its pronounced form maybe symptomatic of various conditions requiring specific attention: hypoglycemia, hypocalcaemia, sepsis, hypoxiceischaemic encephalopathy, intracranial hemorrhage and drug withdrawal. 3/15/2016 Benign neonatal sleep myoclonus (BNSM) • Myoclonus is a brief limb movement, a jerk, caused by a muscle contraction. • BNSM is a condition where such jerks occur only in sleep. • It is the most common condition misdiagnosed for epilepsy in the term neonate, and consequently over treated. 1) BNSM can be distinguished from epileptic myoclonus by the fact the jerks occur only during sleep, and settle on arousal. 2) It tends to occur in term healthy neonates 3) It is bilateral and repetitive, and may involve all limbs but not the face. 4) Onset is usually in the first few days of life, but it resolves by four months of age. 5) jerks resolve on arousal and are not associated with EEG change should this be performed during episodes. 3/15/2016 Apnea • Apnea spells in the neonate, defined as cessation of respirations for at least 20 s • This may or may not be associated with a transient bradycardia. • In preterm babies, the most common cause is immaturity, ‘apnea of prematurity’, where the normal stimulation of respiratory drive by arterial hypoxia and hypercapnia is delayed. • apnea beyond this period is more likely to be associated with other pathology, such as: sepsis, metabolic disorders, GER, poor pharyngeal coordination and, rarely, seizures. • With seizures as a cause in a term infant the only manifestation may be apnea, particularly with temporal lobe onset, and motor manifestations may not be demonstrated. 3/15/2016 Investigations for neonatal seizures 3/15/2016 Investigations for neonatal seizures • Seizures during the neonatal period are always medical emergencies. • Apart from the need for rapid anticonvulsive treatment, the underlying condition is often not immediately obvious. • In the search for the correct diagnosis: 1) A thorough history 2) Clinical examination 3) Laboratory work-up 4) Neurophysiologic and neuroradiological investigations 3/15/2016 Clinical history 3/15/2016 Clinical examination • • • • • • • The level of consciousness Tone Gaze body-posture Tendon reflex Cranial nerve and newborn reflexes The general body examination focuses on finding indications for an underlying disease condition • The skin is inspected for bleeding and bruising,eruptions,birth-marks (for example in the face, indicating phacomatosis) • Cardiac examination includes checking for murmurs, including auscultation over the fontanels as AVmalformations • Abdominal examination focuses on intraabdominal masses (liver, spleen, kidneys). 3/15/2016 Initial laboratory work-up 3/15/2016 Neuroimaging A. A cranial ultrasound is routine management in the investigation of neonatal seizures. • It should be carried out as soon as possible after the first occurrence of seizures . • It will help in early diagnosis of many underlying causes including : intraventricular hemorrhage arterial stroke malformation infections 3/15/2016 Neuroimaging • Magnetic resonance imaging (MRI) is the ‘gold standard’ in the examination of the newborn brain . • We suggest that computed tomography (CT) is reserved for emergency situations where MRI is not available and intracranial hemorrhage (particularly in the posterior fossa) is a real possibility. 3/15/2016 Monitoring neonatal seizures • All suspected neonatal seizures need EEG confirmation. • At-risk neonates should be continuously monitored using multiple EEG electrodes for a minimum of 72 h after birth. 3/15/2016 Treatment of neonatal seizures 3/15/2016 The most important questions that still need to be answered • Which drugs should we use ? • How aggressively should we treat neonatal seizures? • How long should we treat neonatal seizures? 3/15/2016 Acute Management of Neonatal Seizures • After each step, evaluate the infant for ongoing seizures. If seizures persist, advance to next step. • Step 1. Stabilize vital functions • Step 2.Correct transient metabolic disturbances • a. Hypoglycemia (target blood sugar 70-120 mg/dL) 10% dextrose water IV bolus dose 2 mL/kg followed by a continuous infusion at 8 mg/kg/min • B.Hypocalcemia :5% calcium gluconate IV at 4 mL/kg (need cardiac monitoring) • c. Hypomagnesemia :50% magnesium sulfate IM at 0.2 mL/kg 3/15/2016 Acute Management of Neonatal Seizures • Step 3. Phenobarbital 20 mg/kg IV load Cardiorespiratory monitoring 5 mg/kg IV (may repeat to total dose of 40 mg/kg) Consider continuous EEG monitoring Consider intubation/ventilation 3/15/2016 Acute Management of Neonatal Seizures • Step 4.Lorazepam 0.05 mg/kg IV (may repeat to total dose of 0.1 mg/kg) • Step 5.Phenytoin (fosphenytoin) 20 mg/kg slow IV load 5 mg/kg slow IV (may repeat to total dose of 30 mg/kg) • Step 6.Pyridoxine 50-100 mg/kg IV (with EEG monitoring) 3/15/2016 Outcome following neonatal seizures 3/15/2016 Factors determining high risk of poor outcome in neonatal seizures: 3/15/2016 Associated with favorable outcome: 3/15/2016 Sugar & Safe Care Temperature Airway Blood Pressure Lab Work Emotional Support 3/15/2016 THANKS FOR YOUR ATTENTION 3/15/2016