Palliative Care: Back to Basics
advertisement

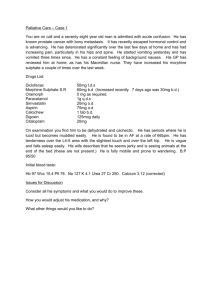
Palliative Care: Back to Basics Dr Shirley H. Bush Assistant Professor, Division of Palliative Care, Department of Medicine March 18, 2015 • You may only access and use this PowerPoint presentation for educational purposes. • You may not post this presentation online or distribute it without the permission of the author. [Back to Basics– Palliative Care – Dr. Shirley Bush] Luke Fildes: The Doctor 1891 Oil on canvas, © Tate (tate.org.uk) Overview of Session • Knowledge Quiz • In-class discussion of answers • Palliative Care overview – Starting opioids – Management of nausea and vomiting • End of life (EOL) care – For MCC objectives “The Dying Patient” • Resources on One45 – Guidelines for Opioids: Opioid Equivalency tables • Don’t forget: The Pallium Palliative Pocketbook from Integration Unit [Back to Basics– Palliative Care – Dr. Shirley Bush] Pallium Palliative e-Book • https://itunes.apple.com/ca/book/palliumpalliative-e-book/id901889273?mt=11 • http://www.amazon.ca/Pallium-PalliativeBook-Jos%C3%A9-Pereiraebook/dp/B00LH2D5WK MCC Objectives – The Dying Patient • http://apps.mcc.ca/Objectives_Online/objectives.pl?lang=englis h&role=expert&id=25 • Key Objectives: • Given a dying patient, the candidate will formulate an appropriate palliative care plan that ensures optimal control of pain and other symptoms, maintenance of human dignity, and recognize the important role of family and social support. [Back to Basics– Palliative Care – Dr. Shirley Bush] MCC Objectives – The Dying Patient • Enabling Objectives: • Given a dying patient, the candidate will construct an effective management plan, including: a) discussion at the appropriate time with the patient as to his wishes for care (e.g., resuscitation) b) determining whether an advanced directive or substitute decision-maker exists, if the patient is unable to express his wishes c) the use of pharmacotherapy (e.g., analgesia) for symptom control, recognizing appropriate indications, side effects, and complications [Back to Basics– Palliative Care – Dr. Shirley Bush] MCC Objectives – The Dying Patient • Enabling Objectives CONTD: • Given a dying patient, the candidate will construct an effective management plan, including: d) ensuring culturally sensitive emotional, physical, and spiritual support to the patient and family, as appropriate e) appropriate involvement of the healthcare team f) referral to other health care professionals, as needed [Back to Basics– Palliative Care – Dr. Shirley Bush] MCC Objectives – Miscellaneous • Vomiting and/or nausea: • http://apps.mcc.ca/Objectives_Online/objectives.pl?lang=englis h&role=expert&id=116 • Delirium: (Dr. Barbara Power: March 30, 2015/ Delirium SLM, Palliative Care week of Integration Unit) • http://apps.mcc.ca/Objectives_Online/objectives.pl?lang=englis h&role=expert&id=58-2 • Truth Telling: (Integration Unit: Communication) • http://apps.mcc.ca/Objectives_Online/objectives.pl?lang=englis h&role=expert&id=121-2 [Back to Basics– Palliative Care – Dr. Shirley Bush] B2B Session Objectives - I • At the end of this session, students will be able to: • Describe models of hospice palliative care and the principles on which these are based. • Discuss interprofessional collaboration in palliative and end-oflife care as a fundamental concept. • Identify “total pain” incorporating the roles that psychological, social, emotional and spiritual concerns, along with physical symptoms, play in producing the pain experience. • Identify the components of a holistic, interprofessional (IP) assessment and plan of care for a terminally ill patient. [Back to Basics– Palliative Care – Dr. Shirley Bush] B2B Session Objectives - II • Complete a ‘worked example’ for prescribing opioids in an opioid naïve patient, and for opioid rotation. • Outline the management of nausea and vomiting in advanced cancer patients. • • • • Describe 3 illness trajectories. Identify signs of approaching death. Describe common signs of the natural dying process. Describe preparing the patient, family and caregivers, when death approaches. • Describe the pharmacological