My Children and Orthopedic Nursing Outline
advertisement

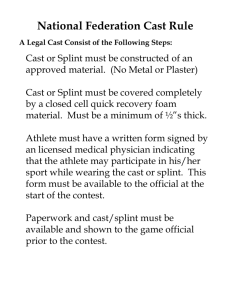
Children and Orthopedic Nursing Pain o Location o Nature o Frequency o Remember child may deny pain Pallor (skin color) o Warm Skin With Blue Tinge Possible Venous Status o Cool Pale Skin Possible Arterial Insufficiency Paralysis (movement) o Compare Bilaterally o Wiggling Fingers Or Toes Does Not Always Assess Motor Damage o Hard For A Young Child To Describe o Numb, Tingling “Bugs Crawling” “Pins And Needles” “Burning” “Asleep” o Loss Of Sensation Pulse o Assess Uninjured Limb First To Establish Baseline o Don’t Forget To Assess Capillary Refill Orthopedic Appliance o Clothing Between Appliance And Skin o No Lotion Under Appliance Can lead to yeast build up o No Powder Under Appliance Can be abrasive and cause skin breakdown o Toughen Skin In Contact With Metal Alcohol Or Tannic Acid o What About Balance? Legg-Calve-Perthes Disease o Info Avascular Necrosis of the femoral head which occurs in four stages o Patho Blood Flow To Femoral Head Is Interrupted Resulting In Bone Necrosis Blood Supply Returns To Femoral Head New Bone Remodeling Of New Bone Bone is taking the proper shape, very important Process Takes 18 Months to Several Years o Assessment Usually A Boy 2- To 12-Years-Old Slow Onset Limp Pain In Thigh, Hip, And/Or Knee o Worse With Activity, Relieved By Rest o Limited Motion o Eventually Muscle Atrophy Definitive Test Is MRI o Treatment Keep Head Of Femur In The Acetabulum (main concept in this disease process) Treatment Plan Is Influenced By Child’s Age o The younger the child the better the outcome because there is more time for that bone to remodel Condition Of The Femoral Head Position Within the Acetabulum o Overview Treatment Initial Therapy Is Rest Non-Weight Bearing Activity Can Cause Microfractures Conservative Versus Surgical Containment Later, Active Motion Is Encouraged o Nonsurgical Containment Non-Weight Bearing Devices Abduction Brace Leg Casts Leather Harness Sling Weight Bearing Devices Abduction-Ambulation Braces Casts After A Period Of Bed Rest And Traction Can Take 2 – 4 Years o Surgical Intervention Osteotomy Screws And Plates Spica Cast Frequently From Chest To Toes 6 – 8 Weeks Physical Therapy Partial-Weight Bearing o Prognosis Excellent In Most Cases Outcome Is Influenced By Child’s Age Early Treatment Possibilities Osteoarthritis Leg Length Discrepancy Osteomyelitis o Info Infection of a bone, primarily a long bone in children In Children: Most Common Between 1 – 12 Years Boys Affected More Often Than Girls Hematogenous Spread Organism Reaches The Bone Through The Blood There is an infection somewhere else in the body and the bug gets into the blood and then reaches the bone Open Fracture Or Wound Staphylococcus aureus o o o o o o Patho Bacteria adheres to bone Purulent exudates in bone tissue (pus) Exudates moves beneath the periosteum, abscess formation Necrosis of the bone Assessment Fever Irritability Pain with movement Swelling and warmth Labs Leukocytosis Elevated Erythrocyte Sedimentation Rate (ESR) Tests for inflammation. Not where in the body that it’s located, just that there is inflammation somewhere Cultures Blood culture looking for bugs in the blood, may also culture the joint nearest the infection Blood And Nearest Joint X-Ray, MRI, CT Scan, Bone Scan Medications Antibiotics 4 – 6 Weeks Important To Monitor Hematological, Renal, Hepatic, Ototoxic And Other Potential Side Effects Common Medications Nafcillin Clindamycin Vancomycin Interventions Assess And Document 5 P’s Pain Handle With Extreme Care On Bed Rest Or Wheelchair (Maybe) Immobilization (Probably) High Protein Diet Surgical Interventions Surgical Drain (Maybe) Two Tubes Are Placed In Wound One Tube Instills An Antibiotic Solution Directly Into Infected Area One Tube Provides Drainage Surgical Removal Of Dead Bone (Sequestrectomy) (Maybe) Scoliosis o