emergencies in general practice
advertisement

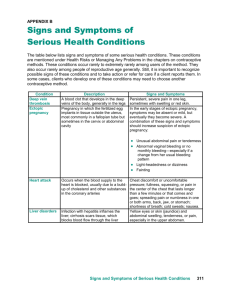
EMERGENCIES IN GENERAL PRACTICE By Amina Ahmed & Simon Robinson CASE A Case A - Anaphylaxis Anaphylaxis is a severe, life-threatening, generalised or systemic hypersensitivity reaction. It is characterised by rapidly developing life-threatening airway and/or breathing and/or circulation problems usually associated with skin and mucosal changes. In general, the more rapid the onset of the reaction, the more serious it will be. Symptoms can develop within minutes and early, effective treatment may be life saving. Anaphylactic reactions may also be associated with additives and excipients in medicines. It is wise therefore to check the full formulation of preparations which may contain allergenic fats or oils (including those for topical application, particularly if they are intended for use in the mouth). Case A - Anaphylaxis Signs and symptoms may include: • Urticaria, erythema, rhinitis, conjunctivitis. • Abdominal pain, vomiting, diarrhoea and a sense of impending doom. • Flushing is common, but pallor may also occur. • Marked upper airway (laryngeal) oedema and bronchospasm may develop, causing stridor, wheezing and/or a hoarse voice. • Vasodilation causes relative hypovolaemia leading to low blood pressure and collapse. This can cause cardiac arrest. • Respiratory arrest leading to cardiac arrest. Case A – Anaphylaxis Management Case A – Anaphylaxis Management CASE B Cardiac emergencies The signs and symptoms of cardiac emergencies include chest pain, shortness of breath, fast and slow heart rates, increased respiratory rate, low blood pressure, poor peripheral perfusion (indicated by prolonged capillary refill time) and altered mental state. If there is a history of angina the patient will probably carry glyceryl trinitrate spray or tablets (or isosorbide dinitrate tablets) and they should be allowed to use them. Where symptoms are mild and resolve rapidly with the patient’s own medication, hospital admission is not normally necessary. Sudden alterations in the patient’s heart rate (very fast or very slow) may lead to a sudden reduction in cardiac output with loss of consciousness. Medical assistance should be summoned by dialling 999. Case B. Myocardial infarction Symptoms and signs of myocardial infarction • Progressive onset of severe, crushing pain in the centre and across the front of chest. The pain may radiate to the shoulders and down the arms (more commonly the left), into the neck and jaw or through to the back. Skin becomes pale and clammy. Nausea and vomiting are common. Pulse may be weak and blood pressure may fall. Shortness of breath. Case B. Myocardial infarction Call 999 immediately for an ambulance. Allow the patient to rest in the position that feels most comfortable; in the presence of breathlessness this is likely to be the sitting position. Patients who faint or feel faint should be laid flat; often an intermediate position (dictated by the patient) will be most appropriate. Give high flow oxygen (10 litres per minute). Give sublingual GTN spray if this has not already been given. Reassure the patient as far as possible to relieve further anxiety. Give aspirin in a single dose of 300 mg orally, crushed or chewed. Ambulance staff should be made aware that aspirin has already been given as should the hospital. Many ambulance services in the UK will administer thrombolytic therapy before hospital admission. If the patient becomes unresponsive always check for ‘signs of life’ (breathing and circulation) and start CPR in the absence of signs of life or normal breathing (ignore occasional ‘gasps’). WITHOUT AED WITH AED CASE C Case C. Epileptic seizures Symptoms and signs There may be a brief warning or ‘aura’. Sudden loss of consciousness, the patient becomes rigid, falls, may give a cry, and becomes cyanosed (tonic phase). After a few seconds, there are jerking movements of the limbs; the tongue may be bitten (clonic phase). There may be frothing from the mouth and urinary incontinence. The seizure typically lasts a few minutes; the patient may then become floppy but remain unconscious. After a variable time the patient regains consciousness but may remain confused. Case C. Epileptic seizures Fitting may be a presenting sign of Hypoglycaemia and should be considered in all patients, especially known diabetics and children. An early blood glucose measurement is essential in all actively fitting patients (including known epileptics). Check for the presence of a very slow heart rate (<40 per minute) which may drop the blood