and non-pharmacological management of patients at the end of life. [Back to Basics– Palliative Care – Dr. Shirley Bush] Palliative Care Knowledge Quiz • Test your own knowledge: [Back to Basics– Palliative Care – Dr. Shirley Bush] Question 1 • Mrs. X is taking Long-Acting Morphine tablets 30 mg by mouth every 12 hours for her pain, which has been well controlled. • She is now dying, and unable to take anything by mouth. • The appropriate change in medication should be: – – – – (a) 10 mg subQ q4h (b) 5 mg subQ q4h (c) 5-10 mg subQ q4h prn only (d) crush the tablets, dissolve them in water, and administer same medications buccally – (e) 30 mg subQ q12 hours [Back to Basics– Palliative Care – Dr. Shirley Bush] Question 2 • The dose conversion ratio of morphine to oxycodone in the setting of palliative care is: (a) 10 mg po of morphine = approximately 5-7.5 mg po of oxycodone (b) 10 mg po of morphine = approximately 15 mg po of oxycodone (c) 10 mg po of morphine = approximately 20 mg po of oxycodone (d) 10 mg po of morphine = approximately 10 mg po of oxycodone (e) 10 mg po of morphine = approximately 1 mg po of oxycodone [Back to Basics– Palliative Care – Dr. Shirley Bush] Question 3 • A 55-year-old, 60-kg cancer patient with severe pain (8/10) related to metastatic bone disease is in need of a strong opioid. You decide to initiate him on a morphine regimen. He has not previously been on a strong opioid and has normal renal function. What starting dose would you use? (a) Morphine (long acting formulation) 30 mg orally twice a day and morphine (short-acting formulation) 5 mg orally every hour as needed (prn) for breakthrough pain. (b) Morphine (short-acting) 5-20 mg orally every 4 hours and morphine 5 mg orally every hour as needed (prn) for breakthrough pain. (c) Morphine (short-acting) 5 mg orally every 4 hours and 5 mg orally every hour as needed (prn) for breakthrough pain (d) Morphine (short-acting) 5 mg orally every hour as needed (prn) for pain. (e) Morphine (short-acting) 5mg orally four times a day and 5mg orally as needed (prn) for breakthrough pain. [Back to Basics– Palliative Care – Dr. Shirley Bush] Question 4 • Which one of the following opioids is not recommended for chronic pain management in palliative patients? (a) Meperidine (Demerol) (b) Codeine (c) Methadone (d) Oxycodone (e) Fentanyl [Back to Basics– Palliative Care – Dr. Shirley Bush] Question 5 • A 67 year-old man with advanced lung cancer and bone metastases is taking slow release morphine 90 mg orally q12h. In the last two days he has complained of increased generalized pain and his family have noticed that he has become agitated, developed generalized myoclonus (muscles twitching) and has started “picking at the air”. • Which one of the following is the most appropriate change to make to his opioid regimen? (a) Switch his morphine to short acting hydromorphone at a dose of 8 mg orally q4h (b) Switch his morphine to short acting hydromorphone at a dose of 4 mg orally q4h (c) Increase the morphine dose to 120mg orally twice a day. (d) Switch his opioid to transdermal fentanyl at a dose of 25 micrograms/hr every 3 days. (e) Continue the morphine at the current dose and add baclofen to control the muscle twitches. [Back to Basics– Palliative Care – Dr. Shirley Bush] Question 6 • A 48 year-old man with advanced cancer presents with delirium. He has cognitive impairment, mild agitation and disturbing visual hallucinations. While searching for the underlying causes, which one of the following treatments would you initiate to control his delirium-related problems? (a) Haloperidol 1mg orally q8hrs and haloperidol 1mg every hour if needed. (b) Diazepam 5 mg to 10 mg orally twice a day and 5mg every hour if needed. (c) Lorazepam 2mg orally or sublingually three times a day and 1mg every hour if needed. (d) Methotrimeprazine 12.5mg orally q12hrs and 12.5mg every hour if needed. (e) Midazolam: a bolus dose of 2.5mg subcutaneously followed by a continuous infusion of 1mg to 4mg/hour titrated to control his agitation. [Back to Basics– Palliative Care – Dr. Shirley Bush] Question 7 • Joe D. is a 73 year old man who was prescribed an