Lecture Outline Ch 23 Digestion Part 1
advertisement

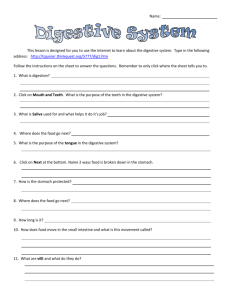
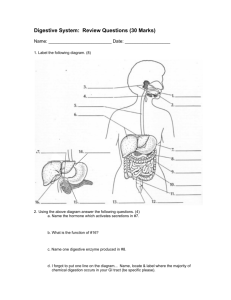
Lecture Outline Ch 22 Respiration I. Functional Anatomy of the Respiratory System (pp. 802–816; Figs. 22.1–22.11; Table 22.1) A. The respiratory system includes the nose, nasal cavity, and paranasal sinuses; pharynx, larynx, trachea, and bronchi; and the lungs, which contain tiny air sacs, the alveoli (p. 803; Fig. 22.1). 1. Functionally, the system has two zones: the respiratory zone, composed of the respiratory bronchioles, alveolar ducts, and alveoli, is the site of gas exchange; the conducting zone consists of all other respiratory passageways. B. The Nose and Paranasal Sinuses (pp. 803–806; Figs. 22.2–22.3; Table 22.1) 1. The nose provides an airway for respiration; moistens, warms, filters, and cleans incoming air; provides a resonance chamber for speech; and houses olfactory receptors. 2. The nose is divided into two divisions: the external nose, which is formed by hyaline cartilage and bones of the skull; and the nasal cavity, which is entirely within the skull. a. The external nose includes the root between the eyebrows, bridge and dorsum nasi anteriorly, ending at the apex, or tip: two exterior openings exist, the external nares. b. The nasal cavity is posterior to the external nose and is divided along the midline by a nasal septum, which ends at the pharynx, forming two openings, the choanae. c. The nasal cavity is lined with two types of mucous membranes: the olfactory mucosa, containing receptors for smell; and the respiratory mucosa, a pseudostratified columnar epithelium with scattered goblet cells for mucus production. d. Nasal conchae protrude into the nasal cavity from each lateral wall, increasing the mucosal surface exposure to air. e. The nasal cavity is surrounded by paranasal sinuses within the frontal, maxillary, sphenoid, and ethmoid bones that serve to lighten the skull, warm and moisten air, and produce mucus. C. The Pharynx (p. 806; Fig. 22.3; Table 22.1) 1. The pharynx connects the nasal cavity and mouth superiorly to the larynx and esophagus inferiorly. a. The nasopharynx serves as only an air passageway and contains the pharyngeal tonsil, which traps and destroys airborne pathogens. b. The oropharynx is an air and food passageway that extends inferiorly from the level of the soft palate to the epiglottis and houses the palatine and lingual tonsils. c. The laryngopharynx is an air and food passageway that lies directly posterior to the epiglottis, extends to the larynx, and is continuous inferiorly with the esophagus. D. The Larynx (pp. 807–809; Figs. 22.3–22.5; Table 22.1) 1. The larynx attaches superiorly to the hyoid bone, opening into the laryngopharynx, and attaches inferiorly to the trachea. 2. The larynx provides an open airway, routes food and air into the proper passageways, and produces sound through the vocal cords. 3. The larynx consists of hyaline cartilages: thyroid, cricoid, paired arytenoid, corniculate, and cuneiform; and the epiglottis, which is elastic cartilage. a. The epiglottis is designed to close off the larynx during swallowing to prevent food or liquids from entering the airways. b. The larynx houses vocal ligaments that form the true vocal cords, which vibrate as air passes over them to produce sound. c. The vocal folds and the medial space between them are called the glottis. 4. Voice production involves the intermittent release of expired air and the opening and closing of the glottis. a. As length and tension of the vocal folds changes, pitch of the voice varies; generally, as tension increases, pitch becomes higher. b. Loudness of the voice is determined by the force of the air forced over the vocal folds. 5. The larynx can act as a sphincter preventing air passage; Valsalva’s maneuver is a behavior in which the glottis closes to prevent exhalation and the abdominal muscles contract, causing intra-abdominal pressure to rise. E. The trachea, or windpipe, descends from the larynx through the neck into the mediastinum, where it terminates at the primary bronchi (p. 809; Fig. 22.6; Table 22.1). 1. The tracheal wall is similar to other tubular body structures, consisting of a mucosa, submucosa, and adventitia. 2. The trachea is lined with ciliated pseudostratified epithelium, designed to propel mucus upward toward the pharynx. 3. C-shaped cartilaginous rings associated with the connective tissue submucosa support the trachea, preventing collapse, while allowing the esophagus to expand normally during swallowing. 