Martha E. Brown, MD
PRN Associate Medical Director
And
UF Associate Professor of Psychiatry
Addiction Medicine Division
William Swiggart, MS, LPC/MHSP
Associate in Medicine
Co-Director
Vanderbilt Center for Professional Health
www.mc.vanderbilt.edu/cph
We judge ourselves by our motives
others judge us by our behavior.
AA saying
Goals
Give learners an overview of
disruptive/distressed behavior
Provide resources and examples
of interventions.
Disruptive/Distressed
Physician Behavior Objectives
Describe the Joint Commission requirements
List examples of disruptive behavior
Estimate the impact of disruptive behavior
Explore the etiology of disruptive behavior
Discuss the components of a comprehensive evaluation
Apply specific educational approaches
Identify some appropriate resources
2004 AAMC Council of Deans
“Physicians are often poorly socialized
and enter medical school with inadequate social skills
for practice.”
“There is a growing body of literature documenting
that residency programs do not prepare resident
physicians adequately for the practice of medicine.”
Joint Commission, Issue 40
July 9, 2008
Defined disruptive behavior as a Sentinel Event
Recognition that disruptive behavior can:
Foster medical errors
Contribute to poor patient satisfaction
Contribute to preventable adverse outcomes
Increase the cost of care (including malpractice)
Lead to turnover/loss of qualified medical staff
Sentinel Events
Defined by The Joint Commission as:
“Any unanticipated event in a healthcare setting resulting in
death or serious physical injury or psychological injury to a
person or persons not related to the natural course of the
patient’s illness.”
Joint Commission
Goal of including Disruptive Behavior as a Sentinel Event:
Reform health care settings to address the problem
There is a history of tolerance and indifference
Promote a culture of safety
Improve the quality of patient care by improving the
communication and collaboration of health care teams
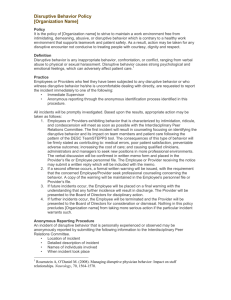
Joint Commission
Requirements
Hospitals establish a formal Code of Conduct
Leadership creates a process for reporting, evaluating
and managing disruptive behavior
Joint Commission
Recommendations
Educate all team members about professionalism
Hold all team members accountable for modeling
desirable behaviors
Enforce the code consistently and equitably
Non-confrontational intervention strategies
Progressive discipline
Definition of Disruptive
Behavior
Disruptive behavior includes, but is not limited to, words or actions
that:
Prevent or interfere w/an individual’s or group’s work, academic
performance, or ability to achieve intended outcomes (e.g.
intentionally ignoring questions or not returning phone calls or pages
related to matters involving patient care, or publicly criticizing other
members of the team or the institution)
Create, or have the potential to create, an intimidating, hostile,
offensive, or potentially unsafe work or academic environment (e.g.
verbal abuse, sexual or other harassment, threatening or intimidating
words, or words reasonably interpreted as threatening or
intimidating)
Threaten personal or group safety, such as aggressive or violent
physical actions
Behavior or behaviors that undermine a culture of safety
Violate Vanderbilt University and/or VUMC policies, including those
related to conflicts of interest and compliance
Vanderbilt University and Medical Center Policy #HR-027, 2010
Disruptive Behavior Is Not
An occasional “out of character” reaction of an individual
Lack of perfectionism. No one is perfect
Constructive criticism in good faith with the aim of
improving patient care or education
Expressions of concern about a patient’s care and safety
Expressions of dissatisfaction with policies through
appropriate grievance channels or other non-personal means
Vanderbilt University and Medical Center Policy #HR-027, 2010
Spectrum of Disruptive
Behaviors
Aggressive
Anger Outbursts
Profane/Disrespectful
Language
Throwing Objects
Demeaning Behavior
Jokes
Physical Aggression
Sexual Comments or
Harassment
Racial/Ethnic
Passive
Aggressive
Derogatory
comments about
institution,
hospital, group,
etc.