opioid for severe pain, due to metastatic prostate cancer, 2 days ago. The medication has made him feel very nauseated. The most appropriate first-line antiemetic which has its main effect on the chemoreceptor trigger zone is: (a) Dimenhydrinate (Gravol) (b) Metoclopramide (Maxeran) (c) Ondansetron (Zofran) (d) Cannibinoid derivative (Marinol or Cesamet) (e) Prochlorprazine (Stemetil) [Back to Basics– Palliative Care – Dr. Shirley Bush] Question 8 • The presence of dyspnea in a terminally ill patient is best determined by: (a) A patient expressing that he is short of breath, without any other objective measures. (b) A patient expressing that he is short of breath, PLUS the use of accessory breathing muscles. (c) A patient expressing that he is short of breath, PLUS tachypnea (d) A patient expressing that he is short of breath, PLUS hypoxia or hypercarbia (e) The presence of the use of accessory breathing muscles and tachypnea. [Back to Basics– Palliative Care – Dr. Shirley Bush] Question 9 • A 68 year old man with progressive amyotrophic lateral sclerosis (ALS) presents with increasing weakness and shortness of breath, even at rest. He has no symptoms or signs to suggest a pneumonia. Which one of the following would be the most appropriate first-line symptomatic management of his dyspnea at this time? (a) Morphine 5mg nebulized (via an airway mask) every 4 hrs and every hour as needed (prn). (b) Morphine 5mg orally every 4 hrs and 5mg orally every hour as needed for dyspnea. (c) Lorazepam 1mg orally or sublingually three times a day. (d) Non-invasive airway support with BIPAP. (e) Tracheostomy with artificial ventilation. [Back to Basics– Palliative Care – Dr. Shirley Bush] Question 10 • You have just written a prescription for hydromorphone (Dilaudid) for a patient. You must also write a prescription for a laxative. The best choice is: (a) a stool softener, such as docusate sodium (b) an enema, if needed (c) a bowel stimulant e.g. senna derivatives or an osmotic agent (d) a glycerine suppository (e) methylnaltrexone [Back to Basics– Palliative Care – Dr. Shirley Bush] WHO Definition of Palliative Care - 2005 • “Palliative Care - an approach that improves QOL of patients and their families facing the problem associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable Assessment and Treatment of pain and other problems, physical, psychosocial and spiritual”. • http://www.who.int/cancer/palliative/definition/en/ • (Page not available in French) [Back to Basics– Palliative Care – Dr. Shirley Bush] • Effective palliative care requires a broad multidisciplinary and interprofessional approach that includes the family and makes use of available community resources • It can be successfully implemented even if resources are limited [Back to Basics– Palliative Care – Dr. Shirley Bush] CHPCA Models of Palliative Care (2002) • Model • Realistically Bereavement Care Bereavement Care Therapy to cure or control disease Therapy to cure or control disease Palliative approach to care Palliative approach to care Illness Trajectory Illness trajectory Dx Dx Death [ Death Aspects/Domains of Holistic Care Physical, e.g. Psychological, e.g. -Disease management -Pain & other symptoms -Function -Nutrition habits -Physical activity -Personality -Psychological symptoms -Emotions -Control & dignity -Coping responses -Self image/ self esteem -Loss & Grief Social/Cultural, e.g. Spiritual, e.g. -Meaning & values -Existential issues -Beliefs -Spirituality -Rites & rituals -Symbols & icons -Loss & Grief -Life transitions -Religions -Finances -Relationships -Personal routines -Recreation -Vocation -Rituals -Legal issues -Family caregiver support -Practical ] Adapted from: “Domains of Issues Associated with Illness and Bereavement” in A Model to Guide Hospice Palliative Care: Based on National Principles and Norms of Practice. CHPCA, March 2002, page 15. Interprofessional (IP) Team Work • Patients and families are experiencing a variety of needs representing the different facets of their reality. • In order to meet these needs which are often complex, the perspectives, skills and resources of a variety of professionals are