Perform Dual Coding Analysis
advertisement

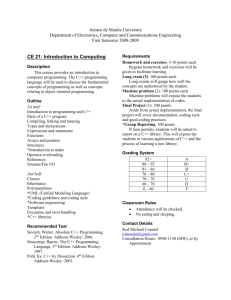
The Impact on Productivity in ICD-10-CM/PCS: Issues Found in the Current ICD-9-CM Environment at Montefiore Mazette H. Edwards, MA, CDIP, CCS, CPC-H, AHIMA ICD-10 Approved Trainer Disclaimer The information contained in this presentation is intended to be used for informational purposes only. It represents results based on studies conducted at Montefiore, in New York. Analyses are supported by findings of leaders and participants of conducted study. They are presented to exemplify the impact at Montefiore and should not be taken as confirmed results for all institutions. It is recommended that all institutions conduct their own studies tailored to suit their policies and needs. Individuals are encouraged to contact presenter if they have any questions about the information found in this presentation. Agenda • • • • • • • • • • Introduction and Objective Background Information: Montefiore ICD-10 Implementation Timeline Dual Coding vs. Duplicate Coding GEMs Tailored CDI Benefits of Dual/Duplicate Coding Game Takeaways Questions Overview • • • • Improve quality Decrease cost of healthcare. Preparation is key Montefiore has prioritized preparation for ICD-10CM/PCS since 2011 • Productivity when coding with ICD-10-CM/PCS • Methods Objective • To compare coding methods and the effect they will have on productivity; • To identify issues when coding discharges in ICD-10CM/PCS and the effects they will have on productivity and revenue; • To optimally resolve the issues and derive ways to improve the current environment for ICD-10-CM/PCS “Go Live” BACKGROUND INFORMATION Montefiore Montefiore To heal, to teach, to discover, to advance the health of the communities we serve • • • • • As the academic medical center and University Hospital for Albert Einstein College of Medicine, Montefiore is a 1,418 bed health system nationally recognized for clinical excellence - breaking new ground in research, training the next generation of healthcare leaders, and delivering sciencedriven, patient-centered care Epicenter of high quality patient care in the Bronx and surrounding areas in New York; provides healthcare services to more than two million people in the Bronx and Westchester County with 86,500 discharges; 12,939 outpatient surgeries; 830,000 outpatient visits and 301,000 Emergency Department visits Montefiore is ranked among the top hospitals nationally and regionally by U.S. News & World Report. For over 100 years Montefiore has been innovating new treatments, new procedures and new approaches to patient care, raising the bar for medical centers in the region and around the world Montefiore believes in providing coordinated, compassionate and leading-edge healthcare. Through highly integrated teams of physicians, nurses, social workers, mental health professionals and other caregivers, Montefiore pioneers a seamless system of care focused around the patient Montefiore is distinguished among premier academic medical centers for its deep commitment to the community Montefiore Transition from a hospital to a world renowned Health System Westchester Square Medical Office The Children’s Hospital at Montefiore (CHAM) North Division (Wakefield Hospital) Weiler Hospital Moses Hospital Mount Vernon Hospital New Rochelle Hospital Montefiore Health Information Management Department • • • • The Health Information Management Department (HIM) at Montefiore is responsible for operations and provision of services at all divisions, cancer registry operations, and registration data integrity and quality HIM Department is committed to providing accurate and timely health information that meets the clinical, administrative, and financial needs of the healthcare community, while maintaining the confidentiality of patients Transitioning from Hybrid to EHR • Medical record generated in a paper format • Paper record is sent to HIM for prepping, scanning, and indexing • Medical record uploaded to EPF for virtual availability to users through Montefiore network • Medical Audit Analyst review charts in EPF to code patients’ visits and submit query forms for any vague, unclear, or missing information. Utilizes Looking Glass (formerly eCHARMS) by Streamline for our abstracting system Impact On The Organization • • • ICD-10 will impact all sectors of healthcare Diagnostic and procedure codes are utilized from the start of healthcare services through the patient experience, from data creation to data use, and control reimbursement It is projected that there are significant costs and negative impact associated with ICD-10 transition – 10%-50% decrease in coder productivity – Fourfold increase in existing DNFB and A/R days for