Refusing to do
tasks
Passive
Chronically late
Alcohol and other
drugs
Not responding
to call
Inappropriate or
inadequate chart
notes
Policies will not work if
disruptive behavior goes
unreported and unaddressed.
14
DVD
Examples of disruptive behavior and a do over
Why bother dealing with
disruptive behavior?
Failure to Address Disruptive
Conduct Leads to:
Perceptions of inequality when members of the team
compare their contributions to those of the disruptive
member (Kulik & Ambrose, 1992)
Some team members will decrease their contributions,
withdraw (Schroeder et al, 2003; Pearson & Porath,
2005)
Felps, W et al. 2006. How, when, and why bad apples spoil the barrel: negative group members and
dysfunctional groups. Research and Organizational Behavior, Volume 27, 175-222.
Failure to Address Disruptive
Conduct Leads To:
Team members may adopt disruptive person’s
negative mood/anger (Dimberg & Ohman, 1996)
Lessened trust among team members can lead to
lessened task performance (always monitoring
disruptive person)... effects quality and patient safety
(Lewicki & Bunker, 1995; Wageman, 2000)
Financial costs and litigation
Felps, W et al. 2006. How, when, and why bad apples spoil the barrel: negative group members and
dysfunctional groups. Research and Organizational Behavior, Volume 27, 175-222.
Failure to Address Disruptive
Conduct Leads To:
High turnover
Pearson et al, 2000 found that 50% of people who
were targets of disruptive behavior thought about
leaving their jobs
Found that 12% of people actually quit
These results indicate a negative effect on
return on investment
Felps, W et al. 2006. How, when, and why bad apples spoil the barrel: negative group members and dysfunctional
groups. Research and Organizational Behavior, Volume 27, 175-222.
Failure to Address Disruptive
Conduct Leads To:
disharmony and poor morale1,
staff turnover2,
incomplete and dysfunctional communication1,
heightened financial risk and litigation3,
reduced self-esteem among staff1,
reduced public image of hospital1,
financial cost1,
unhealthy and dysfunctional work environment1,
and potentially poor quality of care1,2,3
1. Piper, 2000
2. Rosenstein, 2002
3. Hickson, 2002
Disruptive Behavior Leads to Communication
Problems…Communication Problems Lead To
Adverse Events1
Communication breakdown factored in OR errors 50% of
the time2
Communication mishaps were associated with 30% of
adverse events in OBGYN3
Communication failures contributed to 91% of adverse
events involving residents4
Gerald B. Hickson, MD
James W. Pichert, PhD
Center for Patient & Professional Advocacy
Vanderbilt University School of Medicine
1. Dayton et al, J Qual & Patient Saf 2007; 33:34-44. 3. White et al, Obstet Gynecol 2005; 105(5 Pt1):1031-1038.
2. Gewande et al, Surgery 2003; 133: 614-621.
4. Lingard et al, Qual Saf Health Care 2004; 13: 330-334
Disruptive Behavior Creates
fear
confusion or uncertainty
vengeance vs. those who
oppose/oppress them
hurt ego/pride
grief (denial, anger,
bargaining)
apathy
burnout
unhealthy peer pressure
ignorance (expectations,
behavioral standards,
rules, protocols, chain of
command, standards of
care)
distrust of leaders
dropout: early retirement
or relocation
errors
disruptive behavior
begets disruptive
behavior
Vanderbilt University and Medical Center Policy #HR-027
Etiologies
Why Might a Medical
Professional Behave in Ways
that are Disruptive?
Evolution of distressed physicians risk
factors
Lack of Emotional Intelligence
Lack of awareness
Lack of clear boundaries
Multiple triggers
Slippery slope behaviors
Overworked and isolated
Burnout
Multiple etiologies
Why Might a Medical Professional
Behave in Ways that are Disruptive?
