Bipolar Disorder
advertisement

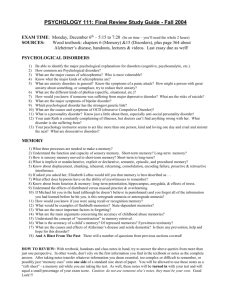
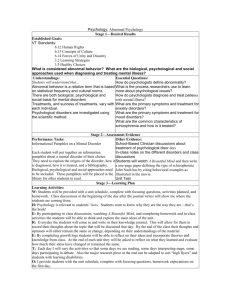
Psychopathology 8 December 2015 Overview of Mental Disorders • • • • • Conceptions and definitions Incidence, prevalence and causes Major categories Relationship to personality theories Closing thoughts Some Things to Consider… • Psychopathologies have biological/medical and psychological/experiential causes • Complexity of causes and symptoms complicates diagnoses and treatment • Perceptions and stigmatization can affect diagnosis and treatment seeking Mental Disorders Aren’t from Evil Spirits • Early theory: Possession mental disorders • Somatogenic hypothesis (bodily) – General paresis (Kraft-Ebing) • Syphilis delusions, depression, paralysis, and death • Psychogenic hypothesis (psychological) – Hysteria (Charcot; Freud; Breuer) • Paralysis or emotional fits with no neurological damage Modern Views: Diathesis-Stress Model • Diathesis – Predisposition (e.g., genetic) for disorder • Stress – Triggers disorder • Both diathesis (risk) and stress must be present for disorder Modern Views: Multicausal Models • Expands diathesis-stress models – Multiple diatheses • E.g., genetics, styles of thinking – Multiple stresses • E.g., relationship problems, victim of a crime • Biopsychosocial perspective – All three can contribute to mental disorders Diagnosis Guidelines: DSM-V DSM-IV-TR (2000-2012) DSM-V (2013-Present) • Previously, 5 major axes • Revised, nonaxial I. Clinical syndromes and disorders II. Personality disorders and mental retardation III. Medical conditions IV. Psychosocial and environmental stressors V. Global assessment of functioning – Biopsychosocial diagnosis and risk factors (Axes I-III) – Psychosocial and environmental stressors (Axis IV) – Disability (Axis V) • Better aligned with international standards (WHO, ICD) Mental Disorders are Functionally-Defined • Behavioral or psychological syndrome or pattern that occurs in a person and that is associated with present distress (e.g., a painful symptom) or disability (i.e., impairment in one or more important areas of functioning) or with a significantly increased risk of suffering death, pain, disability, or an important loss of freedom. In addition, this syndrome or pattern must not be merely an expectable and culturally sanctioned response to a particular event, for example, the death of a loved one. Whatever its original cause, it must currently be considered a manifestation of a behavioral, psychological, or biological dysfunction in the individual. – DSM-IV-TR (American Psychiatric Association, 2000) Functional Focus of Diagnosis • DSM focuses definitions of mental disorders on impaired function within social/cultural context – Biological/psychological symptoms of distress • E.g., chronic pain, hallucinations – Disability • E.g., motor impairment or learning deficits – Social/cultural context • E.g., Crying, fear, and anger are culturally universal emotional responses to death, but may be suppressed in Western cultures (Parkes, Laungani, & Young, 2003) Mental Illness Is a Major Social Issue • Each year, 1 in 5 American adults are or have been diagnosed with a mental illness • Not drug/alcohol-related • Does not include ADHD, autism spectrum disorder, schizophrenia or other psychotic disorders Risk of Mental Illness Is Widespread • Point prevalence – How many people live with a disorder at a given time • Lifetime prevalence – How many people will experience a given disorder at any point in life • Lifetime prevalence among US adults = 46% Assessing Mental Disorders • Assessment is critical for understanding reasons for symptoms and developing a treatment plan • 3 primary methods of assessment – Clinical interviews – Self-report measures – Projective tests Assessment: Clinical Interviews • Semistructured interview – Specific sequence of questions to identify certain diagnostic content • Symptoms – Patient report of physical or mental condition • Signs – Clinician’s observations of physical or mental condition Assessment: Self-Report Measures • Inventory of items to target symptoms or profile patients • Beck Depression Inventory – 21 items, specific to depression • Minnesota Multiphasic Personality Inventory (MMPI-2) – 567 items, broad profile of personality Methods of Assessment: Projective Tests • Projective test types – Thematic Apperception Test (TAT) – Rorschach (inkblot) Test • Meant to indirectly reveal unconscious wishes or conflicts • Though popular, weak correlations with mental health Thought Question… • Considering biopsychosocial factors… – Give one pro AND one con of labeling mental disorders… • Please, write your name and section on slips Section Time TA Name