An-Approach-to-Clinical-Problem-Solving
advertisement

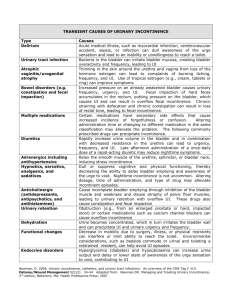
A Logical Approach to Clinical Problem Solving & An applied example on Urinary Incontinence 4 Steps to Clinical Problem Solving • Making the Diagnosis • Assessing the severity and/ or stage of the disease • Rendering a treatment based on the stage of the disease • Following the patient response to treatment Making the diagnosis • Careful evaluation of the gathered data: – History – Investigations Involving in many instances: -GIGO -Putting the pieces of the puzzle in their right place • Making a short list of Differential Diagnosis Assessing the severity and / or stage of the Disease • Determining how bad the disease is • Sometimes there is no ‘mild or severe’ yet the disease may be in itself a risk for another condition: – Bacterial vaginosis Treating based on the stage • PET at 32 weeks gestation – Mild – Severe • Urinary Tract Infection – Lower urinary tract – Upper urinary tract Following the response to treatment / expectant management • Based on clinical judgment • Based on laboratory testing • Based on imaging techniques. However when you are solving a case on paper, it is a bit different… • 7 questions need to be answered – What is the most likely diagnosis? – What should be your next step? – What is the most likely mechanism for this process? – What are the risk factors for this condition? – What are the grade / severity and possible complications of this disease process? – What is the best therapy? Is there an alternative therapy (ies)? – How would you confirm the diagnosis What is the most likely diagnosis? • Means : The most common cause – Data presented may be confirming the diagnosis – Or they may be leading to another cause What should be your next step? • Depends on how much information is provided: – If enough: you will make the diagnosis Stage the disease and treat accordingly – No enough information More diagnostic tests – If he is providing treatment then the next step will be to follow the response • What is the likely mechanism for this process? – The pathophysiology of the disease itself – The disease may lead to another or to a complication • What are the risk factors for this disease process? – Are they present in the context – Do they mandate further testing / investigations. • What is the best therapy? – Do NOT jump to treatment on intuition – The treatment should be tailored according to: • Stage/ severity of the disease • The best possible alternative according to the patient characteristics • How would you confirm the diagnosis? – Making the point and concluding the story • A 48-year old G3 P3+0 woman complains of a 2-year history of loss of urine 4-5 times each day, typically occurring 2-3 seconds after coughing, lifting or sneezing, additionally, she notes dysuria and an urge to void during these episodes. These events causes her embarrassment and interferes with her daily activities. She is otherwise in good health. • A urine culture 1 month ago was negative. • On examination, – she is slightly obese, the BP is 130/80 and the HR is 80bpm and regular with a temp of 37˚C, her breast examination is normal and so were her abdominal examination. – A midstream urinalysis is unremarkable. What is your next step? What is the most likely Diagnosis? What is the best initial treatment? Bladder Control Problems Problems of: • Bladder Emptying • Bladder Storage Bladder Emptying Problems • Urinary Retention – Obstruction from within – Obstruction from outside – Stretch attenuation of the urethra – Bladder neck obstruction – Angulation of the urethra – Neurogenic causes [reflex from pain, retention with overflow] Image source: Virginia Urology Center Urinary Incontinence Definition: Urinary incontinence is uncontrolled leakage of urine causing hygienic and social problems. Urinary Incontinence is Common Among Older Adults Percentage of respondents in each age group 18 16 Men Women 14 12 10 8 6 4 2 0 5-14 15-24 25-34 35-44 45-54 55-64 65-74 75-84 >85 Age (years) Bladder Storage Problems • Overactive Bladder • Stress Incontinence • Mixed Incontinence • Overflow Incontinence •Fistulas Overactive Bladder Urgency Urge incontinence Frequency OVERACTIVE BLADDER Stress Incontinence Stress incontinence occurs when a small amount of urine escapes while the person coughs, sneezes, laughs, jumps or lifts something heavy. Stress Incontinence (a) Continent woman (b) Woman