4. The trachealis is smooth muscle that decreases the trachea’s diameter during contraction, increasing the force of air out of the lungs. F. The Bronchi and Subdivisions (pp. 809–812; Figs. 22.7–22.9; Table 22.1) 1. The conducting zone consists of right and left primary bronchi that enter each lung and diverge into secondary bronchi that serve each lobe of the lungs. 2. Secondary bronchi branch into several orders of tertiary bronchi, which ultimately branch into bronchioles. 3. As the conducting airways become smaller, structural changes occur: a. The supportive cartilage changes in character until it is no longer present in the bronchioles. b. The mucosal epithelium transitions from pseudostratified columnar, to columnar, and finally, to cuboidal in the terminal bronchioles. c. The relative amount of smooth muscle in the walls increases, allowing significant changes in resistance to airflow in the smaller airways. 4. The respiratory zone begins as the terminal bronchioles feed into respiratory bronchioles that terminate in alveolar ducts within clusters of alveolar sacs, which consist of alveoli. a. The respiratory membrane consists of a single layer of squamous epithelium, type I alveolar cells, surrounded by a basal lamina. b. The external surface of the alveoli are densely covered by a web of pulmonary capillaries; the capillary endothelium and the alveolar epithelium together form the respiratory membrane, across which gas exchange occurs. c. Interspersed among the type I alveolar cells are cuboidal type II alveolar cells that secrete surfactant. d. Alveoli are surrounded by elastic fibers, contain open alveolar pores, and have alveolar macrophages. G. The Lungs and Pleurae (pp. 812–816; Figs. 22.10–22.11; Table 22.1) 1. The lungs occupy all of the thoracic cavity except for the mediastinum; each lung is suspended within its own pleural cavity and connected to the mediastinum by vascular and bronchial attachments called the lung root. 2. The left lung is smaller than the right because the position of the heart is shifted slightly to the left; each lung is divided into lobes, separated from each other by fissures. 3. Each lobe contains a number of bronchopulmonary segments, each served by its own artery, vein, and tertiary bronchus. 4. Lung tissue consists largely of air spaces, with the balance of lung tissue, its stroma, comprised mostly of elastic connective tissue. 5. There are two circulations that serve the lungs: the pulmonary network carries systemic blood to the lungs for oxygenation, and the bronchial arteries provide systemic blood to the lung tissue. 6. The lungs are innervated by parasympathetic and sympathetic motor fibers that constrict or dilate the airways, as well as visceral sensory fibers. 7. The pleurae form a thin, double-layered serosa. a. The parietal pleura covers the thoracic wall, superior face of the diaphragm, and continues around the heart between the lungs. b. The visceral pleura covers the external lung surface, following its contours and fissures. c. Pleural fluid lubricates the space between the pleurae to allow friction-free movement during breathing. d. The pleurae divide the thoracic cavity into three discrete chambers, preventing one organ’s movement from interfering with another’s, as well as limiting the spread of infection. II. Mechanics of Breathing (pp. 816–824; Figs. 22.12–22.16; Tables 22.2–22.3) A. Respiratory pressures are described relative to atmospheric pressures: a negative pressure indicates that the respiratory pressure is lower than atmospheric pressure (pp. 816–817; Fig. 22.12). 1. Intrapulmonary pressure is the pressure in the alveoli, which rises and falls during respiration, but always eventually equalizes with atmospheric pressure. 2. Intrapleural pressure is the pressure in the pleural cavity. It also rises and falls during respiration, but is always about 4 mm Hg less than intrapulmonary pressure. a. The negative intrapleural pressure is due to the opposition of two forces: the recoil force and surface tension of alveolar fluid in the lungs vs. the natural tendency of the chest wall to pull outward. b. Neither force overcomes the other due to the fluid adhesion between the pleural membranes created by the presence of pleural fluid. B. Pulmonary Ventilation (pp. 817–820; Figs. 22.13–22.14) 1. Pulmonary ventilation is a mechanical process causing gas flow into and out of the lungs according to volume changes in the thoracic cavity. a. Boyle’s law states that at a constant temperature, the pressure of a gas varies inversely with its volume. 