required. – Physician collaborates with……. • • • • • • • • • • Nurse (RN, RPN, APN, PCA – Personal Care Assistant) Dietician/ Speech Language Pathologist (SLP) Pharmacist Physiotherapist/ Occupational therapist (PT/OT) Psychologist Recreation therapist Social worker Spiritual care professional/ Chaplain Volunteer Patient and family [Back to Basics– Palliative Care – Dr. Shirley Bush] Medical Care of the Dying, 4th ed. Victoria Hospice Society; 2006 Conceptual Model of level of need within the population of patients with a life limiting illness A Guide to Palliative Care Service Development: a population based approach . PCA 2005. Available at: http://www.palliativecare.org.au [Back to Basics– Palliative Care – Dr. Shirley Bush] Episode of Care scenarios to meet Palliative Care needs A Guide to Palliative Care Service Development: a population based approach . Palliative Care Australia (PCA) 2005. Available at: http://www.palliativecare.org.au [Back to Basics– Palliative Care – Dr. Shirley Bush] W.H.O. 3-step Analgesic Ladder Opioid for mild to moderate pain Non-opioid e.g. paracetamol, NSAIDs +/– Adjuvant STEP 1 [Back to Basics– Palliative Care – Dr. Shirley Bush] +/– Non-opioid +/– Adjuvant Opioid for moderate to severe pain +/– Non-opioid +/– Adjuvant STEP 3 STEP 2 Pain persisting or increasing W.H.O. Analgesic “Ladder” • Promoted 3 important concepts world-wide: • By Mouth • By the Clock • By the Ladder • N.B. not designed for use in isolation • Is there still a role for Step 2? [Back to Basics– Palliative Care – Dr. Shirley Bush] Initiating Opioids: “Worked example” • Bernard is a 65 year old retired policeman who was diagnosed with colon cancer 18 months ago. • After surgery, his disease initially responded to chemotherapy, but has now recurred with metastases to the liver and peritoneum. • He is experiencing increasing abdominal pain. • He rates the pain as 6/10. • He has been taking extra strength acetaminophen (1 to 2 tablets 3 to 4 times a day) with minimal effect. • Q: Bernard has moderate to severe nociceptive pain: • What opioid would you choose, and why? What starting dose? [Back to Basics– Palliative Care – Dr. Shirley Bush] “Worked example”: Answers • Bernard is opioid naïve. • Suggested starting doses: – Morphine (IR) 5mg po q4hrs straight + 2.5 or 5mg po q1-2hr prn as ‘rescue’ dose/for breakthrough pain – Hydromorphone (IR) 1mg po q4hrs straight + 0.5 or 1mg po q1-2hr prn • For ‘rescue’ dose: – Generally, it is 10% of total daily dose. – It should be titrated, so could be anything between 5-20% of total daily dose if needed. – If patient needs 3 or more ‘rescue’ doses/24 hours, the regular opioid dose should be increased (assuming opioid-responsive pain) [Back to Basics– Palliative Care – Dr. Shirley Bush] Commencing Opioids Common starting dose Starting dose in frail, weak patients or patients with severe COPD Morphine 5 – 10mg PO q4H straight 2.5 – 5mg PO q4H straight Hydromorphone 1– 2mg PO q4H straight 0.5 – 1mg PO q4H straight Oxycodone 2.5 – 5mg PO q4H straight 1 – 2.5mg PO q4H straight (1) Discuss Opioid fears and misapprehension with patient: ‘Morphine Myths’ (2) Do also prescribe a ‘Rescue ‘ dose of IR (Immediate release) opioid for ‘breakthrough’ or ‘episodic’ pain: 10% of total daily dose (3) Also see OPIOID EQUIVALENCY tables: on One45 [Back to Basics– Palliative Care – Dr. Shirley Bush] When Commencing Opioids: Manage Potential Side Effects • Discuss potential side effects and strategies with patients • Constipation: occurs in majority of patients and does not resolve spontaneously – Regular laxative e.g. senna, lactulose • Nausea: in up to 2/3 of patients, but usually subsides within 3-7 days – Antiemetic e.g. metoclopramide, haloperidol • Somnolence/ Sedation: usually temporary for a few days – Advise patient not to drive following opioid initiation, opioid switch, significant dose increase for at least 5-7 days, or if uncontrolled pain • Respiratory depression (RR less than 8/min): • Extremely low risk if appropriate starting dose and appropriate titration [Back to Basics– Palliative Care – Dr. Shirley Bush] Bernard: “Worked example” continued • Q: How would you titrate the