with stress incontinence External urethral sphincter Sudden increase in intra-abdominal pressure Overflow Incontinence Overflow incontinence happens when urine leaks from an overfilled bladder. Overflow Incontinence Mixed Incontinence Mixed incontinence occurs when a person has both the symptoms of urge incontinence and stress incontinence. Mixed Incontinence Sudden increase in intra-abdominal pressure Uninhibited detrusor contractions Prevalence • 8-51% in community • At least 50% in nursing homes • 25% suffer from severe incontinence • Greatest in older women and increases with age • Incontinence 6-10x greater in women than in men Impact on quality of life • Significant worldwide health problem • Affects 16 million women in US • Cost of diagnosing and managing UI exceed $26 billion annually in US • Adult diaper sales $5-6 billion/yr • Great social impact as well • Leaking depression stop exercise gain weight and so on …. Approach • Every woman is different • Consider quality of life from the patient’s point of view • History • Voiding diary • Quality of life assessment Normal Bladder Function • Functional urethra is intra-abdominal • Increased abdominal pressure transmitted equally to bladder and urethra • With increased stress urethro-vesical junction responds to stress by closing tight • Bladder is a voluntary smooth muscle • Inherent ability to maintain low pressure with filling-increase in volume:compliance Bladder Pressure-Volume Relationship Anatomy of Micturition • • • • • Detrusor muscle External and Internal sphincter Normal capacity 300-600cc First urge to void 150-300cc CNS control – Pons - facilitates – Cerebral cortex - inhibits • Hormonal effects - estrogen Interpretation of Post-Void Residual • PVR < 50cc - Adequate bladder emptying • PVR > 150cc- Avoid bladder relaxing drugs • PVR > 200cc- Refer to Urology • PVR > 400cc- Overflow UI likely Peripheral Nerves in Micturition • Parasympathetic (cholinergic) - Bladder contraction • Sympathetic - Bladder Relaxation – Bladder Relaxation (β adrenergic) – Sympathetic - Bladder neck and urethral contraction (α adrenergic) • Somatic (Pudendal nerve) - contraction pelvic floor musculature Peripheral Nerves in Micturition Factors Associated with Bladder Control Problems • Age • Childbirth • Gender • Menopausal Status • Surgery • Lifestyle • Medications • Concomitant illnesses Potentially Reversible Causes D I A P P E R S - Delirium - Infection - Atrophic vaginitis or urethritis - Pharmaceuticals - Psychological disorders - Endocrine disorders - Restricted mobility - Stool impaction 2 Medications That May Cause Incontinence • Diuretics • Anticholinergics - antihistamines, antipsychotics, antidepressants • Seditives/hypnotics • Alcohol • Narcotics • α-adrenergic agonists/antagonists • Calcium channel blockers 10 Warning Symptoms of Bladder Control Problems #1 Any leakage of urine 10 Warning Signs of Bladder Control Problems #2 Leakage of urine, regardless of amount, on coughing, sneezing, laughing or standing. 10 Warning Signs of Bladder Control Problems #3 Leaking urine on the way to the toilet. 10 Warning Signs of Bladder Control Problems #4 Bed wetting at any age over six years. 10 Warning Signs of Bladder Control Problems #5 An urgent need to pass urine, being unable to hold on. 10 Warning Signs of Bladder Control Problems #6 Passing urine more frequently than 8 times a day and only passing small amounts. 10 Warning Signs of Bladder Control Problems #7 Blood in the urine. 10 Warning Signs of Bladder Control Problems #8 Inability to urinate (retention of urine). 10 Warning Signs of Bladder Control Problems #9 Pain when passing urine. 10 Warning Signs of Bladder Control Problems #10 Progressive weakness of the urinary stream or a stream that stops and starts instead of flowing out smoothly. Image source: Malaysian Urological Association • A 48-year old G3 P3+0 woman complains of a 2-year history of loss of urine 4-5 times each day, typically occurring 2-3 seconds after coughing, lifting or sneezing, additionally, she notes dysuria and an urge to void during these episodes. These events causes her embarrassment and interferes with her daily activities. She is otherwise in good health. • A urine culture 1 month ago was negative. • On examination, – she is slightly obese, the BP is 130/80 and the HR is 80bpm and regular with a temp of 37˚C, her breast examination is normal and so were her abdominal examination. – A