pressure. This is usually caused by a vasovagal episode (see Syncope section below). The drop in blood pressure may cause transient cerebral hypoxia and give rise to a brief fit. Case C. Epileptic seizures Management During a convulsion try to ensure that the patient is not at risk from injury but make no attempt to put anything in the mouth or between the teeth (in the mistaken belief that this will protect the tongue). Do not attempt to insert an oropharyngeal airway or other airway adjunct while the patient is actively fitting. Give high flow oxygen (10 litres per minute). Do not attempt to restrain convulsive movements. After convulsive movements have subsided place the patient in the recovery position and reassess. Case C. Epileptic seizures Management If the patient remains unresponsive always check for ‘signs of life’ (breathing and circulation) and start CPR in the absence of signs of life or normal breathing (ignore occasional ‘gasps’). Check blood glucose level to exclude hypoglycaemia. If blood glucose <3.0 mmol per litre or hypoglycaemia is clinically suspected, give oral/buccal glucose, or glucagon (see Hypoglycaemia section below). Case C. Epileptic seizures Management After the convulsion the patient may be confused (‘post-ictal confusion’) and may need reassurance and sympathy. The patient should not be sent home until fully recovered and they should be accompanied. It may not always be necessary to seek medical attention or transfer to hospital unless the convulsion was atypical, prolonged (or repeated), or if injury occurred. The National Institute for Clinical Excellence (NICE) guidelines suggest the indications for sending to hospital are: Status epilepticus. High risk of recurrence. First episode. Difficulty monitoring the individuals condition. Case C. Epileptic seizures Management Medication should only be given if seizures are prolonged (convulsive movements lasting 5 minutes or longer) or recur in quick succession. In this situation an ambulance should be summoned urgently. With prolonged or recurrent seizures, ambulance personnel will often administer IV diazepam which is usually rapidly effective in stopping any seizure. An alternative, although less effective treatment, is midazolam given via the buccal or intranasal route in a single dose of 10mg for adults. For children the dose can be simplified as follows: child 1-5 years 5mg, child 5-10 years 7.5mg, above 10 years 10mg. This might usefully be administered while waiting for ambulance treatment, but the decision to do this will depend on individual circumstances. CASE D CASE D. HYPOGLYCAEMIA Patients with diabetes should eat normally and take their usual dose of insulin or oral hypoglycaemic agent before any planned dental treatment. If food is omitted after having insulin, the blood glucose will fall to a low level (hypoglycaemia). This is usually defined as a blood glucose <3.0 mmol per litre, but some patients may show symptoms at higher blood sugar levels. Patients may recognise the symptoms themselves and will usually respond quickly to glucose. Children may not have such obvious features but may appear lethargic. CASE D. HYPOGLYCAEMIA Symptoms and signs • Shaking and trembling. • Sweating. • Headache. • Difficulty in concentration / vagueness. • Slurring of speech. • Aggression and confusion. • Fitting. • Unconsciousness. CASE D. HYPOGLYCAEMIA The following staged treatment protocol is a suggested depending on the status of the patient. If any difficulty is experienced or the patient does not respond, the ambulance service should be summoned immediately; ambulance personnel will also follow this protocol. Confirm the diagnosis by measuring the blood glucose. Early stages - where the patient is co-operative and conscious with an intact gag reflex, give oral glucose (sugar (sucrose), milk with added sugar, glucose tablets or gel). If necessary this may be repeated in 10 –15 minutes. CASE D. HYPOGLYCAEMIA In more severe cases - where the patient has impaired consciousness, is uncooperative or is unable to swallow safely buccal glucose gel and / or glucagon should be given. Glucagon should be given via the IM route (1mg in adults and children >8years old or >25 kg, 0.5mg if <8 years old or <25 kg). Remember it may take 5-10 minutes for glucagon to work and it requires the patient to have adequate glucose stores. Thus, it may be ineffective in anorexic patients, alcoholics or some non-diabetic patients. Re-check blood glucose after 10 minutes to ensure that it has risen to a level of 5.0 mmol per litre or more, in conjunction with an improvement in the