1. Substance abuse and psychiatric issues
Alcohol and Drugs
Psychiatric Disorders including Major Depressive,
Bipolar, & Anxiety Disorders
2. Narcissism, perfectionism or other personality
traits/disorders
3. Spillover of family/home problems
Gerald B. Hickson, MD
James W. Pichert, PhD
Center for Patient & Professional Advocacy
Vanderbilt University School of Medicine
©CPPA, 2008
Why Might a Medical Professional Behave
in Ways that are Disruptive? (cont’d)
4. Poorly controlled anger/Snaps under heightened stress,
perhaps due to:
a. Poor clinical/administrative/systems support
b. Poor mgmt skills, dept out of control
c. Back biters create poor practice environments
5. Well, it seems to work pretty well and the system
reinforces the behavior
6. No one addressed it earlier (why? See #5)
7. Family of origin issues—guilt and shame
8. Training or poor social skills entering into medicine
9.
10.
©CPPA, 2008
Two Systems Interact
The external system
Functional &
nurturing
The internal system
Hospital/Clinic
Physician
Dysfunctional
Good skills
Poor skills
“The Perfect Storm”
Systems
"Every system is perfectly
designed to get the results it
gets.”
BW Williams to accompany a talk delivered at the FSPHP Spring Meeting 2010
Individual Factors
Etiologies
Predisposing Psychological Factors (1)
Alcohol and Drug Family History
Trauma History
Religious Fundamentalism
Familial High Achievement, lack of skills regarding conflict
and negotiation and other family of origin patterns
Personality Traits (2)
Narcissism
Obsessive/Compulsive
Physician Burnout (3)
Clinical Skills Satisfactory or Above Average (4)
1.
3.
Valliant, 1972
Spickard and Gabbe, 2002
2.
4.
Gabbard, 1985
Papadakis, 2004, 2005
Etiologies
Institutional Factors (1)
Scapegoats
System Reinforces Behavior
Individual Pathology may over-shadow
institutional pathology
Williams and Williams, 2004
Methods to Address
Behavioral Problems
The role of a comprehensive evaluation
The importance of consequences
Educational programs
Feedback from colleagues, patients, staff, etc.
Monitoring and accountability
External resources
Clinical Approaches To
The Disruptive
Professional
What to do? (Protocol for all cases)
Confirm facts
Immediately talk with the professional and discuss that what
happened was not appropriate
Obtain assurances the behavior will not reoccur
Complete a record of the incident and conversation for the
personnel file
Closely follow up and monitor their behavior
Do not be intimidated by threats of legal action
Step-wise Protocol for Handling
Disruption
First time incident of disruptive behavior that is relatively
“mild” and not egregious (i.e., routinely failing to complete
records in a timely manner affecting patient care, being
chronically late, or not answering pages) might be handled
by executive committee
CME course should be mandated in most cases (MD should
allow committee to talk with CME staff)
Mentoring of professional
Behavior closely watched by executive committee
CME Program for Distressed
Physicians
Originally developed at the Vanderbilt Center for Professional
Health (now offered at Vanderbilt, University of Florida, and
Professional Renewal Center)
Designed to address the specific needs of professionals
whose workplace conduct has become problematic, but not risen
to the point of a formal referral
3 days with 1 day follow-ups at 1, 3, and 6 months
Step-wise Protocol for Handling
Disruption
Repeated behavior that disrupts healthcare system or if 1st
incident particularly egregious (throwing objects,
continual/demeaning language such as profanity/sexual
comments) must be addressed more formally
Call your PHP to discuss whether formal assessment is
warranted or if referral to CME might be sufficient in lieu of
a more formal report to the PHP at this time
Brief contract outlining expectations/requirements should be
signed by professional (include written permission to talk
with CME staff or PHP)
