File
advertisement

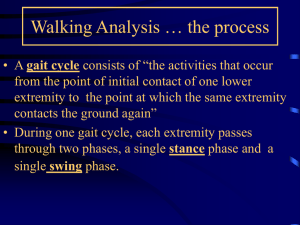
GAIT ANALYSIS & GAIT TRAINING Identify phases of the gait cycle Differentiate between stride and step length Introduce common pathological gait patterns Define terms used to describe normal gait Identify joint specific gait abnormalities in lower extremities Gait is one of the most basic components of independent function A common goal of rehabilitation is to restore or improve the ambulatory status of a patient Purpose of Gait Analysis: Assist with understanding the gait characteristics of a particular disorder Assist with movement diagnosis Determine proper interventions Evaluate the effectiveness of treatment The gait cycle begins when the heel of the reference extremity contacts the supporting surface and ends when the heel of the same extremity contacts the ground again The gait cycle is divided into two phases: Stance – The interval in which the foot is on the ground (60% of the gait cycle) Swing – The interval in which the foot is not in contact with the ground (40% of the gait cycle) Refers to the interval in a gait cycle in which body weight is transferred from one foot to the other and both right and left feet are in contact with the ground at the same time Two periods of double support occur within a single gait cycle Traditional Terminology Rancho Terminology Heel strike Footflat Midstance Heel-off Toe-off Initial contact Loading response Midstance Terminal stance Preswing Traditional Terminology Rancho Terminology Acceleration Midswing Deceleration Initial swing Midswing Terminal swing Refer to O’Sullivan (pg. 255) for differences between the two terminologies Heel strike to foot flat Foot flat through midstance Midstance to heel off Heel off to toe off Normal Motion: 0 -15 degrees PF Normal Muscle Activity: Eccentric contraction of tibialis anterior Result of Weakness: Lack of PF causes the foot to slap the floor Normal Motion: 15 degrees PF to 10 degrees DF Normal Muscle Activity: Gastroc and soleus muscles act eccentrically Result of Weakness: Excessive DF and uncontrolled tibial advance Normal Motion: 10-15 degrees of dorsiflexion Normal Muscle Activity: Gastroc and soleus contract eccentrically Result of Weakness: Excessive DF and uncontrolled forward motion of tibia Normal Motion: 15 degrees DF to 20 degrees PF Normal Muscle Activity: Gastroc, soleus, peroneals, and flexor hallicus longus contract to PF the foot Result of Weakness: No roll off. Decreased contralateral step Acceleration to midswing Midswing to deceleration Normal Motion: Dorsiflexion to neutral Normal Muscle Action: Dorsiflexors are contracting to bring the ankle into neutral Result of Weakness: Foot drop and/or toe dragging Normal Motion: Neutral Normal Muscle Action: Dorsiflexion Result of Weakness: Foot drop and/or toe dragging What happens at the knee during the stance phase and swing phase of gait? Tables 10.4 and 10.5 Page 323 in O’Sullivan What happens at the hip during the stance phase and swing phase of gait? Tables 10.6 and 10.7 Page 324 in O’Sullivan Stride Length The distance between corresponding contact points of the same foot (e.g., distance from heel strike to heel strike of the same foot) Step Length The distance between corresponding contact points of opposite feet (e.g., distance from heel strike of one foot to heel strike of the opposite foot) Stride Width The lateral distance between the feet (continued) COG located at S1 - S2 During preferred rate walking the COG approximates a sinusoidal curve from the: Sagittal perspective - no greater than a 2” peakto-valley excursion Frontal perspective - no greater than a 2” medialto-lateral excursion If the COG deviates too far from the norm increased energy is required Example: Walking with a stiff-knee (“stiff-knee gait”) while in a brace/cast During stance phase the patient will vault over the fixed foot (especially during mid-stance) COG will be deflected higher than the usual 2” upward vertical displacement with increased energy cost Requirements for normal gait: Normal range of motion Normal and balanced muscle strength Normal balance Stabile structures for weight acceptance Normal control of reciprocal gait pattern both in symmetry and muscle activation sequence Motor control options: ‘Manual’ control theory – Thinking about having to take a step each time you want to advance the foot forward ‘Automatic’ control theory – An automatic control system that accounts for gait mechanics without having to think about foot placement and other metrical details Free or comfortable