opioid dose up, if Bernard’s pain remains poorly controlled? • Method 1: Increase the dose by 20-30% • Method 2: – Add up the # of ‘rescue’ doses used in previous 24 hours – Add these to the total dose of regularly scheduled doses over last 24 hour period – Now divide this total by 6 to get the new 4-hourly dose • Q: Bernard still has pain despite Morphine 10mg po q4hr plus 4-5 PRN doses of 5mg/day: What morphine dose would you prescribe now? • Morphine 15mg po q4hrs straight • Don’t forget to increase ‘rescue’ dose too [Back to Basics– Palliative Care – Dr. Shirley Bush] Bernard: “Worked example” continued • 2 weeks later, Bernard’s pain is under good control (2/10). He is now on Morphine (IR) 20mg po q4hrs straight, and taking only 1 -2 ‘rescue’ doses a day. He finds the q4hr regimen inconvenient. • Q: What dose of slow release morphine would you start? • Slow release Morphine 60mg po q12hrs • And continue IR Morphine for breakthrough pain [Back to Basics– Palliative Care – Dr. Shirley Bush] Bernard: “Worked example” continued • Bernard’s disease progresses. He is managing at home with his wife, family, and community team (Family physician and home care nursing). He now develops vomiting from a bowel obstruction. • Q: How will you control his pain now that the oral route is no longer working? • Change to subcutaneous route. • Generally, the po: subcut conversion dose for both Morphine and Hydromorphone is 2:1 • Morphine SR 60mg po q12hrs = Morphine 120mg po/24 hours • = Morphine 60mg subcut/24hrs = 10mg subcut q4hr straight • Add subcut option for breakthrough pain (Morphine 5mg subcut q1hr prn) [Back to Basics– Palliative Care – Dr. Shirley Bush] Opioid-Induced Neurotoxicity (OIN) Therefore we may give more Agitation often Interpreted as increasing pain Opioids Dehydration (decrease po. Intake…) leading to progressive renal failure OIN – delirium, agitation, +/hyperalgesia Accumulation of Opioid metabolites Alice: Opioid Rotation Question • Alice: 73 y.o. metastatic breast cancer • Lives with frail husband @home, regular CCAC and GP visits • PPS (Palliative Performance Scale) 50% • PPS 50% = mainly sit/lie, requires considerable assistance • Increased pain++ Right hip • Morphine dose increased from 60mg subcut/24h to 120mg subcut/24h within the last 7 days…. – Alice is somnolent – Her husband says she has been confused – Mild myoclonus of both legs observed • You, as her visiting MD, are concerned that she is opioid toxic. • How would you rotate her to hydromorphone? [Back to Basics– Palliative Care – Dr. Shirley Bush] Alice: Opioid Rotation Answer • For opioid rotation Morphine (M) → Hydromorphone (HM) • 10mg subcut M = 2mg subcut HM (i.e. 5:1) – See Guidelines for Opioids: Opioid Equivalency tables on One 45 • So 120mg M subcut/24h = 120/5 = 24mg HM subcut/24h • BUT: equianalgesic dose of the new opioid should be reduced by 30-50% because of incomplete cross tolerance • 30% of 24mg HM subcut/24h = 7.2mg • Thus, suggested final dose = 24-7= 17mg HM subcut/24h • Also: – – – – Review other medications, especially other psychoactive drugs Consider hydration ? Role for non-opioid co-analgesic/adjuvant Imaging R hip: ? Role for palliative RADS [Back to Basics– Palliative Care – Dr. Shirley Bush] [Back to Basics– Palliative Care – Dr. Shirley Bush] Multi-factorial Causes of Nausea and Vomiting in patients with advanced cancer Gastric outlet obstruction / intestinal obstruction Severe constipation Autonomic failure / delayed gastric emptying Gastroesophageal reflux disease / gastritis / peptic ulcer disease / gastric compression / ‘squashed stomach syndrome’/ gross ascites Drugs e.g. opioids, antibiotics, digoxin Psychological factors / anxiety / anticipatory (conditioned) Metabolic disorders e.g. hypercalcemia, hyponatremia, liver failure, renal failure Nausea and Vomiting Oral / esophageal infection or lesions, esophagitis Toxins e.g. sepsis, urinary tract infection, tumor produced peptides Chemotherapy / Radiotherapy Vestibular stimulation e.g. motion sickness, Menières, labyrinthitis, base of skull disease Raised intracranial pressure e.g. brain tumor or metastasis, leptomeningeal disease [Back to