Info Curvature of the spine associated with vertebral rotation causing rib asymmetry, potentially effecting heart/lung function Structural Has to do with the spine itself The most common type we see is idiopathic and we see it during the growth spurts Adolescent Growth Spurt (is when you usually notice this) >10° Functional Factors Outside Spinal Column Like a leg length discrepancy, so when they stand up the spine is crooked, but when they sit down the spine is straight o Assessment Forward Bending Test Assess Standing And Bending Assess Symmetry o Shoulders o Scapulas o Waist o Hips Scoliometer Protractor Used To Measure Curvature Assess For Leg Length Discrepancy o Treatment Serial Observation (10° to 20°) Bracing (20° to 40°) Purpose Is To Prevent Further Curvature Usually Worn 16 – 23 Hours A Day Gradually Weaned Off Brace After Spinal Growth Has Stopped o May Wear At Night For 1 – 2 Years o Braces Braces do not correct the curve that is already there, but only prevents further curvature Boston Brace Standard, kind of off the rack, generic style for everyone TLSO Brace (Thoracolumbosacral Orthotic) Custom Fit, you get your own one of a kind brace Milwaukee Brace Kyphosis o Surgical Intervention > 40˚ Curve Realignment And Straightening Instrumentation Developmental Dysplasia of the hip o Info Separation of the femoral head from the acetabulum o Types Dysplasia Mildest Form Femoral Head Remains In Acetabulum Subluxation Greatest Percentage Of Cases Incomplete Dislocation Dislocation Femoral Head Not In Contact With Acetabulum o Infant Assessment Shortened Limb On Affected Side Asymmetry Of Gluteal Folds Ortolani Click Into Place When you move the leg and you hear a click, meaning the leg is in place Positive Barlow Sign Passive Dislocation Nursing Alert Ortolani and Barlow tests must be performed by an experienced clinician to prevent damage to the hip. If these tests are performed too vigorously in the first 2 days of life, persistent dislocation may occur o Child Assessment Level Of Knees Limp Leg Length Discrepancy Positive Trendelenburg Sign Stand On One Foot (Affected Side). Pelvis Tilts Downward On Normal Side o Treatment Newborn to 6 Months (treatment is crucial for the infant! Don’t want them to have a limp or whatever for the rest of their life) Pavlik Harness o Legs Abducted, Knees And Hips Are Flexed Holds the femoral head high in the acetabulum o Worn Continually 3 – 6 Months o Position Chest Halter At Nipple Line Fasten With Velcro o Position Legs And Feet In The Stirrups Hips Are Flexed And Abducted o Connect The Chest Halter And Leg Straps In Front Then In Back o Skin Is Marked With Indelible Ink At Strap Lines 6 to 8 months old Traction (but we don’t see this much anymore) Closed Reduction Under Anesthesia Spica Cast For ~ 2 – 4 Months Brace after the spica cast is taken off Older child Tenotomy Of Contracted Muscles o The muscles grow and tighten around the retarded hip joint, before we can fix the hip we have to address the muscles Reconstruction Of Acetabulum Cast (Spica) Rehab o May never have a perfect leg or walk, will have some degree of impairment, limp etc. Fractures o Types Bend Bent But Not Broken o May Bend 45° Or More Before Breaking Most Common In Ulna And Fibula o Often Associated With Fractures Of Radius And Tibia o Casts o o o o Greenstick Bent beyond edurance Buckle Compression Of Porous Bone o Occurs Near Growth Plate o Tends To Be Seen In Young Children Spinal Fracture Twisting Motion o Planted Foot, Twist To Throw Football o Skiing o Maltreat In Nonambulating Child Epiphyseal Growth Plate injury Weakest Point Of Bones Can Result In Growth Disturbance Assessment History Child’s Story May Not Be Reliable o Child May Be Afraid Of Getting In Trouble Muscle Contraction Muscles Contract To Splint Fracture Swelling Peaks In 1 – 2 Days Swelling and cast placement Swelling Peaks In 1 – 2 Days Current Trend Is To Cast 1 – 2 