midstream urinalysis is unremarkable. What is your next step? What is the most likely Diagnosis? What is the best initial treatment? What is your next step? • Answer the question: What type of incontinence Does she have? – Perform cystometry • Conduct a pelvic examination: – Will the presence of proplase alter your decision regarding therapy? • The Q-tip cotton swab test has been used as a simple means of identifying patients with hypermobility of the urethrovesical junction. • A sterile Q-tip lubricated with xylocaine gel is placed in the urethra but not through the internal sphincterand the patient is asked to bear down. – If the Q-tip moves up more than 30°, the test is considered positive, and the patient may benefit from surgery • This means that the pressure in the bladder was transmitted to the Q-tip (i.e. exceeded the closing urethral pressure) Urodynamics • Indications – “complicated” incontinence – Pre-op – After failure of an anti-incontinence procedure Urodynamics • Components (a combo of any listed below) – Cystometry – study of bladder fxn – Pressure-flow study – bladder fxn during void – Videourodynamics – Uroflowmetry (study of flow rates) & PVR – Electromyography (EMG) – Urethral Pressure Profilometry – Ambulatory Urodynamics Cystometric Evaluation • Simple – After void, insert foley, measure PVR, <50cc. Attach syringe to foley, instill sterile saline. Normal first desire ~200cc. – Observe column of saline, unusual waves suggest detrusor dyssynergia. – Maximum bladder capacity ~500 cc. – Remove ~250 cc, remove foley, ask to cough, loss of urine suggests GSI. Bladder Pressure-Volume Relationship Stable Bladder Detrusor Instability Genuine Stress Incontinence Studies • Cystometry • Compliance, fd 90-150ml, nd 200-300ml, sd 400-550 ml, true subtracted detrusor pressures • Valsalva leak point pressure • Amount of intraabdominal pressure needed to leak • <60 cm H2O is ISD • Urethral pressure profile • Full bladder, catheter pulled along urethra • Urethral closure pressure >30 cm H20 nl, <20 is ISD • Uroflow • Rate and pattern of urine flow • Peak flow 20-30 ml/sec • Pressure flow test • Details voiding mechanism, obstructive dysfunction, poor contractility • Voiding detrusor pressure 10-30 cm H20 is nl • Electromyography • Electrical activity of pelvic floor musculature • Timing and degree of muscle relaxation impacts voiding mechanism Definition (based on urodynamic studies) Genuine Stress Urinary Incontinence (GSUI) • involuntary loss of urine with a rise in intraabdominal pressure in the absence of any rise in detrusor pressure • Urethral hypermobility Helpful hints • Stress induced detrusor instability – May be confused with GSI – See loss of urine after cough, but delayed – Bladder overactive after stress • Incontinence may only be seen in standing position • Correction of the cystocele may produce incontinence – UVJ is slightly kinked with cystocele and correction may reveal the econdition Treatment Options • • • • Reduce amount and timing of fluid intake Avoid bladder stimulants (caffeine) Use diuretics judiciously (not before bed) Reduce physical barriers to toilet (use bedside commode) 1 Treatment Options • Bladder training – Patient education – Scheduled voiding – Positive reinforcement • Pelvic floor exercises (Kegel Exercises) • Biofeedback • Caregiver interventions – Scheduled toileting – Habit training – Prompted voiding Pharmacological Interventions • Urge Incontinence – Oxybutynin (Ditropan) – Propantheline (Pro-Banthine) – Imipramine (Tofranil) • Stress Incontinence – Phenylpropanolamine (Ornade) – Pseudo-Ephedrine (Sudafed) – Estrogen (orally, transdermally or transvaginally) Other Interventions • Pessaries • Periurethral bulking agents (periurethral injection of collagen, fat or silicone) • Diapers or pads • Chronic catheterization – Periurethral or suprapubic – Indwelling or intermittant Pessaries Indwelling Catheter Surgery? • Bonney test: Gentle support of bladder neck during exam and asking patient to cough again • If continent, surgical repair is likely to be successful • Surgical repairs aim at elevation of bladder neck and correction of the pubovesical fascia tears Surgery is reported to “cure” 4 out of 5 cases, but success rate drops to 50% after 10 years. Surgical Procedures • Six basic surgical themes – Bladder buttress operations (anterior repair, etc) – Retropubic operations (Burch, MMK, etc) – Bladder neck suspensions (Raz, Stamey, Pereyra, etc) – Sling procedures (TVT, PV Sling, etc) – Periurethral Injections – Artificial urinary sphincter Bladder Buttress • Post-op continence rates are lower when compared to other procedures • Still in use for correction of cystocele and can be performed in conjunction with other incontinence procedures Retropubic Operations • Marshall Marchetti Krantz (MMK) cystourethropexy – 1949 – Para-urethral vaginal wall suspended to symphisis pubis • Burch colposuspension – 1961 – Para-urethral vaginal wall suspended to Cooper’s ligament • Paravaginal fascial repair – Para-urethral vaginal wall suspended to the tendinous arc on the pelvic sidewall Bladder Neck Suspensions • Pereyra • Stamey • Raz Sling Procedures • Suburethral sling is a strip of material that is tunneled underneath the bladder neck and/or proximal or midurethra and then attached to above structures such as rectus fascia or pelvic sidewall to create a posterior support, or “hammock effect” to the bladder neck and proximal urethra • Initially used for ISD (intrinsic sphincter deficiency), but now used for all kinds GSI Slings • Materials – Autologous fascia lata or rectus abdominis – Homologous materials (cadaveric fascia lata) – Synthetic Slings • Types of slings – Traditional suburethral (rectus abdominis) sling – Minimally invasive suburethral slings • Transvaginal bone-anchored sling (In-Fast, Vesica) • Tension free vaginal tape (TVT) – only sling placed at the midurethra • Initial results are encouraging, but long-term results are lacking TVT Operative Technique • • • • Abdominal incisions made Vaginal wall incision made Paraurethral dissection performed Trocar with tape advanced through vaginal incision, urogenital diaphragm, and retropubic space until its tip is brought out to the abdominal incision • Cystoscopy • Trocar and tape pulled through, tension is adjusted, and plastic sheath is removed • Abdominal and vaginal incisions are closed Periurethral Bulking Injection • Indicated for patients with stress incontinence who have: – Medical conditions that make them unfit for surgery – A history of partially successful treatment and wish to avoid more invasive procedures – Particularly indicated in patients with ISD Periurethral Bulking Injections • Purpose is to bulk up the tissue at the bladder neck in order to increase urethral closure pressure • Bulking agents – – – – – Collagen* Silicone Teflon Fat * Durasphere* (carbon beads in a carrier gel) *FDA approved bulking agents Artificial Urinary Sphincter • Indicated mainly in patients who have undergone recurrent previous surgery for GSI and have ISD • Few reports on this as first-line treatment, so results are difficult to interpret. • As high as 92% continence rate, but also a high revision rate of 17% Comparative Outcomes Procedure Category Retropubic Suspensions Transvaginal Anterior Suspensions Repair Sling Procedures Cure/Dry @ 48mo 84% 67% 61% 83% Cure/Dry/Improved @ 48mo 90% 82% 73% 87% De-Novo Urgency 11% 5% 5% 5% N/A N/A 7% 8% Intraoperative Complications 2% 2% 1% 3% Postoperative Complications 4% 7% 2% 7% Death 5/10,000 Retention (>4wks) Urge Incontinence • Loss of urine associated with uncontrollable urge to void • Uninhibited, involuntary detrusor contractions • Pressure-volume relation out of balance • Also called unstable bladder • Frequency • Urgency • nocturia • Chronic irritation due to infection, irritation or tumors Treatment • Primarily medical • Most commonly anticholinergics – Ditropan – oxybutynin chloride – Detrol – Imipramine – Levbid, cytospaz – hyoscyamine sulphate – Tolterodine (detrusitol) • Side effects- dry mouth, constipation etc. • Behavioral – Bladder retraining – Pelvic-floor rehabilitation Mixed Incontinence • Some degree of both stress and urge • More difficult to treat • Need to do complex urodynamic studies to determine major component • Precisely predict success with surgery • Surgery may worsen the urge component • Properly counsel patient Overflow Incontinence • Neurogenic bladder – Multiple sclerosis, spinal cord lesions, stroke – Diabetis – Trauma – Radical hysterectomy • Normal innervation absent or damaged • Loss of vesical reflexes and emptying sensation • Overdistended bladder with overflow • Complaints of fullness, pressure • Large bladder capacity • Absence of uninhibited bladder contractions • Treatment – medical – Cholinergics to increase tone and contractility • Urecholine- bethanechol • Prostigmine