Basics– Palliative Care – Dr. Shirley Bush] Common Causes of Nausea & Vomiting in Advanced Cancer [Back to Basics– Palliative Care – Dr. Shirley Bush] Major Emetogenic Pathways Pain, anxiety,ICP, anticipatory (pre-CT) e.g. lorazepam dexamethasone Shirley Bush 2014 Motion e.g. dimenhydrinate (Gravol) H1 _ Achm + + CTZ D2 5HT3 Drugs, biochemical disorders, toxins via systemic circulation e.g haloperidol, (metoclopramide) (prochlorperazine action at Vestibular input, CTZ and Vomiting Centre) + Vestibular input + + Higher cerebral centres Vomiting Centre H1 Achm 5HT3 5HT2 e.g. dimenhydrinate (Gravol) + VAGUS Effector organs Liver Gut D2 5HT3 5HT4 Ach G.I. Distension, obstruction, liver mets. e.g. metoclopramide domperidone Methotrimeprazine (Nozinan) • A more sedating phenothiazine than prochlorperazine (Stemetil) • Long T ½ • Used in palliative care as anti-emetic and for agitated delirium • (Like Stemetil) Broad receptor coverage • D2, H1, Ach, 1 adrenoreceptors, 5HT2 • CTZ antagonist, Vomiting centre, Vestibular system and gut • Also adjuvant analgesic effect • NB: Many anti-emetics – Extrapyramidal adverse effects – QTc prolongation [Back to Basics– Palliative Care – Dr. Shirley Bush] Anatomical Reflex Pathways We have N & V as protective mechanisms Sight, smell, taste: To detect contaminated food stuffs Receptors in upper gut detect toxins E.g. Vagus from gut (Peripheral Dopamine D2 receptors) Also gut Acetylcholine (Ach) receptors And gut Serotonin (5HT3) receptors 5HT3 receptors Via gut 5HT3 (serotonin) receptors Serotonin located in enterochromaffin cells in gut wall Released and metabolised locally in response to various insults, including radiotherapy with gut in field and highly emetogenic chemotherapy (N.B. also 5HT3 receptors in V.C. (and CTZ) Major N & V Pathways - 1 VAGUS from gut (Peripheral Dopamine D2 receptors) CTZ = Chemoreceptor Trigger Zone Area Postrema in floor of 4th ventricle in medulla Effectively NO blood brain barrier Capillaries of AP – leaky fenestrated endothelium, permitting direct chemical communication between blood and subarachnoid CSF So sensitive to CHEMICAL stimulation from blood/ CSF Principal central receptors - Dopamine D2, (also 5HT3) (Vagal afferents from gut also project to CTZ) Major N & V Pathways - 2 Impulses from CTZ to VC Sensory information processed in tractus solitarius and its nucleus (and vomiting initiated by dorsal motor nucleus of the vagus and nucleus ambiguus) CTZ may also send outputs directly to VC efferent components Major N & V Pathways - 3 VC = Integrated Vomiting Centres Neuroanatomical region Adjacent co-ordinated sites in lateral reticular formation of the medulla Also receives afferents from GIT, thorax, vestibular system, thalamus, higher brain stem and cerebral cortex Consists of: Nucleus tractus solitarius Main efferent motor components of VC Dorsal motor nucleus of vagus & nucleus ambiguus Major N & V Pathways - 4 Integration of emetogenic stimuli with parasympathetic activity and Stimulation of these motor efferent pathways from VC vomiting Principal receptors are: Histamine H1 Muscarinic cholinergic Achm Serotonin 5HT3 + others, e.g. 5HT2 Major N & V Pathways - 5 Vestibular system (via Achm / H1 receptors) Motion sickness, Meniere’s disease, labyrinthitis Malignant infiltration of vestibular apparatus E.g. acoustic neuroma, 10 and 20 cerebral tumours, base of skull disease Drugs e.g. platinum, aspirin Major N & V Pathways - 6 Via Cortical Centres Effect of memories on sensitising the whole process Anticipatory N & V pre chemotherapy Raised ICP E.g. 10 and 20 CNS tumour E.g. meningitis (carcinomatous, chemical, infection) Psychological factors, anxiety N & V: Non-Pharmacological Management • Assist patient to sit upright in bed, or out of bed, for meals • Encourage family to bring in foods that patient likes and can tolerate • Try easily digested foods (add sauces) • Small attractive meals, little and often • Refer to dietician to increase food choices • Flat ginger ale • At home, avoid smell of cooking food [Back to Basics– Palliative Care – Dr. Shirley Bush] Non-Drug Management for N & V • Acupuncture / acupressure wrist bands (Sea