NEW PATIENT QUESTIONNAIRE - Saint Luke`s Health System
advertisement
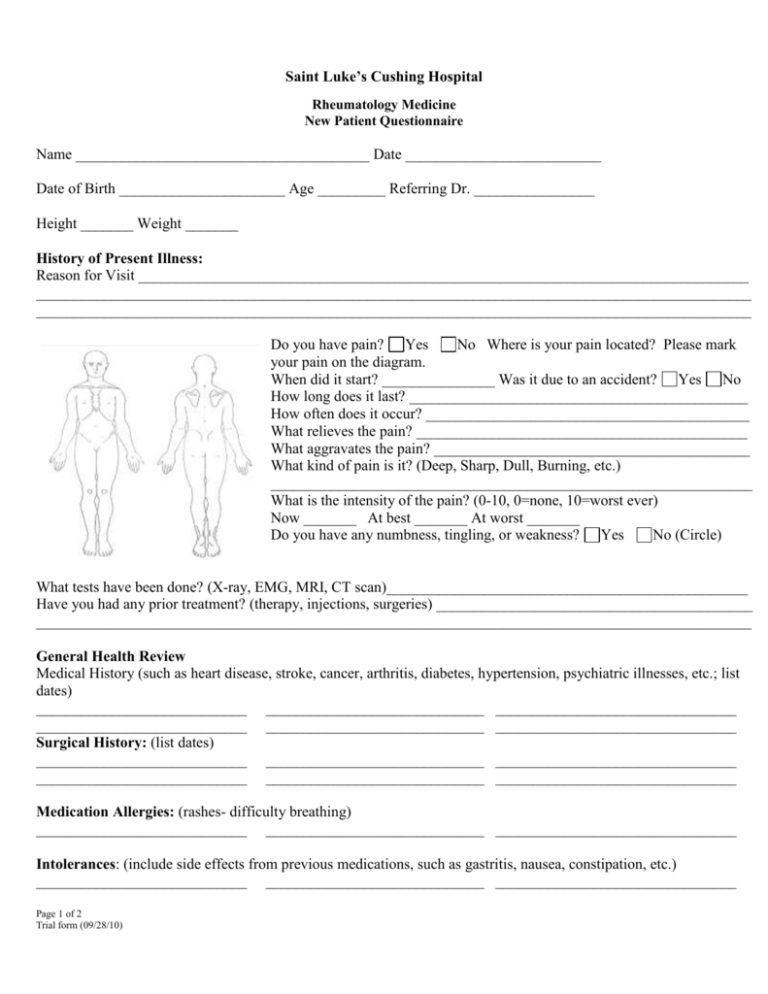
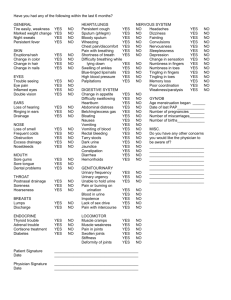
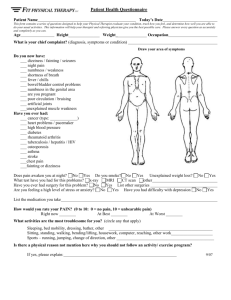
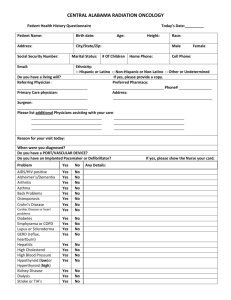
Saint Luke’s Cushing Hospital Rheumatology Medicine New Patient Questionnaire Name _______________________________________ Date __________________________ Date of Birth ______________________ Age _________ Referring Dr. ________________ Height _______ Weight _______ History of Present Illness: Reason for Visit _________________________________________________________________________________ _______________________________________________________________________________________________ _______________________________________________________________________________________________ Do you have pain? Yes No Where is your pain located? Please mark your pain on the diagram. When did it start? _______________ Was it due to an accident? Yes No How long does it last? _____________________________________________ How often does it occur? ___________________________________________ What relieves the pain? ____________________________________________ What aggravates the pain? __________________________________________ What kind of pain is it? (Deep, Sharp, Dull, Burning, etc.) ________________________________________________________________ What is the intensity of the pain? (0-10, 0=none, 10=worst ever) Now _______ At best _______ At worst _______ Do you have any numbness, tingling, or weakness? Yes No (Circle) What tests have been done? (X-ray, EMG, MRI, CT scan)________________________________________________ Have you had any prior treatment? (therapy, injections, surgeries) __________________________________________ _______________________________________________________________________________________________ General Health Review Medical History (such as heart disease, stroke, cancer, arthritis, diabetes, hypertension, psychiatric illnesses, etc.; list dates) ____________________________ _____________________________ ________________________________ ____________________________ _____________________________ ________________________________ Surgical History: (list dates) ____________________________ _____________________________ ________________________________ ____________________________ _____________________________ ________________________________ Medication Allergies: (rashes- difficulty breathing) ____________________________ _____________________________ ________________________________ Intolerances: (include side effects from previous medications, such as gastritis, nausea, constipation, etc.) ____________________________ _____________________________ ________________________________ Page 1 