walking speed Self-selected pace Rate at which the normal individual is most energy efficient Range: ~2.5 - 4.0 mph (cadence of ~75 - 120 steps per minute) Will vary from individual-to-individual Results when a segment is not able to move as it should Common Causes: Injury Weakness, loss of flexibility Pain Bad habits As a result, compensations occur elsewhere in the body with resultant effects (stress, weakness, and further injury) Propulsive Scissors Spastic Steppage Waddling Trendelenberg Antalgic Leg length discrepancy Circumduction Vaulting Hip Hiking Quadriceps Gait Stiff Knee Gait Propulsive Gait A stooped, rigid posture, with the head and neck bent forward; Balance deficit Scissors Gait Characterized by legs flexed slightly at the hips and knees, giving the appearance of crouching, with the knees and thighs hitting or crossing in a scissor-like movement Spastic Gait A stiff, foot-dragging walk caused by one-sided, longterm, muscle contraction Steppage Gait Foot drop where the foot hangs in plantarflexion, toes can scrape the ground during swing phase; Exaggerated hip and knee flexion used to clear toes Waddling Gait – A distinctive duck-like walk; trunk sways side to side; wide base of support Trendelenburg Gait Weakness of the hip abductor muscles; pelvis drops on the contralateral side with compensatory lateral trunk lean over that side Antalgic Gait Pattern- A protective gait pattern Stance time is usually limited on the painful limb resulting in uneven timing and/or uneven step lengths The uninvolved limb will demonstrate a shortened step length since it must bear weight sooner than normal Pain promotes a modification of the gait pattern to avoid joint motions, muscle contraction and weight bearing that sustains or may increase the pain Functional Leg length discrepancy – The pelvis dips downwards on the side of the shortened limb with compensatory lateral trunk bend Circumduction Secondary to hip flexor weakness; adductor muscles act as hip flexors while the hip joint is extended Hip hiking Pelvis lifts on the side of the swinging limb by contraction of spinal muscles and lateral abdominal wall; may also see posterior trunk lean Vaulting Used to increase ground clearance in swing phase by going up on the toes of the stance phase leg Stiff knee Gait – During stance the patient will vault over the fixed foot (especially during mid-stance) & COG will be deflected higher than the usual 2” upward vertical displacement Gluteus Medius Gait – (Trendelenburg Gait) Pelvis drops on contra-lateral non-weight bearing side Compensation – patient moves trunk laterally over the weak hip Quadriceps Gait – (weakened Quads) An immediate lurch occurs at heel strike forcing the femur backward & the trunk forward to passively lock the knee Compensation – COG moves anterior to the knee with increased forces at the knee joint & hip extensors The knee often buckles during this gait pattern Normal Strength Prevent contra-lateral hip from dipping greater than 5-8 degrees Stance-side abductor muscle group is active Loss of abductors: Positive Trendelenburg sign Weakness of abductors manifests as ‘lurching gait’ (toward stance side) Early stance (Heel strike – Foot flat) Guides knee into 20 degrees of flexion eccentrically (controls unlocking of the knee) Late stance (Heel off – Toe off) Controls for knee flexion (~40 degrees at TO) Early stance weakness/absence Inability to absorb energy Buckling Late stance weakness/absence Knee collapse into flexion -premature flexion into early swing Early stance (HS FF) & late stance (HO - TO) Prevent forward flexion of trunk acting on pelvis Early & late stance weakness/absence Trunk falls forward Loss of head and neck control Early stance (HS) Prevent hip flexion (jack-knifing) Early stance (HS FF) Guide hip into flexion eccentrically Early stance (HS) weakness/absence Hip/trunk collapses into flexion Early stance (HS FF) Trunk falls forward Early stance (HS FF) Lowers forefoot to floor eccentrically After forefoot contacts floor- pull tibia forward over foot Early stance weakness/absence Forefoot slaps to the floor - ‘drop-foot’ gait Loss of forward pull of tibia Late mid-stance Concentrically pulls tibia forward Late stance (HO - TO) Provides propulsive thrust during push off Early stance weakness/absence Loss of forward pull of tibia Loss of forward thrust - poor transition to early swing Late mid-stance Concentrically pulls tibia forward Late stance (HO - TO) Provides propulsive thrust during push off Early stance weakness/absence Loss of forward pull