A 9:30 AM Josh C 11:30 AM Jing D 11:30 AM Matthew E 9:30 AM Sophie F 12:30 PM Sophie G 10:30 AM Josh H 1:30 PM Kevin I 1:30 PM Matthew J 2:30 PM Kevin L 3:30 PM Muhammad M 3:30 PM Charlotte N 6:30 PM Anna Major Categories of Mental Disorders • • • • Anxiety disorders Mood disorders Schizophrenia Other “Axis I & II” disorders Anxiety: Coping with Intense Emotions • Characterized by feelings of intense distress or worry • Disruptive and unsuccessful attempts at coping with those feelings Phobias = Fear + Avoidance • Specific phobias – E.g., acrophobia (heights), claustrophobia (enclosed places), arachnophobia (spiders) • Social phobia (social anxiety disorder) • Avoidance may exacerbate psychological or physical harm – E.g., more extreme avoidance of related fears, resorting to substance abuse dependence Panic Disorder As Physical Anxiety • Panic attacks – Sudden onset of terrifying bodily symptoms • • • • • • • • Labored breathing Choking Dizziness Tingling hands & feet Sweating Trembling Heart palpitations Chest pain Anxiety Can Be Continuous & Pervasive • Phobias need a stimulus • Panic attacks are not constant • Generalized Anxiety Disorder – Visibly worried nearly all the time – Anxiety is not specific to any stimulus – Physical symptoms (e.g., rapid heart rate, irregular breathing, sweating) can accompany psychological symptoms Obsessive-Compulsive Disorder (OCD) • Obsessions – Recurrent, unwanted or disturbing thoughts • Compulsions – Repetitive or ritualistic acts that may help cope with obsessions • OCD symptoms may defend against anxiety • “3 minutes in the mind of someone with OCD” Acute and Post-Traumatic Stress Disorders • Triggered abruptly by identifiable, horrific event • Dissociation – “Numbness” to traumatic event • Reactions include intense, intrusive recurrent nightmares and flashbacks • Affects women and men equally, with different causes – Women: rape or assault – Men: combat-related Specific Differences in PTSD • Major clusters of symptoms persist >1 month – Re-experience • Nightmares, flashbacks – Arousal • Difficulty sleeping, concentrating – Avoidance • Avoid anything related to trauma • 7% lifetime prevalence • More likely in women Roots of Anxiety • Predisposition is heritable – Meta-analysis of siblings – Identical twins have higher chance of having same diagnosis than fraternal twins or non-twins • Hettema, Neale, Kendler, 2011 • Anxiety can be conditioned – Classical (Pavlovian) – exposure to stimulus in context of fear or anxiety – Vicarious – observing another person’s anxiety Roots of Anxiety • Similar brain areas (amygdala, insula) are hyperactive (red) across phobias, social anxiety, and PTSD • Hypoactivation (blue) may be related to blunted affect in PTSD – Etkin & Wager, 2007 Mood: Persistent Ups and/or Downs • Depression – Extremely common lifetime prevalence • 1 in 4 women, 1 in 10 men – Global deficits or disruption in… • Affect (sadness, loss of pleasure) • Behavior (sleep, diet, bodily functions) • Cognition (attention, working memory) – Severe symptoms persist for > 2 weeks – Common in adolescence through middle adulthood, but not specific to any age in life Mood: Persistent Ups and/or Downs • Bipolar Disorder – Depressive & manic episodes (hours-months in duration) • Mania – racing thoughts and speech, irritability or euphoria, impaired judgment – Hypomania Mania Acute/Psychotic Mania • Short-lived periods, particularly insidious progression – Switching doesn’t always happen, but there can be mixed states (signs of both depression and mania) – Lifetime prevalence of 4%... Roots of Mood Disorders • High concordance rate – For bipolar disorder, 60% in twins (Kelsoe, 1997) • Neurotransmitter response and/or reuptake have complex, unclear effects on mood – Norepinephrine, dopamine, serotonin • Personal experiences, environment, and social/cultural factors can increase vulnerability to depression – Family/job problems; low SES neighborhood; social support structure; norms for expressing emotion Developing Vulnerability to Mood Disorders • Negative cognitive schema (Beck) – Automatic, negative interpretations about self, future, world • Explanatory style (Peterson & Seligman) – Internal, global, stable characterization of bad experiences • Since the above both predate depression, how might personality be involved? Schizophrenia: The “Split Mind” (Blueler) • Group of severe mental disorders – Disturbance of thought, withdrawal, inappropriate or flat emotions, delusions, hallucinations • Lifetime prevalence = 1% • Commonly diagnosed in adolescence or early adulthood; more often in men Signs and Symptoms of Schizophrenia • Positive or negative symptoms based on presence or absence in healthy people • Cognitive