patient’s mental status. CASE E CASE E. ASTHMA Patients with asthma (both adults and children) may have an attack whilst at the surgery. Most attacks will respond to a few ‘activations’ of the patient’s own short-acting beta2-adrenoceptor stimulant inhaler such as salbutamol (100 micrograms/actuation). Repeat doses may be necessary. If the patient does not respond rapidly, or any features of severe asthma are present, an ambulance should be summoned. Patients requiring additional doses of bronchodilator should be referred for medical assessment after emergency treatment. If the patient is unable to use the inhaler effectively, additional doses should be given through a large-volume spacer device. CASE E. ASTHMA Symptoms and Signs Clinical features of acute severe asthma in adults include: • Inability to complete sentences in one breath. • Respiratory rate > 25 per minute. • Tachycardia (heart rate > 110 per minute). Clinical features of life threatening asthma in adults include: • Cyanosis or respiratory rate < 8 per minute. • Bradycardia (heart rate < 50 per minute). • Exhaustion, confusion, decreased conscious level. CASE E. ACUTE SEVERE ASTHMA MANAGEMENT If the reponse is unsatisfactory and a nebuliser is unavailable, 4–6 activations from the salbutamol inhaler should be given using a large-volume spacer device and repeated every 10 minutes if necessary until an ambulance arrives. If the response remains unsatisfactory and a nebuliser is available, give salbutamol 2.5mg-5mg via a nebuliser, and oral prednisolone, 30mg stat. If the response remains unsatisfactory and the patient develops tachycardia, becomes distressed or cyanosed, arrangements must be made to transfer the patient urgently to hospital. CASE E. ACUTE SEVERE ASTHMA MANAGEMENT If any patient becomes unresponsive always check for ‘signs of life’ (breathing and circulation) and start CPR in the absence of signs of life or normal breathing (ignore occasional ‘gasps’). CASE F CASE F. EPISTAXIS Epistaxis is so common that almost everyone has had a nosebleed on at least several occasions, usually as a result of trauma. It has peaks of incidence at age 2-10 and 50-80 years old. Both sexes are equally affected. It is classified as anterior or posterior, depending upon the source of bleeding Anterior haemorrhage - The source of bleeding is visible in about 90% of cases - usually from the nasal septum Posterior haemorrhage - This emanates from deeper structures of the nose, and occurs more commonly in older individuals CASE F. EPISTAXIS CAUSES Trauma to the nose (commonest cause) - especially nose picking! Insertion of foreign bodies and excessive nose blowing may also be seen as trauma. The latter is likely to occur with a cold when the nasal mucosa is congested. Sinusitis causes nasal congestion. Disorders of platelet function. Thrombocytopenia and other causes of abnormal platelets including splenomegaly and leukaemia. Waldenström's macroglobulinaemia may present with nosebleeds. ITP can occur in children and young adults. Drugs - aspirin and anticoagulants. Disorders of platelets are more likely to be a problem than clotting factor deficiency. Abnormalities of blood vessels. In the elderly arteriosclerotic vessels prolong bleeding. Hereditary haemorrhagic telangiectasia (Osler-Weber-Rendu syndrome) causes recurrent epistaxis from nasal telangiectasiae. Malignancy of the nose may present with bleeding. Juvenile angiofibroma is a highly vascular benign tumour that typically presents in adolescent males. Cocaine Use - If the septum looks sloughed or atrophic ask about use of cocaine.3 The drug is usually taken by inhalation and it has a very strong vasoconstrictive effect that can lead to complete obliteration of the nasal septum. Other conditions - Wegener's granulomatosis and pyogenic granuloma can present as an epistaxis. CASE F. EPISTAXIS MMANAGEMENT Iniatial Assessment, First Aid Maintain a calm attitude around the patient - but protect yourself (gloves, gown and goggles - the 3Gs). Resuscitate the patient (if necessary) - remember the ABCD(E) of resuscitation. Take a quick history Which nostril is bleeding? Is there blood the pharynx? How much blood loss has there been? Are there symptoms of hypovolaemia? Is the bleeding recurrent? What measures have been tried before? Past medical history (e.g. recent trauma) and current medication (especially aspirin or warfarin). CASE F. EPISTAXIS MMANAGEMENT Get the patient to sit upright, leaning slightly forward; and to squeeze the bottom part of the nose (NOT the bridge of the nose) for 10-20 minutes to try and stop the bleeding . Patient should breathe through the mouth and spit out any blood/saliva into a bowl. An ice pack on the bridge of the nose may help. Monitor pulse and blood pressure. If bleeding has stopped after this time (as it does in most cases) proceed to inspect the nose using a nasal speculum and consider cautery. If the history is of severe and prolonged bleeding get expert help - and watch carefully for signs of hypovolaemia etc.. CASE F. EPISTAXIS MANAGEMENT Silver nitrate cautery and naseptin cream Anterior bleeds - Packing Posterior bleeds – packing/ balloon catheter CASE F. EPISTAXIS MANAGEMENT These are unnecessary in most (mild) cases but recurrent or severe cases require at least a FBC, coagulation studies and blood typing. Quite marked anaemia can result but a haematological malignancy may also be revealed. Any suspicion of malignancy of the nose or other abnormality should require referral to an ENT surgeon. CASE G CASE G - CHOKING Children are susceptible to choking Symptoms and Signs • The patient may cough and splutter. • They may complain of difficulty breathing. • Breathing may become noisy with wheeze (usually aspiration) or stridor(usually upper airway obstruction). • They may develop ‘paradoxical’ chest or abdominal movements. • They may become cyanosed and lose consciousness. CASE G – CHOKING MANAGEMENT The treatment of the choking patient involves removing any visible foreign bodies from the mouth and pharynx. Encourage the patient to cough if conscious. If they are unable to cough but remain conscious then sharp back blows should be delivered. These can be followed by abdominal thrusts if the foreign body has not been dislodged. If the patient becomes unconscious, CPR should be started. This will not only provide circulatory support but the pressure generated within the chest by performing chest compressions may help to dislodge the foreign body. CASE G – CHOKING MANAGEMENT CASE H CASE H - TRAUMA Trauma Assessment The initial assessment and management of seriously injured patients is a challenging task and requires a rapid and systematic approach. This systematic approach can be practised to increase speed and accuracy of the process but good clinical judgement is also required. Although described in sequence some of the steps will be taken simultaneously. The aim of good trauma care is to prevent early trauma mortality. Early trauma deaths occur because of failure of oxygenation of vital organs or central nervous system injury or both. Injuries causing this mortality occur in predictable patterns and recognition of these patterns led to the development of Advanced Trauma Life Support (ATLS) by the American College of Surgeons. A standardised protocol for trauma patient evaluation has been developed. The protocol celebrated its 25th anniversary in 2005. Good teaching and application of this protocol is held to be an important factor in improving the survival of trauma victims worldwide. CASE H – TRAUMA MANAGEMENT First and most important: Is it safe to approach? CASE H – TRAUMA MANAGEMENT Aims of the initial evaluation of trauma patients Stabilise the patient Identify life threatening conditions in order of risk and initiate supportive treatment Organise definitive treatments or organise transfer for definitive treatments Preparation and coordination of care Assessment and management will begin out of hospital at the scene of injury and good communication with the receiving hospital is important. The preparatory measures are outlined below to 'set the scene': CASE H – TRAUMA MANAGEMENT The prehospital phase Preparation of a resuscitation area Airway equipment (laryngoscopes etc accessible, tested) Intravenous fluids (warming equipment etc) Immediately available monitoring equipment Methods of summoning extra medical help Prompt laboratory and radiology backup Transfer arrangements with trauma centre. Guidelines on protection when dealing with body fluid should be followed throughout this and subsequent procedures. CASE H – TRAUMA MANAGEMENT General principles 1. Follow the Airway, Breathing, Circulation, Disability, and Exposure approach (ABCDE) to assess and treat the patient. 2. Treat life-threatening problems as they are identified before moving to the next part of the assessment. 3. Continually re-assess starting with Airway if there is further deterioration. 4. Assess the effects of any treatment given. 5. Recognise when you need extra help and call for help early. This may mean dialling 999 for an ambulance. 