of tibia Loss of forward thrust - poor transition to early swing Late stance (HO - TO) Late stance weakness/absence Dynamically provide collateral stability to ankle when plantar flexed Secondary plantar flexor for forward thrust Ankle instability causing medial-lateral movement Potential for ankle injury - sprains Poor transition from late stance to early swing Late stance (HO - TO) Late stance weakness/absence Provide medial lateral stability to MTP joints (especially nos. 1 & 2) Improves forward propulsion and transition to early swing Excessive medial lateral ‘shimmy’ of hindfoot during HO Inefficient forward thrust Late stance - early swing (acceleration) Forward flexion of femur working with plantar flexors to accelerate LE in early swing Functionally shortens LE (with eccentric action of quadriceps and dorsiflexors) to prevent ‘toe-drag’ Late stance - early swing weakness/absence of forward acceleration after TO Toe may not clear the floor during swing through Compensate with circumduction at hip Mid-to-late swing (deceleration) Affects ‘toe-up’ concentrically Functionally shortens LE during swing through Mid-to-late swing weakness/absence Loss of ‘toe-up’ Compensation Increased hip flexion ‘steppage gait’ Circumduction at hip Late swing (deceleration) Decelerates tibial shank Provides for smooth transition between late stance and early swing Late swing weakness/absence ‘Impact on terminal extension’ - knee slapped into extension or hyperextension ROM – for any joint motion restriction Stretching – for soft tissue restriction or shortened muscle groups Strengthening for weakened musculature Gait training to address specific deviations May need temporary or permanent AD if deviations are significant Balance training HEP Instruction / Patient Education Modalities – as needed Orthotics Heel lift, or shoe build up for leg length discrepancies or foot drop Appropriate assistive device Functional activity training Gait belt Proper guarding techniques Proper lighting Clear unobstructed path Proper shoe wear Adherence to weight bearing status Use of appropriate device that has been fitted/measured for the patient Patient’s cognitive status Why could this statement be detrimental to your 83 y.o. patient? Mrs. Jones, while you’re walking, I want to go…” “...very slow!” Mr. Jones will be safe - probably won’t fall and break her hip The path of the COG may be distorted Energy cost Suppose Mrs. Jones has a cardiac condition? Mr. Jones’ gait may never return to ‘normal’ …going very slow might actually cause Mrs. Jones to lose her balance and fall? How? Mrs. Jones may never reach her preinjury/disease preferred rate of ambulation and therefore never trigger a CPG that automates gait What is a CPG? A group of synaptic connections at the spinal cord level which are triggered by an event or condition (perturbation) When a threshold is met via a triggering mechanism the CPG appears to be activated and takes over automatic control of gait metrics (the individual does not have to think about it) Are all patients’ objectives/goals the same? Are your objectives for Ms. Walksalot, a 39 year old healthy female who broke her ankle two weeks ago in an intensive tennis match, the same as… Mr. Livesinathirdstorywalkup, a frail 87 year old male, with emphysema and a fractured hip? It is important to keep the objectives/goals in mind during gait training Various assistive devices are available for use during gait/ambulation activities Parallel bars Walkers Bilateral & unilateral crutches Canes (single point, quad) Remember it is very important to properly guard your patient during gait training while using an assistive device in the clinic Progression from assistive device to normal gait Progress from assistive device with large base of support to small base of support 2 Axillary crutches or 2 Lofstrand crutches 1 Axillary crutch or 1 Lofstrand or 1 Straight cane Hemi-walker Straight cane Walker Quad Cane Document any deviations noted during gait training Did gait appear vigorous or labored? Was gait guarded or restrained – was the patient attempting to gain stability and security? Was the toe/floor clearance distance slightly decreased? Was there decreased reciprocal arm swing? Was there decreased step and/or stride length? Narrow or wider dynamic base of support? Increased lateral head movement? Increased or decreased rotation of pelvis? Any abnormal or pathological gait patterns noted? Gait distance / endurance Any shortness of breath or other physiological reactions Any episodes of loss of balance?