2. During quiet inspiration, the diaphragm and intercostals contract, resulting in an increase in thoracic volume, which causes intrapulmonary pressure to drop below atmospheric pressure, and air flows into the lungs. 3. During forced inspiration, accessory muscles of the neck and thorax contract, increasing thoracic volume beyond the increase in volume during quiet inspiration. 4. Quiet expiration is a passive process that relies mostly on elastic recoil of the lungs as the thoracic muscles relax. 5. Forced expiration is an active process relying on contraction of abdominal muscles to increase intra-abdominal pressure and depress the rib cage. C. Physical Factors Influencing Pulmonary Ventilation (pp. 820–821; Fig. 22.15) 1. Airway resistance is the friction encountered by air in the airways; gas flow is reduced as airway resistance increases. a. Airway resistance is greatest in the medium-sized airways due to two factors: upper airways are very large diameter, and lower airways, while smaller, are very numerous. 2. Alveolar surface tension due to water in the alveoli acts to draw the walls of the alveoli together, presenting a force that must be overcome in order to expand the lungs. a. Surfactant, produced by type II alveolar cells, reduces alveolar surface tension to an optimal amount. 3. Lung compliance is determined by distensibility of lung tissue and the surrounding thoracic cage and alveolar surface tension. a. Any decrease in resilience reduces compliance; factors such as chronic inflammation, the presence of nonelastic scar tissue, or decreased surfactant can reduce resilience of the lungs. D. Respiratory Volumes and Pulmonary Function Tests (pp. 821–823; Fig. 22.16; Table 22.2) 1. Respiratory volumes and specific combinations of volumes, called respiratory capacities, are used to gain information about a person’s respiratory status. a. Tidal volume (TV) is the amount of air that moves in and out of the lungs with each breath during quiet breathing and averages 500 ml per breath. b. The inspiratory reserve volume (IRV) is the amount of air that can be forcibly inspired beyond the tidal volume (2100–3200 ml). c. The expiratory reserve volume (ERV) is the amount of air that can be evacuated from the lungs after tidal expiration (1000–1200 ml). d. Residual volume (RV) is the amount of air that remains in the lungs after maximal forced expiration (about 1200 ml). 2. Respiratory capacities are sums of multiple respiratory volumes. a. Inspiratory capacity (IC) is the sum of tidal volume and inspiratory reserve volume and represents the total amount of air that can be inspired after a tidal expiration. b. Functional residual capacity (FRC) is the combined residual volume and expiratory reserve volume and represents the amount of air that remains in the lungs after a tidal expiration. c. Vital capacity (VC) is the sum of tidal volume, inspiratory reserve, and expiratory reserve volumes and is the total amount of exchangeable air. d. Total lung capacity (TLC) is the sum of all lung volumes. 3. The anatomical dead space is the volume of the conducting zone conduits, roughly 150 ml, which is a volume that never contributes to gas exchange in the lungs. 4. Pulmonary function tests evaluate losses in respiratory function using a spirometer to distinguish between obstructive and restrictive pulmonary disorders. a. Obstructive pulmonary diseases involve hyperinflation of the lungs and are characterized by increased TLC, FRC, and RV. b. Restrictive pulmonary disorders, in which expansion of the lungs is limited, display low VC, TLC, FRC, and RV. E. Nonrespiratory Air Movements (p. 823; Table 22.3) 1. Nonrespiratory air movements cause movement of air into or out of the lungs, but are not related to breathing (coughing, sneezing, crying, laughing, hiccups, and yawning). III. Gas Exchanges Between the Blood, Lungs, and Tissues (pp. 824–828; Figs. 22.17–22.19; Table 22.4) A. Gases have basic properties, as defined by Dalton’s law of partial pressures and Henry’s law (pp. 824–825; Table 22.4). 1. Dalton’s law of partial pressures states that the total pressure exerted by a mixture of gases is the sum of the pressures exerted by each gas in the mixture. 