of 2 Trial form (09/28/10) Saint Luke’s Cushing Hospital Rheumatology Medicine New Patient Questionnaire Current Medications: (include vitamins and birth control pills, if applicable) See medication reconciliation form Social History/Functional History: Do you currently work outside of the home? Yes No Occupation: ___________________________________ What type of recreational activities do you do? _________________________________________________________ Do you live by yourself? Yes No Marital Status? ___________________ Home or Apartment? __________________ How many levels? ______________ How many stairs? ______________ Do you use: walker cane crutches bedside commode tub grab bars Smoking History: How much? _______________ How long? _____________ ___Have you quit? Yes No How often do you drink alcohol? _____________________ How much?_____________________ Caffeine: Coffee_____________ Tea______________ Soda______________ How often_________________ Family History: ↑Living ↓Deceased (please circle) Mother ↑ ↓ Diseases ______________________________________________________ Age __________________ Father ↑ ↓ Diseases ______________________________________________________ Age __________________ Brothers ↑ ↓ Diseases ______________________________________________________Ages _________________ Sisters ↑ ↓ Diseases _______________________________________________________ Ages _________________ Children How many? _______ ↑ ↓ Diseases ___________________________________ Ages _________________ Review of Systems: Circle any that apply or NA = not applicable General (weight changes ↑ ↓ ____ lbs., fever, chills, night sweats, insomnia, appetite, NA) SKIN (rashes, color changes, bruising, bleeding, pigmentations, sores, NA) HEAD (headaches, trauma, NA) EYES (reading, visual fields, disturbances, NA) EARS (hearing, infections, discharge, NA) NOSE (sinus problems, smell, NA) MOUTH AND TEETH (teeth: exams, sore throat, swallow, drooling, NA) NECK (lumps, pain, limitation of movement, trauma, circulation, NA) BREASTS (lumps, surgery, pain, discharge, NA) RESPIRATORY (cough, asthma, shortness of breath, painful breathing, NA) CARDIAC (chest pain, heart attack, palpitations, edema, murmurs, hypertension, NA) GASTROINTESTINAL (nausea, vomiting, bleeding, diarrhea, constipation, incontinence) MUSCULO (weakness, arthritis, gout, pain, trauma, scoliosis, back problems, surgeries, cramps, NA) VASCULAR (vein problems, grafts, DVT, leg clots, NA) NEURO (seizures, weakness, paralysis, numbness, tingling, balance, speech, cognition, NA) PSYCH (depression, anxiety, hallucinations, psych care, NA) ENDOCRINE (heat/cold intolerance, osteoporosis, NA) HEMOTOLOGY (anemia, immune problems, clotting, bleeding, blood thinners, NA) Page 2 of 2 Trial form (09/28/10)