6. Use all of your resources – ask members of public for help. This will allow you to do several things at once, e.g., collect emergency drugs and equipment, dial 999. CASE H – TRAUMA MANAGEMENT Initial assessment This comprises: Primary survey Resuscitation Secondary survey Definitive treatment or transfer for definitive care CASE H – TRAUMA MANAGEMENT A= Airway maintenance cervical spine protection B= Breathing and ventilation C= Circulation with haemorrhage control D= Disability: Neurological status E= Exposure/ environmental control CASE H – TRAUMA MANAGEMENT As part of the secondary survey History: A=Allergies M=Medication currently used P=Past illnesses/Pregnancy L=Last meal E=Events/Environment related to injury CASE H – TRAUMA MANAGEMENT A= Airway maintenance cervical spine protection Are there signs of airway obstruction, foreign bodies, facial, mandibular or laryngeal fractures? Establish a clear airway (chin lift or jaw thrust) but protect the cervical spine at all times. If the patient can talk the airway is likely to be safe but remain vigilant and recheck. GCS less than 8 requires definitive airway. CASE H – TRAUMA MANAGEMENT B= Breathing and ventilation Evaluate breathing: lungs, chest wall, diaphragm. Chest examination with adequate exposure: watch chest movement, auscultate, percuss to detect lesions acutely impairing ventilation: Tension pneumothorax Flail chest Haemothorax Pneumothorax. CASE H – TRAUMA MANAGEMENT C= Circulation with haemorrhage control Blood loss is the main preventable cause of death after trauma. To assess blood loss rapidly observe: Level of consciousness Skin colour Pulse. Bleeding should be assessed and controlled: Direct manual pressure should be used (not tourniquets except for traumatic amputation as these cause distal ischaemia). Transparent pneumatic splinting devices may control bleeding and allow visual monitoring. Occult bleeding into the abdominal cavity and around long bone or pelvic fractures is problematic. CASE H – TRAUMA MANAGEMENT D= Disability: Neurological status After A,B and C above rapid neurological assessment is made to establish Level of consciousness, using Glasgow Coma Scale Pupils: size, symmetry and reaction Any lateralising signs Level of any spinal cord injury (limb movements, spontaneous respiratory effort) Note: remember oxygenation, ventilation, perfusion, drugs, alcohol and hypoglycaemia may all also affect level of consciousness. CASE H – TRAUMA MANAGEMENT E= Exposure/ environmental control Undress patient, but prevent hypothermia Clothes may need to be cut off, but after examination attention to prevention of heat loss with warming devices, warmed blankets etc is important, Intravenous fluids should be warmed before infusion. CASE I CASE I – GI BLEEDING Upper gastrointestinal bleeding (UGIB) is a significant and potentially life-threatening worldwide problem. Despite advances in diagnosis and treatment, mortality and morbidity have remained constant. Bleeding from the upper gastrointestinal tract (GIT) is about 4 times as common as bleeding from the lower GIT. Typically patients present with bleeding from a peptic ulcer and about 80% of such ulcers stop bleeding. Increasing age and co-morbidity increase mortality. It is important to identify patients with a low probability of re-bleeding from patients with a high probability of re-bleeding. CASE I – GI BLEEDING Aetiology A cause is found in 80% of cases. Approximate percentages given. Note the predominance of peptic ulcer disease Peptic ulcer disease 35 to 50%: Gastroduodenal erosions 8 to 15% Oesophagitis 5 to 15% Oesophageal varices 5 to 10% 'Mallory-Weiss' tears 15% Upper gastrointestinal malignancy 1% Vascular malformations 5% Rare causes - less than 5%: Dieulafoy's lesion (a vascular malformation of the proximal stomach) Angiodysplasia; Haemobilia (bleeding from the gallbladder or biliary tree); Pancreatic pseudocyst and pseudo-aneurysm; Aortoenteric fistula; Bleeding diathesis; Ehlers-Danlos syndrome; Pseudoxanthoma elasticum; Gastric antral vascular ectasia; and Rendu-Osler-Weber syndrome CASE I – GI BLEEDING The strong association of Helicobacter pylori (H. pylori) infection with duodenal ulcer is worthy of special mention. The organism disrupts the mucosal barrier and causes inflammation in the gastric and duodenal mucosae. Eradication reduces the risk of both recurrent ulcers and recurrent haemorrhage. Non-steroidal anti-inflammatory drugs (NSAIDS) are the second most important aetiological factor. They exert an effect on cyclooxygenase-1 leading to impaired resistance of the mucosa to acid. The size of the bleeding vessel is important in prognosis. Visible vessels are usually between 0.3 mm and 1.8 