up to nine months postimplementation – Up to a 25% increase in re-works from claim rejections, adjustments and inquiries – $50 million to $250 million in productivity loss among physicians – Denial rates expected to increase 10% - 25% – Over-coding due to inexperienced coders will lead to a potential increase of 10% - 25% in RAC/MIC backlogs Evolution ICD-10-CM/PCS In 2011, Montefiore commenced training in the HIM Department in preparation for the ICD-10 transition 2011 Anatomy & Physiology detailed review Conducted by NYHIMA ICD-10-CMPCS series 2012 Pathophysiology detailed review in conjunction with CDI nurse managers •Specific diseases were targeted each month ICD-10-CM-PCS combination of: •3M educational modules •In-house ICD-10-CM/PCS trainer •9 hours per week in class training on: •New coding guidelines •New code set structure •Documentation required •Reinforcement of pathophysiology 2013 Coding in ICD-10-CM/PCS •Dual coding •Duplicate coding •Refresher on problematic areas: •Cardiovascular procedures •Pregnancy •Nervous system •Musculoskeletal system diagnoses and procedures ICD-10 NOW • Montefiore’s HIM Department began coding records with ICD-10 in mock trials, in December 2012 • Training and communication will continue throughout 2014 • The HIM Department at Montefiore hypothesizes that if the organization is thoroughly prepared for “Go Live,” the productivity of Medical Audit Analysts will not be severely affected, and the benefits of ICD-10 will overwhelmingly outweigh the negatives, if any METHOD Identifying the problems when coding with ICD-10-CM/PCS in the current environment Defining The “Method to our Madness” • Dual Coding – Medical Audit Analyst (MAA) assigns both ICD-9 and ICD-10 codes in a single coding session – MAA first assigns ICD-9 codes, then assigns ICD-10 codes in same setting • Duplicate Coding (variation of dual coding) – MAA codes discharge in ICD-9 – Another MAA codes same discharge in ICD-10 • Native Coding – Coding discharge utilizing usual procedure (abstracting, codebook etc.) • General Equivalent Mapping (GEMs) – Utilizing program to convert ICD-9 codes to ICD-10 Benefits and Goals • Benefits of Coding Analysis • Dual Coding / Duplicate Coding – Time to practice for ICD-10 – Actual revenue impact once change happens – Analyze data to pinpoint diagnoses with high risk for losses with inadequate documentation – Train physicians in what is needed to refrain from reimbursement loss – Identify need for additional coding resources – Full preparation for ICD-10 • To prevent current productivity loss due to using resources to code in ICD-10 – Hire consultant companies to currently code discharges Method I. Perform Dual Coding Analysis 1. Select 10 Medical Audit Analyst (MAA) to natively code current discharges with an average length of stay (LOS) of 7 days for Medicare and Medicaid patients in ICD-9-CM 2. The same group natively codes the same discharges in ICD10-CM/PCS 3. Each MAA is given 10 inpatient discharges to natively code in 7.5 hours, to maintain current average coding productivity Method II. Perform Duplicate Coding Analysis 1. Select 5 MAA to natively code current discharges with an average length of stay (LOS) of 7 days for Medicare and Medicaid patients in ICD-9-CM 2. Select another 5 MAA to natively code the same discharges in ICD-10-CM/PCS 3. Each coder is given 20 inpatient discharges to natively code in 7.5 hours, to maintain current average coding productivity RESULT INTERVENTION Number of Charts Coded Daily Montefiore Dual Coding Productivity Results • • 20 18 16 14 12 10 8 6 4 2 0 • • • 1 2 3 4 5 6 7 7 Month Trial Period Average # of charts expected to be coded according to average productivity (18 charts) Average # of charts actually coded in ICD-9 and ICD-10 • Dual Coding Analysis Due to decrease in productivity, dual coding method was terminated before the end of projected trial Increase in days in A/R DNFB not maintained Expected to code 18 cases in both ICD-9 and ICD-10 – 9 discharges in ICD-9; – 9 discharges in ICD-10 Actual average coded discharges: 6 total RESULT INTERVENTION Number of Charts Coded Daily Montefiore Duplicate Coding Productivity Results 18 16 14 12 10 8 6 4 2 0 Number of charts expected to be coded Number of charts coded in ICD-9 Number of charts coded in ICD-10 1 2 3 4 5 6 7 7 Month Trial Period Number of charts coded in ICD-10 Number of charts coded in ICD-9 Productivity in ICD-9 was maintained Decline in discharges coded in ICD-10 Number of charts expected to be coded Duplicate Coding Analysis • Inpatient coder productivity rates: – Currently codes 18.75 encounters per day in ICD-9-CM • Converts to a rate of 2.5 encounters per hour » 24 minutes to code each encounter – Inpatient coder in ICD-10-CM/PCS system • Currently codes 10 encounters per day – Converts to a rate of 1.3 encounters per hour » 46.2 minutes to code each encounter • Time to code same encounter doubled; resulted in decreased in productivity • Duplicate Coding method proved to be more productive however, than Dual Coding method. Method III. • Analyze Coding Productivity Utilizing GEMs 1. Select 5 MAA to natively code current discharges with an average length of stay (LOS) of 7 days for Medicare and Medicaid patients in ICD-9-CM 2. Select another 5 MAA to code the same charts in ICD-10CM/PCS utilizing electronic software for mapping. 