2. Henry’s law states that when a mixture of gases is in contact with a liquid, each gas will dissolve in the liquid in proportion to its partial pressure. B. The composition of alveolar gas differs significantly from atmospheric gas due to gas exchange occurring in the lungs, humidification of air by conducting passages, and mixing of alveolar gas that occurs with each breath (p. 825). C. External Respiration (pp. 825–827; Figs. 22.17–22.19) 1. External respiration involves O2 uptake and CO2 unloading from hemoglobin in red blood cells. a. A steep partial pressure gradient exists between blood in the pulmonary arteries and alveoli, and O2 diffuses rapidly from the alveoli into the blood, until it reaches equilibrium at PO2 of 104 mm Hg. b. Carbon dioxide moves in the opposite direction along a partial pressure gradient that is much less steep, reaching equilibrium at 40 mm Hg. c. The difference in the degree of the partial pressure gradients of oxygen and carbon dioxide reflects the fact that carbon dioxide is much more soluble than oxygen in the blood. 2. The respiratory membrane is normally very thin and presents a huge surface area for efficient gas exchange. 3. Ventilation-perfusion coupling ensures a close match between the amount of gas reaching the alveoli and the blood flow in the pulmonary capillaries. a. In order to optimize perfusion and maximize oxygen uptake into the blood, arterioles feeding areas with low PO2 constrict, while arterioles serving well ventilated areas dilate. b. To increase ventilation so that there can be more rapid elimination of CO2 from the body, bronchioles serving areas with high alveolar CO2 dilate, but in areas with low CO2, bronchioles constrict. c. Ventilation and perfusion are balanced so that they work together to make O2 and CO2 levels match physiological demands. D. Internal Respiration (pp. 827–828; Fig. 22.17) 1. The diffusion gradients for oxygen and carbon dioxide are reversed from those for external respiration and pulmonary gas exchange. 2. The partial pressure of oxygen in the tissues is always lower than the blood, so oxygen diffuses readily into the tissues, while a similar but less dramatic gradient exists in the reverse direction for carbon dioxide. VIII. Developmental Aspects of the Respiratory System (pp. 841–844; Fig. 22.28) A. By the fourth week of development, the olfactory placodes are present and give rise to olfactory pits that form the nasal cavities (p. 841; Fig. 22.28). B. The nasal cavity extends posteriorly to join the foregut, which gives rise to an outpocketing that becomes the pharyngeal mucosa. Mesoderm forms the walls of the respiratory passageways and stroma of the lungs (pp. 841–842; Fig. 22.28). C. As a fetus, the lungs are filled with fluid, and vascular shunts are present that divert blood away from the lungs; at birth, the fluid drains away, and rising plasma PCO2 stimulates respiratory centers (p. 842). D. Respiratory rate is highest in newborns, and gradually declines in adulthood; in old age, respiratory rate increases again (p. 842). E. As we age, the thoracic wall becomes more rigid, the lungs lose elasticity, and the amount of oxygen we can use during aerobic respiration decreases (p. 842). F. The number of mucus glands and blood flow in the nasal mucosa decline with age, as do ciliary action of the mucosa and macrophage activity (p. 844). Lecture Outline Ch 23 Digestion Part 1: Overview of the Digestive System (pp. 850–855; Figs. 23.1– 23.6) A. Digestive system organs fall into two main groups: the alimentary canal and the accessory organs (pp. 850–851; Fig. 23.1). 1. The alimentary canal, or gastrointestinal (GI) tract, is the continuous muscular digestive tube that winds through the body digesting and absorbing foodstuffs; its organs include: the mouth, pharynx, esophagus, stomach, small intestine, and large intestine. 2. Accessory digestive organs aid digestion physically and produce secretions that break down foodstuffs in the GI tract; the organs involved are the teeth, tongue, gallbladder, salivary glands, liver, and pancreas. I. Digestive Processes (pp. 851–852; Figs. 23.2–23.3) A. Ingestion is the simple act of putting food into the mouth (p. 851; Fig. 23.2). B. Propulsion moves food through the alimentary canal and includes both swallowing and peristalsis (p. 851; Figs. 23.2–23.3). C. Mechanical digestion is the physical process of preparing the food for digestion and involves chewing, mixing, churning, and segmentation (pp. 851–852; Fig. 23.2). D Digestion is a series of catabolic steps in which complex food molecules are broken down to their chemical building blocks by enzymes (p. 852; Fig. 23.2). E. Absorption is the passage of digested end products from the lumen of the GI tract through the mucosal cells into the blood or lymph (p. 852; Fig. 23.2). F. Defecation eliminates indigestible substances from the body via the anus as feces (p. 852; Fig. 23.2). II. Basic Functional Concepts (p. 852; Fig. 23.4) A. The digestive system creates an optimal internal environment for its functioning in the lumen of the GI tract, an area that is technically outside of the body (p. 852; Fig. 23.4). 