mm. Large bleeding vessels cause faster blood loss. Generally larger vessels are found deeper in the submucosa and serosa and more specifically high in the lesser curve of the stomach and postero-inferiorly in the duodenal bulb. CASE I – GI BLEEDING Peptic ulcer disease is the most common cause of UGIB. Risk factors for peptic ulcer disease are: Alcohol abuse Chronic renal failure Non-steroidal anti-inflammatory use Age Low socio-economic class Although duodenal ulcers are more common than gastric ulcers, both contribute nearly equally to the incidence of UGIB. After an initial bleed the risk factors for re-bleeding, with associated higher mortality, are: Age over 60 Presence of signs of shock at admission Coagulopathy Pulsatile haemorrhage Cardiovascular disease CASE I – GI BLEEDING Assessment History Is there abdominal pain? History of other gastrointestinal symptoms should be sought. The symptoms in order of frequency are: Haematemesis including coffee-ground emesis: 40 to 50% Melaena: 70 to 80% Haematochezia (red or maroon stool): 15 to 20% Syncope: 14% Presyncope: 43% Dyspepsia:18% Epigastric pain: 41% Diffuse abdominal pain:10% Weight loss: 12% Jaundice 5% CASE I – GI BLEEDING Alcohol intake. Past history of bleeding (haematemesis or melaena) or of anaemia. Drug history is important. Drugs such as NSAIDs, aspirin and corticosteroids are an important cause of bleeding. Iron and bismuth may mimic melaena. Retching may precede bleeding with a 'Mallory-Weiss' tear. CASE I – GI BLEEDING Examination The main aim of examination is to assess blood loss and look for signs of shock. A secondary aim is to look for signs of underlying disease and significant co-morbid conditions. For example: Pallor and signs of anaemia should be sought Pulse and blood pressure Postural hypotension may be detected and usually indicates a blood loss of 20% or more Other signs of shock: Cool extremities; Chest pain; Confusion; and Delirium CASE I – GI BLEEDING Evidence of dehydration (dry mucosa, sunken eyes, skin turgor reduced) Stigmata of liver disease may be present (jaundice, gynaecomastia, ascites, spider naevi, flap etc) Signs of a tumour may be present (nodular liver, abdominal mass, lymphadenopathy) Subcutaneous emphysema and vomiting suggests Boerhaave's syndrome (oesophageal perforation) Urine output should be monitored (oliguria is a sign of shock) CASE I – GI BLEEDING Differential Diagnosis Abdominal aortic aneurysm Boerhaave's syndrome Cholecystitis Coeliac sprue Dengue fever Disseminated intravascular coagulation Zollinger-Ellison syndrome Von Willebrand's disease CASE I – GI BLEEDING Assessment of bleeding severity and re-bleeding Bleeding severity can be assessed by: The extent of blood loss The degree of shock However there are other factors which affect risk of death: Age: deaths under age 40 years are rare. 30% of patients over 90 years old with UGIB die as a result of the bleed. Co-morbidity: complications are more likely with co-morbid disease. Shock: the presence of signs of shock confers a worse prognosis. Endoscopic findings: much work has been done on classifying and identifying endoscopic findings which correlate with high risk. For example: 'Mallory-Weiss' tears or clean ulcers have a low risk of re-bleeding and death. Active bleeding in a shocked patient carries an 80% risk of re-bleeding or death. Non-bleeding but visible vessel has a 50% risk of re-bleeding. CASE I – GI BLEEDING Risk of Re-bleeding Various methods have been designed to assess the risk of rebleeding. These include Rockall score (see next slide) and Baylor score. Use of these remains controversial. Co-morbid conditions have a significant effect on prognosis, as embodied in the Rockall assessment. Patients with advanced renal or liver disease and disseminated cancer fare worst. Note: the Rockall score is a very useful tool but you should always use your clinical judgement in each individual case. CASE I – GI BLEEDING CASE I – GI BLEEDING MANAGEMENT Rockall score - initial assessment or at admission Calculate the initial Rockall score: If 0, then consider patient for discharge or non-admission with out-patient follow-up. Rockall score >0 - i.e. all other patients - should be considered for admission and early endoscopy and should have a full Rockall score calculation. Patients who have a Rockall score >0 should have an early endoscopy which will allow calculation of their full Rockall score. CASE I – GI BLEEDING MANAGEMENT Resuscitation is a priority It has been demonstrated that early and aggressive resuscitation reduces mortality in UGIB. Maintain airway - remember