3. Each coder is given 20 inpatient cases to code in 7.5 hours, to maintain current average coding productivity GEMs: Not a hidden “charm” • Inefficient way of learning the ICD-10 coding methodology • Compromise in quality • Takes time away from coding and transfers it to deciphering best code match based on chart documentation – Does not decrease amount of time necessary to code discharge in ICD-10 – Need to rescan and abstract charts for added information • Inaccuracies in code assignment • Revealed documentation issues Duplicate Coding Overall Results • Revealed issues in documentation that would negatively impact productivity and reimbursement • Cases unnecessarily difficult to code with ICD-10-PCS due to insufficient information • Site and laterality were key missing notes abstract – MRI’s, X-Rays and CT scans: no record of contrast medium – Injections and infusions: no record of administered site – Port-a-cath and vascular catheters: no specification of insertion site, no specification of artery or vein – Vague descriptions of physical and occupational therapy – CABG: no specification of which vein (greater or lesser, left or right) the graft comes from – Vague descriptions of fetal monitoring – PTCA: unclear about exact coronary artery sites angioplasties were performed on – Blood transfusions: Sparse information on kind of blood product, administration, autologous vs. non-autologous – Neoplasms: Laterality absent ANALYSIS Solution, Summary, Closing Eye-Opener, Pocket-Closer • Dual Coding – – – – Time consuming Coder abstracting and coding the same encounter twice Decrease in productivity Increase in days in A/R • Duplicate Coding Method more productive, less impact on reimbursement • Mapping utilizing duplicate coding did not improve productivity, repetitive process • Mapping utilizing dual coding would negatively impact reimbursement • Duplicate along with CAC may improve productivity in future • Documentation downfalls revealed for ICD-10 – Increase in Physician queries for ICD-10 Clinical Documentation Improvement • Major benefit of dual coding process is tailored CDI • Training is tailored for clinicians in respective specialties – Decrease amount of time dedicated to training – Shows benefit of specificity for reimbursement – Decrease in amount of records queried – Decreases hindrances on coder productivity – Elimination of ambiguous information • Physician documentation assessment • Enhance completed medical records with implementation of electronic health records • Holistic approach Benefits of Duplicate Coding Process • • • • • • • • Measure productivity impact Revenue reimbursement analysis Identify physician query opportunities Coder training Generating data for end-to-end testing Possibly improve documentation Impact Case Mix Index Increase in SOI and ROM scores Takeaways • Updating of policies and procedures ( Coding Department) • Continue to training and educational preparation • Documentation for both diagnoses and procedure codes • Looking at top 10 DRG's in ICD-9-CM • Looking at the top 10 diagnoses in ICD-9-CM Summary • The study performed allowed the HIM Department at Montefiore to unravel issues MAA face daily • Understanding from a primary perspective gives Montefiore outlook on efficient changes which should be beneficial to the implementation of ICD-10-CM/PCS • Upon completion of further training, and installation of upgraded technology, Montefiore plans to conduct another assessment to observe how the Coding Unit will perform with the proposed solutions • With the addition of Electronic Health Records (EHR), Computer Assisted Coding (CAC), further demo coding in ICD-10-CM/PCS, Montefiore feels confident in preparation for ICD-10-CM/PCS GO LIVE! Thank you! • • • • Mazette H. Edwards Director of Clinical Coding Practice 914-349-8144 maedward@montefiore.org References • http://ahima.org • http://www.cms.gov/Medicare/Coding/ICD10/Downloads/ICD10_Introduction_060413[1].pdf • http://www.cms.gov/Medicare/Coding/ICD10/Downloads/ICD10LargePracticesChecklistTimeline.p df • http://www.montefiore.org/ • http://streamlinehealth.net