Step-wise Protocol for Handling
Disruption
If behavior reaches a level that there is an immediate
risk of harm to patients or staff, then a more formal
procedure needs to happen
The professional should be directed to contact their
PHP immediately
Strong consideration should be given to suspension of
privileges until the PHP deems the professional safe to
practice again
This type of behavior usually results in a
comprehensive residential evaluation and treatment
Comprehensive Evaluation
Professional will be sent to a program that specializes in
evaluating disruptive professionals
Multidisciplinary evaluation lasting 1-5 days
Medical workup
Psychiatric/substance abuse evaluation
Psychosocial information including genogram
Neuropsychological testing
Collateral information
Comprehensive report results with recommendations by
evaluation team which may include
Outpatient treatment
Residential treatment
Long-term psychotherapy
360 evaluations
CME Program for Distressed
Physicians
Components:
Phone interview
Three-day CME course (47.5 AMA PRA Category 1
Credits ™)
Teach Specific tools/skills - e.g., grounding skills,
Alter, communication strategies
Three follow-up sessions with the core group over
the next six months; importance of group process
CME Course Goals
Teach specific skills related to preventing disruptive
behavior
Promote peer accountability and support
Identify risk factors and prevention strategies
Understand their own behavior and how it affects others
Discuss healthy boundaries and appropriate expression of
emotions
Understand socialization of professionals learned in training
that contributes to maladaptive patterns
This is NOT treatment, but rather education
Let’s practice
Flooding*
“ This means you feel so stressed that you become
emotionally and physically overwhelmed…”
“Pounding heart, sweaty hands, and shallow
breathing.”
“When you’re in this state of mind…you are not
capable of hearing new information or accepting
influence.”
*John M. Gottman, Ph.D. The Relationship Cure, Crown Publishers, New York, 2001, 74-78.
SELF-TEST: FLOODING
1.
At times, when I get angry I feel confused.
Yes No
2.
My discussions get far too heated.
Yes No
3.
I have a hard time calming down when I discuss disagreements.
Yes No
4.
I’m worried that I will say something I will regret.
Yes No
5.
I get far more upset than is necessary.
Yes No
6.
After a conflict I want to keep away or isolate for a while.
Yes No
7.
There’s no need to raise my voice the way I do in a discussion.
Yes No
8.
It really is overwhelming when a conflict gets going.
Yes No
9.
I can’t think straight when I get so negative.
Yes No
10.
I think, “Why can’t we talk things out logically?”
Yes No
John M. Gottman, All Rights Reserved (revised 11/17/03)
11.
My negative moods come out of nowhere.
Yes
No
12.
When my temper gets going there is no stopping it.
Yes
No
13.
I feel cold and empty after a conflict.
Yes
No
14.
When there is so much negativity I have difficulty focusing
my thoughts.
Yes
No
15.
Small issues suddenly become big ones for no apparent reason.
Yes
No
16.
I can never seem to soothe myself after a conflict.
Yes
No
17.
Sometimes I think that my moods are just crazy.
Yes
No
18.
Things get out of hand quickly in discussions.
Yes
No
19.
20.
My feelings are very easily hurt
When I get negative, stopping it is like trying to stop an
oncoming truck.
Yes
No
Yes
No
21.
My negativity drags me down.
Yes
No
22.
I feel disorganized by all this negative emotion.
Yes
No
23.
I can never tell when a blowup is going to happen.
Yes
No
24.
When I have a conflict it takes a very long time before I feel
at ease again.
Yes
No
Flooding - Scoring
Scoring: If you answered “yes” to more than eight statements, this is a strong
sign that you are prone to feeling flooded during conflict. Because this state can
be harmful to you, it’s important to let others know how you are feeling. The
antidote to flooding is to practice soothing yourself.