Days After Fracture o Don’t want to cast before swelling is done because you risk tissue damage and squishing of the arm or whatever in the cast Elevate o Above the level of the heart to help reduce swelling Bivalve Cast, If Needed Cut the cast in half then wrap it all with an ace bandage, holds the limb immobile, but loosened it to allow for circulation Synthetic Casts Dry Quickly (10 – 30 Minutes) Lightweight Can Be Durable In Water Cast Application Assess Limb For Alteration In Skin And Jewelry Tube Of Cloth Stockinet Over Area Bony Prominences Covered With Cotton Sheeting Wet Casting Material Molded To Limb Stockinet May Be Pulled Over Rough Edges Of Cast And Secured With Casting Material Casts: Nursing Cast To Dry Inside Out Don’t use heaters or blow dryers or whatever Reposition Wet Cast With Palms To Avoid Pressure Points (Hot Spots) These hot spots are sites of skin breakdown and possible infection After The Cast Has Dried Petal The Cast, If Needed o o o Petaling is like softening. Use tape that is strong, moisture resistant. Cut a circle on the tape that will be on the inside of the cast so there are no sharp edges or whatever against the skin. Kids don’t really like when you do this… With a Spica cast, don’t use the bar between the legs to move the child. If the bar breaks they have to go back and get a new cast. Also, for babies, put the diaper up underneath the cast, not over, or else it will get shitty, literally… Arm Sling Distributes Weight Evenly Over Large Area Of The Shoulders And Trunk, Not Just Neck Discouraged After First Few Days, Especially With Short Arm Cast Encourage Normal Movement, increases circulation which speeds up recovery A few other items Windows Allows Abdominal Expansion You basically cut a hole over the abd so they can eat Odor Can Indicate Infection Objects in Cast (very common for kids) Moisture in Cast 5 P’s of Circulation Cast removal Cast Cutter Cuts By Vibration Generates Heat Noisy Flakey Skin Traction o Purpose of traction Fatigue Muscle To Reduce Muscle Spasms Realign Bone Immobilize During Healing o Check these Position Of Frames, Splints, Etc. Ropes & Pulleys Alignment Good Working Order Weights Correct Amount Hanging Freely Bed Position o Manual Traction Limb is help in position by person Nurses are frequently the manual traction, we hold leg in position when someone is putting a cast on for example Once traction is released, the muscle spasms come back (this is with any kind of traction) o Skin Traction Primary Purpose Is To Decrease Painful Muscles Spasms Limited Weight To Prevent Skin Injury If “Oked” By Physician Remove Bandage Every 8 Hours to Assess Skin Manual Traction o Buck Traction o o o o o Short Term Immobilization Preoperative Management Of Muscle Spasm Associated With Fractures Dislocated Hip Pediatric pt tends to migrate toward the foot of the bed. May draw a line and tell the kid “Hey don’t let your butt get past this line” Bryant’s Traction (rarely seen) Hip Dislocation Or Fractured Femur Weigh Less Than 40 Pounds Buttocks Off The Bed This Is The Countertraction 7 – 10 Days Spica Cast, Maybe Skeletal Traction Primary Purpose Is Bone Realignment Pins, Wire, Tongs, Screws Are Implanted In Bone Longer Traction Time And Heavier Weights Than Skin Traction Nursing Alert “Skeletal traction is never released by the nurse (unless under direct supervision of a practitioner.)” 90° - 90° Traction Two 90° Angles Steinmann Pin Or Kirschner Wire In The Distal Fragment Of Femur Lower Portion Of Leg Is Supported In Cast Boot Or Sling Most common form of traction seen in pedi Traction Assessment Inspect Skin At Least Every 8 Hours External Hardware Inspect Insertion Sites For Inflammation o Drainage o Color o Odor Pin Care Controversy Pin Care Prevents Infection Pin Care Disrupts Skin’s Natural Barrier To Infection Triad of Injuries When A Child Is Hit By A Car Assess For Broken Femur Chest Injury Head Injury