Bands™) • Anxiety management • Behavioural therapy with systematic desensitization – anticipatory emesis with chemotherapy [Back to Basics– Palliative Care – Dr. Shirley Bush] – P6 (Neiguan) acupuncture point = midline of palmar aspect of wrist, about 3cm from palmar crease – Acupuncture point stimulation acute CINV – Acupressure may acute nausea – Ezzo JM et al. Acupuncture-point stimulation for chemotherapy-induced nausea or vomiting; Cochrane 2006 Illness Trajectories [Back to Basics– Palliative Care – Dr. Shirley Bush] Murray SA , et al. BMJ 2008;336:958-9 3 Triggers for Palliative/ Supportive Care • (1) The ‘Surprise’ Question: – Would you be surprised if this patient were to die in the next 6 - 12 months? • (2) Choice/Need • (3) Clinical indicators: Specific indicators of advanced disease for each of the 3 main EOL patient groups • Prognostic Indicator Guidance from the Gold Standards Framework ™ • Available @ • www.goldstandardsframework.org.uk [Back to Basics– Palliative Care – Dr. Shirley Bush] Prognosis: “Doctor: How long do I have to live?” • How frequently is the patient observed to decline? The Thinker, Auguste Rodin, 1902 – Every Month: estimated prognosis of months – Every Week: estimated prognosis of weeks – Every Day: estimated prognosis of days – Every Hour: estimated prognosis of hours BUT with caveat: in setting of advanced cancer, patient’s condition can change very quickly (Another disclaimer: life expectancy can be longer) [Back to Basics– Palliative Care – Dr. Shirley Bush] See Chapter 4 in Pallium Palliative Pocketbook Goals of Care • Establish patient’s Goals of Care • Assess the patient and/or family’s knowledge of the illness and prognosis • Assess priorities – Comfort – Allow a Natural Death – Life-prolongation – Special events • Communication: Is everyone on the same page? – Role for Family Meeting • Detailed documentation, including ‘level of care’, code status [Back to Basics– Palliative Care – Dr. Shirley Bush] See Chapter 3 in Pallium Palliative Pocketbook The Normal Dying Process - The Last Days • • • • • • • Weaker: need assistance with all care Bed-bound Reduced oral intake - food/ fluids Difficulty swallowing oral medications Drowsy or reduced cognition and difficulty concentrating More time asleep Some symptoms may increase e.g. delirium, dyspnea • “Withdraw” - say their goodbyes [Back to Basics– Palliative Care – Dr. Shirley Bush] Signs that Death is Imminent: “days to hours” • Explain these signs to the family and other caregivers: • CNS: Refractory delirium (in up to 88% of patients @ EOL), (N.B. exclude reversible causes e.g. urine retention, opioid toxicity), Reduced consciousness • RESP: Rate, pattern – Altered breathing • Cheyne-Stokes respiration • Periods of apnea • Agonal breathing – Profuse upper airway secretions – “terminal respiratory congestion” or “death rattle” • CVS: Weak and rapid pulse, decreased capillary refill • SKIN: Cold extremities, mottling of periphery (hands, feet, legs) • GU/GI: Reduced output [Back to Basics– Palliative Care – Dr. Shirley Bush] Terminal Respiratory Congestion: “Death Rattle” • • • • Inability to clear secretions from oropharynx and trachea Relaxation of pharynx Noisy “rattling” respiration Patients usually unconscious/ semi-conscious and too weak to expectorate – likely not distressing to patient – Explain to and reassure family • Nursing care – – – – Nurse semi-prone Nurse side to side Maintain scrupulous oral hygiene Suction rarely required • Light oral suctioning may be needed – avoid deep suctioning [Back to Basics– Palliative Care – Dr. Shirley Bush] Terminal Respiratory Congestion Management contd. • Discontinue parenteral fluids • Anticholinergic drugs may be required…. – Reduce production of pharyngeal secretions – ? Less effective on chest secretions compared with oral secretions – E.g. Glycopyrrolate 0.2 – 0.4 mg subcut. q2-4 hr PRN – E.g. Hyoscine hydrobromide (Scopolamine™) 0.2 – 0.4 mg subcut. q2-4 Hr PRN [Back to Basics– Palliative Care – Dr. Shirley Bush] Still Active Management of Symptoms • Prepare patient and family (Difficulty with prognostication) • Full nursing cares - for patient comfort and