vomitus can lead to airway obstruction. Provide high flow oxygen - this will aid tissue perfusion. Correct fluid losses (place 2 wide bore cannulae and also send bloods at the same time). Initial fluid resuscitation may be with crystalloids or colloids; give intravenous blood when 30% of circulating volume is lost. Major haemorrhage protocols should be in place. CASE I – GI BLEEDING MANAGEMENT Once patient is more stable Assess the patient, taking history and examining the patient as above - a collateral history might be needed. Identify and treat any co-morbid conditions. Estimate the severity of bleeding CASE I – GI BLEEDING MANAGEMENT Endoscopy Ideally, endoscopy should be performed within 24 hours. Endoscopy can be used both in diagnosis and therapy. Therapy might involve injection of adrenaline or other sclerosants, thermal coagulation or application of clips. Meta-analysis of trials has shown that endoscopic haemostatic techniques reduce bleeding, reduce the need for surgery and reduce mortality. Endoscopic therapy should be applied to the following: Actively bleeding lesion Non-bleeding visible vessels Ulcers with adherent clot The preference is for dual therapy, e.g. injection of adrenaline with thermal coagulation. High dose PPI should be given to those with major peptic ulcer bleeding, i.e. active bleeding or non-bleeding visible vessel. All other patients who do not receive endoscopic therapy should commence oral PPI post-procedure. CASE I – GI BLEEDING MANAGEMENT Medical management post-endoscopy H. pylori eradication: All patients with bleeding peptic ulcer should be tested for H. pylori, e.g. urea breath test and biopsy specimen. Patients who test positive should receive a 1-week course of eradication therapy. This should be followed by 3 further weeks with ulcer healing treatment. All therapy can be discontinued after successful healing of peptic ulcers provided patients are not taking NSAIDs. A negative urea breath test should be confirmed on the initial biopsy specimen taken prior to diagnosis and before any PPI therapy was given. Two weeks after successful therapy and stopping of all medication, a repeat urea breath test should be performed to confirm successful eradication. Unsuccessful eradication should be treated with second-line therapy. CASE I – GI BLEEDING MANAGEMENT Other points to note: PPI use is not recommended prior to diagnosis by endoscopy in the latest SIGN guidance, however current hospital protocols often include PPI use for suspected UGIB before endoscopic confirmation. There is insufficient evidence to use somatostatin or tranexamic acid in UGIB. In selected patients (e.g. variceal haemorrhage) it may be appropriate to use terlipressin or octreotide and, in the case of uncontrolled UGIB in an unstable patient, balloon tamponade may be necessary, e.g. Sengstaken-Blakemore, Minnesota or Linton-Nachlas tubes. Patients with an UGIB might need to be admitted to a high-dependency unit or intensive care unit. This decision should be clinical and used in conjunction with the Rockall score. Some hospitals have beds specifically for patients with an UGIB. Evidence suggests that patients with UGIB should be assessed and managed in dedicated units as their outcome is improved. Emergency endoscopy should be available 24 hours a day in such units. Note that patients with liver disease are a special case and have separate guidelines for management. CASE I – GI BLEEDING MANAGEMENT Other Medication: Anticoagulants and antiplatelet agents should be stopped during the acute phase and restarted later only if there is a clear indication. Patients who have healed ulcers and were H. pylori negative and require aspirin or NSAIDs or COX2 inhibitors, should be given concomitant PPI. SSRIs should be used in caution in patients at risk of UGIB or who have had a previous UGIB (especially if other drugs such as aspirin or NSAIDs are used). Corticosteroids will also need to be used carefully and probably with concomitant PPI in high-risk patients or those on high doses. CASE J CASE J. ECTOPIC PREGNANCY An ectopic pregnancy is one that occurs anywhere outside the uterus By far the commonest place for ectopic pregnancy is the fallopian tubes. There are a few documented cases of viable pregnancy outside the uterus and tubes but as a general rule only an intrauterine pregnancy is viable. CASE J. ECTOPIC PREGNANCY Risk factors Pelvic inflammatory disease may cause complete tubal occlusion or delay the transport of the embryo so that implantation occurs in the tube. Adhesions from infection and inflammation from endometriosis