Autoimmune Disorder: Psoriasis
advertisement

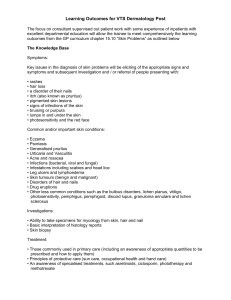
Autoimmune Disorder: Psoriasis Presented by: Paige Barry & Chloe Janson What is Psoriasis? • Chronic skin disease that causes a rapid growth of skin cells. What are Symptoms of Psoriasis? What is the Epidemiology of Psoriasis? • Equally common in males and females • Most common in 15-30 year olds; – Can range from birth to 90 years old • Effects 2-3% of total population (Psoriasis Vulgaris) What are Triggers and Risk Factors? • Medication Triggers – – – – – Lithium Anti-Malarials Quinidine Indomethacin Inderal What is the Genetic Basis of Psoriasis? What is the Genetic Basis of Psoriasis? What is the Genetic Basis of Psoriasis? • Strongest association with MHC class I • Locus: Psoriasis susceptibility I (PSORS1) • Located telomeric to the HLA-C region • Strong association with HLA-Cw6 due to Linkage Disequilibrium (non-random association of alleles at different loci) What is the Genetic Basis of Psoriasis? • HLA-Cw*0602 is a high relative risk factor • Study by Krueger and Bowcock said that HLA-Cw*0602 was found in 10% of healthy controls and 50% of psoriasis patients • No current studies have shown occurrences of psoriasis independent of HLA-Cw6. Cellular Interactions/Inflammation • SLC9A3R1 is a scaffold protein in epithelial cells that sends external signals to plasma membrane proteins • Leads to alterations in signal transduction and cell growth and may be involved in formation of the immune synapse. • Dysregulation of this gene could delay the formation of the synapse, increasing the time that antigen is presented to the T cell receptor, hence leading to prolonged inflammation. Cellular Interactions • Psoriasis histopathology: neutrophils in the papillary dermis and polymorphonuclear leucocytes (neutrophils) in the stratum corneum What is Molecular Mimicry? • A foreign antigen shares sequence or structural similarities with self-antigens • Immune system attacks body due to shared antigens How is Streptococci Recognized? • A streptococci and is recognized by anti-M protein monoclonal antibody (MAb) 10B6. • Two C repeat peptides (C2A and C3) containing the amino acid sequence KGLRRDLDASREAK react with MAb 10B6 What is the Molecular Mimicry of Psoriasis? What is the Molecular Mimicry of Psoriasis? • Step 1: PG and M-protein enter the bloodstream and are taken up by monocytes/macrophages that migrate developing psoriatic lesions. What is the Molecular Mimicry of Psoriasis? • Step 2: Increased frequency of CD4+ and CD8+ T cells in blood. What is the Molecular Mimicry of Psoriasis? • Step 3: Re-circulating CD4+ T cells migrate into the lesional dermis. What is the Molecular Mimicry of Psoriasis? • Step 4: CD8+ T cells migrate through the dermis and into the epidermis (required for the characteristic keratinocyte proliferation of psoriasis). What is the Molecular Mimicry of Psoriasis? • Step 5: Streptococcal components (PG) are presented in the dermis to CD4+ T cells. What is the Molecular Mimicry of Psoriasis? • Step 6: K peptides (crossreact with streptococcal Mprotein) are presented in the epidermis to CD8+ T cells. What is the Molecular Mimicry of Psoriasis? • Step 7: APCs at the dermal– epidermal junction can present PG to CD4+ T cells via HLA class II molecules. What is the Molecular Mimicry of Psoriasis? • Step 8: APCs also present keratin determinants to CD8+ T cells via HLA class I. Effectiveness What are Treatments for Psoriasis? Toxicity How Do These Treatments Work? • Cyclosporin: lowers activity of T cells – Binds to cyclophilin of T cells – Inhibits transcription of IL-2 – Leads to reduced function of effector T cells How Do These Treatments Work? • UVB: reduces dermal T cells and induces T-cell apoptosis – Downregulations the adhesion molecules that recruit T cells from the blood into the skin How Do These Treatments Work? • Anthralin: restores the normal rate of epidermal cell proliferation by reducing the mitotic activity – In vitro studies: prolongs the prophase of mitosis for keratinocytes – In vivo studies: inhibits DNA synthesis and increases release of reactive oxygen species References Berth-Jones J. 2009. Psoriasis. Medicine 37(5):235-241. Bowcock A, Krueger JG. 2005. Getting under the skin: the immunogenetics of psoriasis. Nature Reviews Immunology 5(9): 699-711. Gudjonsson, JE, Elder J. 2007. Psoriasis: epidemiology. Clinics in Dermatology 25(6): 535-546. Krueger JG, Bowcock A. 2005. Psoriasis pathophysiology: current concepts of pathogenesis. Annuals of Rheumatic Diseases 64(2): ii30-ii36. Pardasani AG, Feldman SR, Clark AR. 2000. Treatment of Psoriasis: An Algorithm-Based Approach for Primary Care Physicians. American Academy of Family Physicians 61(3): 725-733. Valdimarsson H, Thorleifsdottir RH, Sigurdardottir SL, Gudjonsson JE, Johnston A. 2009. Psoriasis – as an autoimmune disease caused by molecular mimicry. Trends in Immunology 30(10): 494-501. Study Question 1 • Which of the following is not a trigger of psoriasis? A) Stress B) Genetic Tendency C) Environmental Factors D) Hair loss Study Question 2 • PSORS1 can be defined as…? A) An allele of a gene B) A class of MHC C) A Locus D) A haplotype Study Question 3 • Which of the following Psoriasis treatments inhibits the transcription of IL-2? A) Cyclosporin B) Anthralin C) UVB D) Coal Tar Study Question 4 • Which of the following is an appropriate definition of molecular mimicry A) The non-random assortment of genes B) The body attacking self due to a similarity of a self antigen and a foreign antigen C) Self reactivity due to the presence of a foreign antigen D) The decreased production of T cells in the body due to immune system failure Study Question 5 • A patient with horrible Psoriasis symptoms complains that topical, photo, and systemic treatments aren’t providing enough relief of the symptoms. The doctor suggests that the patient receive a tonsillectomy. Why might this offer the patient greater symptomatic relief?