There are four secrets of soothing yourself: breathing, relaxation, heaviness, and
warmth. The first secret is to get control of your breathing. When you are getting
flooded, you will find yourself either holding your breath a lot or breathing
shallowly. Change your breathing so it is even and you take deep regular
breaths. Take your time inhaling and exhaling. The second secret is to find areas
of tension in your body and first tense and then relax these muscle groups. First,
examine your face, particularly your forehead and jaw, then your neck,
shoulders, arms, and back. Let the tension flow out and start feeling heavy. The
secret is to meditate, focusing your attention on one calming vision or idea. It
can be a very specific place you go to that was once a very comforting place, like
a forest or a beach. Imagine this place as vividly as you can as you calm yourself
down. The fourth part is to imagine the body part becoming warm.
John M. Gottman, All Rights Reserved (revised 11/17/03)
SKILLS TO USE WHEN
FLOODING
GROUNDING
Categories exercise
Judge versus describe
Mindfulness with all senses
Breathe
Role Play Exercise
Describe an incident you are concerned about.
Who was there?
Pick someone to play you.
A powerful cathartic exercise viewing their
behavior from multiple points of view.
Example.
ASSERTIVE COMMUNICATION
GUIDELINES
When asking for something, use the acronym
DRAN
Describe
Reinforce
Assert
Negotiate
Describe
Describe the other person’s behavior objectively
Use concrete terms
Describe a specified time, place & frequency of action
Describe the action, not the “motive”
Reinforce
Recognize the other person’s past efforts
Assert Directly & Specifically
Express your feelings
Express them calmly
State feelings in a positive manner
Direct yourself to the offending behavior, not the
entire person’s character
Ask explicitly for change in the other person’s
behavior
Negotiate: Work Towards A
Compromise That is Reasonable
Request a small change at first
Take into account whether the person can meet you
needs or goals
Specify behaviors you are willing to change
Make consequences explicit
Reward positive changes
Communication
The 8:1 Ratio
*John M. Gottman, Ph.D. The Relationship Cure, Crown Publishers, New York, 2001, 74-78.
B-29 Survey©
It is not enough to have good motives; others
respond to our behavior.
Physicians are often not given essential feedback
about their behavior.
The Team Behavior Survey (B-29) is designed to
provide feedback from those we work with.
© Swiggart, Williams, and Williams
Disruptive behavior
Social Systems
If the physician is returned to the institution to
practice, it is necessary to ensure that the behavior
does not recur.
There is a significant level of recidivism
As high as 20% among “severe offenders” (Grant and
Alfred 2007)
Prior behavioral issues are a significant risk factor for
later disruption (Papadakis, Arnold, et. al. 2008)
BW Williams to accompany a talk delivered at the FSPHP Spring Meeting 2010
Disruptive behavior
Social Systems
A monitoring system that measures these
issues using a 360◦ survey.
Early data show the survey to be valid.
The survey was developed to facilitate
integration with institutional systems.
BW Williams to accompany a talk delivered at the FSPHP Spring Meeting 2010
The Survey is Based on the Core
Competencies of the ACGME
Communication
Concern for patients and families
Accessibility and timeliness
Work environment
Ethical behavior
Interpersonal behavior & respect for others
System-based practice
Ability to work with other members of the
medical team
Potential Resources for Healthy
Coping
Courses
Coaches, counselors
Comprehensive
Evaluation
360° Evaluations
Risk Managers
Physician Wellness
Treatment Centers
Office of General Counsel
State BME
Professional Societies
QI Officers
EAP
Others
State Physician Health
Program
What we have learned?
There is a need to develop standard, model policies for
hospitals and medical practices
Medical student and resident training cultivates many of
the disruptive behaviors, as trainees learn from their
mentor’s behavior
Many physicians and other professionals come to training
“predisposed” to having problems
Information needs to be widely distributed to hospitals and
medical practices that this is treatable, saves money,
prevents malpractice suits, and that early intervention is
best
Disruptive behavior is a patient safety issue and needs to be
quickly addressed
Not all can be helped or saved
University of Florida and Vanderbilt
Center for Professional Health
Please visit our websites
http://drmarthabrown.com
http://www.mc.vanderbilt.edu
Additional resources can
be found on the website