symptoms reflect impaired attention, working memory, inhibitory control, and even early sensory processing – Psychosis is a “cognitive break” from reality • Bizarre beliefs and perceptions Positive Symptoms of Schizophrenia • Not typically present in healthy individuals • Delusions – Systematized false beliefs of grandeur or persecution (delusions of reference) • Hallucinations – Sensory experience without actual external stimulation – Anderson Cooper tries a schizophrenia simulator • Disorganized behavior – Strangely dressed, violent or nonsensical behavior Negative Symptoms of Schizophrenia • Not typically absent or low in healthy individuals • Flat affect – Little to no display of emotion – Catatonic behavior • Anhedonia – No interest in pleasurable activities • Withdrawal – Isolation from social interactions – Development of idiosyncratic thoughts and behavior Genetics & Development in Schizophrenia • Risk increases with closer relations • Potential developmental risk factors – Influenza exposure • Brown et al., 2001 – Maternal malnutrition • St. Clair et al, 2005 – Oxygen deprivation • Cannon et al., 2000 Neural Bases of Schizophrenia • Dopamine Hypothesis – Oversensitivity to dopamine – Classic antipsychotics block dopaminergic signaling – Amphetamines increase dopamine activity schizophrenia-like symptoms Neural Bases of Schizophrenia • Enlarged ventricles – Decreased white and gray matter volume – Shenton et al., 2001 • Decreased gray matter in prefrontal cortex – Impaired executive control Poverty: Diathesis & Stress in Schizophrenia • Prevalence in Chicago (19221934) – Low SES closer to center High incidence – High SES moving outward Low incidence • Poverty increases vulnerability to schizophrenia, schizophrenia increases vulnerability to poverty Overview of Other “Axis I & II” Disorders • • • • Developmental Eating Dissociative Personality Developmental Disorders • Autism – Language deficits: late onset, pronoun difficulties – Motor impairments: peculiar repetitive actions – Apparently have little understanding of or interest in other people’s emotions or goals • Attentiondeficit/hyperactivity disorder (ADHD) – Impulsivity, attentional deficits, behavioral problems – Controversy in diagnosis – Development of prefrontal cortex is implicated Eating Disorders • Either may arise from genetic factors, as well as sociocultural norms of attractiveness • Anorexia nervosa – Appear underweight – Preoccupation with food, eating, gaining weight – Incredibly strict dieting and/or exercise; purging • Bulimia nervosa – Appear “normal” weight – Binging and compensatory behavior Dissociative Disorders • Psychological distancing to cope with ongoing traumatic or distressing events – Dissociative amnesia • Sudden inability to remember a period of life – Dissociative fugue • Wandering from home for extended period of time – Dissociative identity disorder (DID) • Creation of “multiple personalities” Personality Disorders • Some aspects of different personality dimensions can be socially or culturally maladaptive • The associated maladaptive behaviors and cognitions can lead to distress or impairments • Since personality is relatively stable within an individual and across time, such issues can then be pervasive and persistent 10 Types of Personality Disorders • Paranoid • – Mistrust of others • Schizoid – Detachment from others • • Antisocial – Disregard & violation of other’s rights • – Excessive attention-seeking and emotionality • Borderline – Impulsive behavior; unstable relationships, self-concept, affect Narcissistic – Grandiose, lacks empathy, attentionand validation-seeking Schizotypal – Discomfort with relationships; cognitive & perceptual distortions; odd behavior Histrionic • Avoidant – Social inhibition & insecurity • Dependent – Excessive need to be cared for • Obsessive-Compulsive – Preoccupation with order, cleanliness, and control Take Home Messages • There is a high prevalence of mental illness • Mental illnesses have biological, psychological, and social underpinnings • Social factors can influence illnesses and their characterization/stigmatization • Complexity of mental illnesses (e.g., symptoms, signs, comorbidity) make diagnosis and treatment extremely challenging Some Thoughts before We Cover Treatment • 1 in 5 people you see may live with a mental illness… – Consider how biological, psychological, and social factors influence our perceptions of people who live with mental illness – How do these factors guide our assessment and treatment? – How do these factors help or hinder the decision to seek treatment? • Be compassionate!!! – Even though you see people every day, you may never know what it’s like live a day in their mind…