1. Digestive activities within the GI tract are triggered by mechanical and chemical stimuli. 2. Controls of the digestive activity are both extrinsic and intrinsic (nervous and hormonal). III. Digestive System Organs: Relationships (pp. 852–855; Figs. 23.5–23.6) A. Relationship of the Digestive Organs to the Peritoneum (pp. 852–854; Fig. 23.5) 1. The visceral peritoneum covers the external surfaces of most of the digestive organs, and the parietal peritoneum lines the body wall of the abdominopelvic cavity. 2. The peritoneal cavity is located between the visceral and parietal peritoneums and is filled with serous fluid. 3. Mesentery is a double layer of peritoneum that extends to the digestive organs from the body wall. It allows blood vessels, lymphatics, and nerves to reach the digestive organs; holds the organs in place; and stores fat. 4. Retroperitoneal organs are found posterior to the mesentery, lying against the dorsal abdominal wall. B. The splanchnic circulation serves the digestive system and includes those arteries that branch off the abdominal aorta to serve the digestive organs and the hepatic portal circulation (p. 854). C. Histology of the Alimentary Canal (pp. 854–855; Fig. 23.6) 1. Mucosa is the innermost, moist, epithelial membrane that lines the entire digestive tract. It secretes mucus, digestive enzymes, and hormones; absorbs digestive end products into the blood; and protects against infectious disease. 2. Submucosa is a moderately dense connective tissue layer containing blood and lymphatic vessels, lymphoid follicles, and nerve fibers. 3. Muscularis externa typically consists of smooth muscle and is responsible for peristalsis and segmentation. 4. Serosa, the protective outer layer of the intraperitoneal organs, is the visceral peritoneum. D. The alimentary canal has its own nerve supply made up of enteric neurons that communicate widely with each other to regulate digestive activity (p. 855). Part 2: Functional Anatomy of the Digestive System (pp. 856–892; Figs. 23.7–23.31; Tables 23.1–23.3) IV. The Mouth and Associated Organs (pp. 856–861; Figs. 23.7–23.11) A. The mouth is a stratified squamous epithelial mucosa-lined cavity with boundaries of the lips, cheeks, palate, and tongue (pp. 856–861; Figs. 23.7–23.11). 1. The lips and cheeks have a core of skeletal muscle covered externally by skin that helps to keep food between the teeth when we chew. a. The fleshy lips are formed by the orbicularis oris muscle; the cheeks are formed largely by the buccinators. b. The oral vestibule is the space between the lips and cheeks and gums and teeth. c. The area within the teeth and gums is the oral cavity proper. 2. The palate forms the roof of the mouth and has two parts: a. The anterior hard palate, is formed by the palatine process of the maxilla and the palatine bones, forms a rigid surface that the tongue manipulates food against. b. The posterior soft palate is formed by skeletal muscle that rises to close off the nasopharynx during swallowing. 3. The tongue is made of interlacing bundles of skeletal muscle and is used to reposition food when chewing, mix food with saliva, initiate swallowing, and help form consonants for speech. a. A fold of mucosa, the lingual frenulum, anchors the tongue to the floor of the mouth. b. Several types of papillae are located on the superior surface of the tongue: filiform papillae that are used to provide friction against foods, fungiform papillae that contain taste buds, and vallate and foliate papillae that house taste buds and secrete lingual lipase. 4. Major and minor salivary glands produce saliva, which cleanses the mouth, dissolves food chemicals for taste, moistens food, contains antibodies and defensins to protect against microorganisms, and is a source of chemicals that begin the breakdown of starches. 