dignity – – – – – – Eyes: Artificial tears, lacrilube eye ointment Nose: Reassess nasal prongs, salinex gel Oral hygiene: Regular mouth care, moisture spray, gels GI: Suppository PRN GU: Pads, Foley catheter PRN Skin: Pressure area care (Including mattress) • Ongoing review and relief of physical symptoms – delirium, dyspnea @ EOL • Psychosocial (settle affairs)/ spiritual and/or religious needs [Back to Basics– Palliative Care – Dr. Shirley Bush] Preparing for Death • Communication with family: explanation and support • Clinical management – Vitals – discontinue – Investigations – discontinue – Life-prolonging treatments • Evaluate benefit, role in ongoing symptom management • Stop non-essential medications/ ? Discontinue oxygen – Comfort treatments – continue/ institute • Appropriate dosing & schedule – Parenteral route for medications (subcut. route generally) when patient no longer able to swallow/ in anticipation of this • Review role for Medically Assisted Hydration & Nutrition • Deactivate Implantable Cardioverter Defibrillator (ICD) [Back to Basics– Palliative Care – Dr. Shirley Bush] Review Venue of Care • Knowledge of options available • ? Hospital vs. Palliative Care unit vs. hospice vs. nursing home/LTC vs. home • Single room if possible • If needed, liaise with Palliative Care Hospital Consult service – Liaise with Family Physician – As Early as possible – Community palliative care team (24 hr cover) - RPCT – Referral to community nursing service (CCAC) • Supply of drugs with medication orders, hospital bed and other equipment, ?Foley catheter, ? Dressings, ??Oxygen • Insert indwelling Subcut. butterfly needle • Urgent ambulance home/ completed MOHLTC DNR order [Back to Basics– Palliative Care – Dr. Shirley Bush] Planning for Crises • Community: Supply of emergency drugs at home – E.g. Subcut. opioid, neuroleptic, antiemetic, benzodiazepine, anticholinergic (EOL) • Risk of Hemorrhage • E.g. Carotid hemorrhage in Head and Neck (H&N) cancer • E.g. Massive GI bleed, massive hemoptysis – Discuss with family and staff – Green towels – Catastrophic order/ Crisis pack • Midazolam 5- 10mg subcut. (or I.M.), +/- Usual opioid rescue dose and repeat q5 minutes PRN if needed – Stay with patient (At home: advise family not to call 911 – DNR order in place) [Back to Basics– Palliative Care – Dr. Shirley Bush] Essential Medications at EOL …… • Cessation or subcut. conversion of oral medications – Consider continuous Subcut. infusion • ? Opioid (e.g. for pain, dyspnea) • +/- Antipsychotic for delirium – E.g. Haloperidol, methotrimeprazine (Nozinan™) • +/- Sedative agent for refractory delirium, refractory dyspnea at the end of life – E.g. Midazolam, lorazepam, methotrimeprazine (Nozinan™), phenobarbital • +/- Antiemetic • +/- Anticholinergic for respiratory secretions – E.g. Glycopyrrolate, hyoscine • Review parenteral fluids/ oxygen [Back to Basics– Palliative Care – Dr. Shirley Bush] Caring for Patients - and Families - at the End of Life • • • • • Address fears and concerns Reassurance where appropriate ? Hearing and Touch last senses to go Suggest notifying family/ friends, especially if overseas Consider allied health support (social work, spiritual care, psychology) if not already involved • Ensure family members looking after selves (eating, drinking, sleep) • “Keeping vigil”: Give permission for family to leave room and take breaks, or create a roster for family shifts • Enquire if any cultural or religious/spiritual needs for end of life care, and after death [Back to Basics– Palliative Care – Dr. Shirley Bush] Orienting Ourselves for End of Life (EOL) Care • Reflective Discussion Video – Orienting Ourselves for Hospice, Palliative & EOL Care (5 minutes) • From pallium.ca • http://www.youtube.com/watch?v=sP4Fkjn3OwU [Back to Basics– Palliative Care – Dr. Shirley Bush] • Any Questions….. • Please feel free to contact me: • sbush@bruyere.org [Back to Basics– Palliative Care – Dr. Shirley Bush] Guerir quelquefois Soulager souvent Consoler toujours To cure occasionally To relieve often To comfort always Death in the sickroom, Edvard Munch, 1895 [Back to Basics– Palliative Care – Dr. Shirley Bush]