may play a part. Ectopic pregnancy has been reported in tubes that have been divided in a sterilisation operation and where they have been reconstructed to reverse one. Ectopic pregnancy has been reported in the treatment of infertility Right sided tubal pregnancy is commoner than on the left. This is thought to be from spread of infection from appendicitis. The ability of the tube to expand increases from medially to laterally. Hence a more lateral implantation will present later as either pain or rupture. Where an IUCD or progestogen-only oral contraceptives, including emergency contraception fails, the risk of a pregnancy being ectopic is greater than with other forms of contraception. Depot and implant contraception may not have the same risks. Ectopic pregnancy has been reported with implant contraception with etonogestrel (Implanon™) but appears rare. An IUCD, being a foreign body with threads hanging into the vagina, increases the risk of infection. It is effective at preventing intrauterine pregnancy but probably ineffective at preventing pregnancy at other sites. Therefore, if pregnancy occurs with an IUCD in situ consider ectopic pregnancy CASE J. ECTOPIC PREGNANCY PRESENTATION 30% of ectopics present before a period has been missed The first symptom is usually pain. This may be left or right iliac fossa pain or it may be central and suprapubic. If vaginal bleeding occurs it is much less significant than the pain. There may be a missed period and signs of pregnancy, perhaps even a positive pregnancy test. There may be a history of a previous ectopic pregnancy. After one ectopic pregnancy the chance of another in the other tube is much increased. If the ectopic pregnancy has ruptured, bleeding is profuse and there may be features of hypovolaemic shock including feeling dizzy on standing. Most bleeding will be into the pelvis and so vaginal bleeding may be minimal and misleading. Recent CEMACH reports have repeatedly emphasised the importance of diarrhoea and vomiting as a possible, atypical clinical presentation of ectopic pregnancy. CASE J. ECTOPIC PREGNANCY Examination There may be some tenderness in the suprapubic region to left or right of the midline. If bleeding has started there may be peritonism and signs of an acute abdomen. There may be signs of early pregnancy such as fullness and tenderness of the breasts. Bimanual vaginal examination may reveal a tender fullness of one adnexum but some authorities recommend that this should not be done as the examination may rupture the tubal pregnancy. There is evidence that vaginal examination in suspected ectopic pregnancy adds nothing to the clinical picture and so should be avoided.5 The cited paper is just one of many reaching a similar conclusion. A check must be made for signs of blood loss. If there is hypovolaemic shock, resuscitation and transfer to hospital must occur without delay. CASE J. ECTOPIC PREGNANCY Investigation The most accurate method to detect a tubal pregnancy is transvaginal ultrasound. Its availability improves management. Quantitative assessment of hCG levels is of value in confirming pregnancy and follow up if there is medical or conservative management. If hCG is below 1000 units and ultrasound has failed to locate an intrauterine or tubal pregnancy it is called a pregnancy of unknown location. CASE J. ECTOPIC PREGNANCY MANAGEMENT Admit as an emergency if the diagnosis of ectopic pregnancy is considered a possibility. A bedside pregnancy test should be performed on all women of childbearing age presenting with lower abdominal pain where pregnancy is even the remotest possibility. Expectant Management in hospital Clinically stable patient, HCG<1000 and falling Medical Management Haemodynamically stable and initial HCG<3000 IM Methotrexate Need Reliable contraception for 3months after 10% need surgical intervention Surgical Management CASE J. ECTOPIC PREGNANCY MANAGEMENT Prognosis The risk of another ectopic pregnancy is about 10 to 20% The chance of subsequent intrauterine pregnancy is about 55 to 60% Prevention Ectopic pregnancy does not occur in normal tubes, so prevention is based on avoiding the cause of damaged tubes This includes avoiding promiscuity and activities that predispose to pelvic inflammatory disease and the early diagnosis and treatment of appendicitis. That is not to say that all PID is sexually transmitted but many of the infecting organisms, including Chlamydia spp. are usually spread by that route. Routine screening of asymptomatic people for chlamydia may reduce the incidence of ectopic pregnancy, but this is yet to be proved.