5. The teeth tear and grind food, breaking it into smaller pieces. a. The primary dentition, also called deciduous, or baby, teeth consists of 20 teeth that are lost to make way for the permanent dentition. b. The permanent dentition consists of 32 teeth, including the wisdom teeth, or third molars. c. Teeth are classified by their shapes and functions: incisors are used for cutting, canines tear or pierce, and premolars and molars are used for grinding. d. Each tooth has two regions: the enamel covered crown extending above the gingiva, or gum, and the root, which is embedded in the jawbone. e. Cement, a calcified connective tissue, anchors the root to the periodontal ligaments, which hold the tooth in the bony socket of the jaw. f. Dentin, a bonelike material, underlies the enamel and surrounds the pulp cavity, containing blood and nerve supply. V. The Pharynx (pp. 861–862) A. The pharynx (oropharynx and laryngopharynx) provides a common passageway for food, fluids, and air (pp. 861–862). VI. The Esophagus (pp. 862–863; Fig. 23.12) A. The esophagus provides a passageway for food and fluids from the laryngopharynx to the stomach where it joins at the cardial orifice (pp. 862–863; Fig. 23.12). VII. Digestive Processes: Mouth to Esophagus (pp. 863–864; Fig. 23.13) A. Mastication, or chewing, begins the mechanical breakdown of food and mixes the food with saliva (p. 863). B. Deglutition, or swallowing, is a complicated process that involves two major phases (p. 863; Fig. 23.13). 1. The buccal phase is voluntary and occurs in the mouth where the bolus is forced into the oropharynx. 2. The pharyngeal-esophageal phase is involuntary and occurs when food is squeezed through the pharynx and into the esophagus. VIII. The Stomach (pp. 864–874; Figs. 23.14–23.20; Tables 23.1–23.2) A. The stomach is a temporary storage tank where the chemical breakdown of proteins is initiated and food is converted to chyme (pp. 864–865; Fig. 23.14). 1. The adult stomach varies from 15–25 cm long; its diameter and volume vary depending on the amount of food it contains. a. The major regions of the stomach include the cardial part, fundus, body, and the pyloric part. b. The convex lateral surface of the stomach is its greater curvature, and its convex medial surface is its lesser curvature. c. Extending from the curvatures are the lesser omentum and the greater omentum, which help to tie the stomach to other digestive organs and the body wall. B. Microscopic Anatomy (pp. 866–869; Figs. 23.15–23.16; Table 23.1) 1. The surface epithelium of the stomach mucosa is a simple columnar epithelium composed of goblet cells, which produce a protective two-layer coat of alkaline mucus. 2. The gastric glands of the stomach produce gastric juice, which may be composed of a combination of mucus, hydrochloric acid, intrinsic factor, pepsinogen, and a variety of hormones. C. Digestive Processes in the Stomach (pp. 869–874; Figs. 23.17–23.20; Table 23.2) 1. Gastric secretion is controlled by both neural and hormonal mechanisms and acts in three distinct phases: the cephalic phase, the gastric phase, and the intestinal phase. 2. The reflex-mediated relaxation of the stomach muscle and the plasticity of the visceral smooth muscle allow the stomach to accommodate food and maintain internal pressure. 3. The enteric pacemaker cells establish the stomach’s basic electrical rhythm of peristaltic waves. 4. The rate at which the stomach empties is determined by both the contents of the stomach and the processing that is occurring in the small intestine. IX. The Small Intestine and Associated Structures (pp. 874–887; Figs. 23.21– 23.28; Tables 23.2–23.3) A. The small intestine is the site of the completion of digestion and absorption of nutrients (pp. 875–878; Figs. 23.21–23.23). 1. It extends from the pyloric sphincter to the ileocecal valve where it joins the large intestine. It has three subdivisions: the duodenum, the jejunum, and the ileum. 2. It is highly adapted for absorption with three microscopic modifications: circular folds, villi, and microvilli. 3. The intestinal crypts, secrete intestinal juice that serves as a carrier fluid for absorbing nutrients from chyme. B. The liver and gallbladder are accessory organs associated with the small intestine (pp. 878–882; Figs. 23.24–23.25). 1. The liver is the largest gland in the body and has four lobes. 2. The liver is composed of liver lobules, which are made of plates of liver cells (hepatocytes). 3. The digestive function of the liver is to produce bile, which is a fat emulsifier. 4. Bile is a yellow-green, alkaline solution containing bile salts, bile pigments (primarily bilirubin), cholesterol, neutral fats, phospholipids, and a variety of electrolytes. 5. The gallbladder stores and concentrates bile that is not needed immediately for digestion. 6. Bile does not usually enter the small intestine until the gallbladder contracts when stimulated by cholecystokinin. C. The pancreas is an accessory gland that is retroperitoneal (pp. 882–884; Figs. 23.26– 23.28). 1. Pancreatic juice consists mainly of water and contains enzymes that break down all categories of foodstuffs and electrolytes. 2. Secretion of pancreatic juice is regulated by local hormones and the parasympathetic nervous system. D. Digestive Processes in the Small Intestine (pp. 884–887; Tables 23.2–23.3) 1. Food takes 3–6 hours to complete its digestive path through the small intestine, the site of virtually all nutrient absorption. 2. Most substances required for digestion within the small intestine are imported from the pancreas and the liver. 3. Optimal digestive activity in the small intestine depends on a slow, measured delivery of chyme from the stomach. 4. Segmentation is the most common motion of the small intestine. X. The Large Intestine (pp. 887–892; Figs. 23.29–23.31; Table 23.2) A. The large intestine absorbs water from indigestible food residues and eliminates the latter as feces (pp. 887–890; Figs. 23.29–23.30). 1. The large intestine exhibits three unique features: teniae coli, haustra, and epiploic appendages, and has the following subdivisions: cecum, appendix, colon, rectum, and anal canal. 2. The mucosa of the large intestine is thick and has crypts with a large number of mucus-producing goblet cells. 3. Bacteria entering the colon via the small intestine and anus colonize the colon and ferment some of the indigestible carbohydrates. B. Digestive Processes in the Large Intestine (pp. 890–892; Fig. 23.31) 1. The movements seen in the large intestine include haustral contractions and mass movements. 2. Feces forced into the rectum by mass movements stretch the rectal wall and initiate the defecation reflex. Part 3: Physiology of Digestion and Absorption (pp. 892–901; Figs. 23.32–23.36) XI. Digestion (pp. 892–895; Figs. 23.32–23.34) A. Digestion is a catabolic process in which large food molecules are broken down to chemical building blocks (monomers), which are small enough to be absorbed by the GI tract lining (pp. 892–895; Figs. 23.32–23.24). 1. Digestion is accomplished by enzymes, secreted by intrinsic and accessory glands of the alimentary canal, used in hydrolysis reactions. 2. Carbohydrates a. Monosaccharides are simple sugars that are absorbed immediately (glucose, galactose, and fructose). b. Disaccharides are composed of two monosaccharides bonded together (maltose, lactose, and sucrose). c. The digestible polysaccharide found in the diet is starch; other polysaccharides, such as cellulose, are not able to be broken down by humans. d. Digestion of carbohydrates begins in the mouth, where salivary amylase breaks large polysaccharides into smaller fragments. 3. Proteins digested into amino acids in the GI tract include not only dietary proteins but also enzyme proteins secreted into the GI tract lumen. a. Pepsin, secreted by the chief cells, begins the digestion of proteins in the stomach. b. Rennin is produced in infants and breaks down milk proteins. c. Pancreatic enzymes, such as trypsin and chymotrypsin, further break down proteins in the small intestine. d. The brush border enzymes carboxypeptidase, aminopeptidase, and dipeptidase work on freeing single amino acids in the small intestine. 4. The small intestine is the primary site for lipid digestion. a. Lipases are secreted by the pancreas and are the enzymes that digest fats after they have been pretreated with bile. 5. Nucleic acids (both DNA and RNA) are hydrolyzed to their nucleotide monomers by pancreatic nucleases present in pancreatic juice. XII. Absorption (pp. 895–898; Fig. 23.35) A. Absorption occurs along the entire length of the small intestine, and most of it is completed before the chyme reaches the ileum (pp. 895–898; Fig. 23.35). 1. Absorption of Specific Nutrients a. Glucose and galactose are transported into the epithelial cells by common protein carriers and are then moved by facilitated diffusion into the capillary blood. b. Several types of carriers transport the different amino acids before entering the capillary blood by diffusion. c. Monoglycerides and free fatty acids of lipid digestion become associated with bile salts and lecithin to form micelles, which are necessary for lipid absorption. d. Pentose sugars, nitrogenous bases, and phosphate ions are transported actively across the epithelium by special transport carriers in the villus epithelium. e. The small intestine absorbs dietary vitamins, while the large intestine absorbs vitamins B and K. f. Electrolytes are actively absorbed along the entire length of the small intestine, except for calcium and iron, which are absorbed in the duodenum. g. Water is the most abundant substance in chyme and 95% of it is absorbed in the small intestine by osmosis. 2. Malabsorption of nutrients can result from anything that interferes with the delivery of bile or pancreatic juices, as well as factors that damage the intestinal mucosa.