Inflammation vivas - Improving care in ED
advertisement

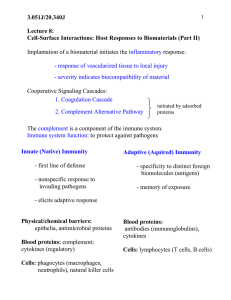
INFLAMMATION VIVAS 2011-2, 2010-2, 2008-2 What leukocytes types are characteristic of acute inflammation - Initially Neutrophils first 6-24 hours - Then replaced by monocytes 24-48 hours - Neutrophils may last longer (4 days) in pseudomonas - Lymphocytes in viral - Eosinophils in hypersensitivity How do leucocytes get to an area of acute inflammation Extravasation – 3 steps: 1. Margination of WCC in vessels, rolling and adhesion to endothelium (pavementing) (Selectins) 2. Transmigration and diapedesis across endothelium (PECAM1, CD31, Integrins) 3. Migration towards chemotactic stimulus in tissue (bacterial products, cytokines, IL8, C5A) Why do neutrophils predominate in the inflammatory response in the first 6-24 hours 1. More numerous in the blood 2. Respond more rapidly to chemokines, 3. May attach more firmly to adhesion molecules, especially those expressed early 4. Neutrophils are short lived - disappear after 24-48 hrs (monocytes live longer) What is the role of leukocytes in acute inflammation? 2010-2 1. Recognition and attachment to materials (opsonins) mediated by receptors 2. Killing of microbes: phagocytosis /engulfment /killing and degradation (H2O2-MPO-Halide) 3. Release of products – Amplify the inflammatory reaction (lysosomal enzymes, reactive oxygen/nitrogen) 2010-2, 2009-1, 2007-1, 2006-1, 2003-2 Describe the vascular changes in acute inflammation 1. Transient and brief vasoconstriction (lasting seconds) 2. Vasodilatation: opening of arterioles and capillary beds mediated by histamine and Nitric Oxide leading to increased blood flow 3. Increased vascular permeability with outpouring of protein-rich exudate 4. Stasis: due to PP permeability and increased viscosity – congestion of blood with margination of blood leukocytes What are the mechanisms of increased vascular permeability? - Contraction of the endothelial cells (histamine, bradykinin, leukotrienes, neuropeptide and substance P) called the immediate transient response, leading to inter-endothelial spaces - Direct vascular endothelial injury eg. in severe burns, microbial toxin injury, amplified by neutrophil activation, rapid onset but may last days - Leukocyte mediated leakage, in venules and pulmonary capillaries, long lasting for hours - Trancytosis increased Tx of fluid and protein thru endothelial cell, VEGF 2011-2, 2009-2 What are the characteristics of chronic inflammation - Prolonged process (weeks or more) in which active inflammation, tissue destruction and healing all occur together. Morphologic features: 1. Infiltration with mononuclear inflammatory cells - Macrophages - Lymphocytes - Plasma cells - (also eosiniphils, Mast cells and neutophils) 2. Tissue destruction 3. Attempts at healing by connective tissue replacement - Angiogenesis - Fibrosis What are the causes of chronic inflammation Causes: 1. Persistent infection by intracellular microbes of low direct toxicity (e.g. TB, viruses) 2. Immune reactions - Against own tissues especially i.e. auto-immune (RA, lupus) - Against host flora (e.g. inflammatory bowel disease) - Against benign environmental substance (allergies) 3. Prolonged exposure to potentially toxic substances - Exogenous (e.g. silica) - Endogenous (e.g. lipids -> atherosclerosis) Why does macrophage accumulation persist in chronic inflammation 1. Continued recruitment of monocytes due to continued expression of adhesion molecules and chemotactic factors) 2. Local proliferation of macrophages 3. Immobilisation of macrophages What products are released by macrophages in chronic inflammation 2009-2 - Products associated with tissue injury: Toxic O2 metabolites; Proteases (elastases, collagenases); Neutrophil chemotactic factors; Coagulation factors; AA metabolites; Nitric oxide - Products associated with fibrosis: Growth factors (PDGF, FGF, TGF): Fibrogenic cytokines; Angiogenesis factors (FGF); "Rem odelling" collagenases 2011-2 Describe the pathogenesis of Fibrosis Fibrosis = excess deposition of collagen & ECM in chronic disease 1. 2. 3. 4. Frustrated healing/chronic inflammation -> Persistent stimulus (infections, autoimmune, trauma) Macrophage/Lymphocyte activation -> Growth factors: especially TGF-, PDGF, FGF -> Proliferation of fibroblasts, endothelial cells, specifically fibrogenic cells Alternatively activated macrophages - by IL- 4, IL-13, cytokines from TH2 , Mast, eosinophils - produce TGF- - act to suppress microbicidal function, stimulate angiogenesis and scar formation - vs. classically activated by TH1 cells (IFN- and TNF) -> micobicidal and phagocytic TGF-β almost always involved: - Monocyte attractant (L/Mac) - Fibroblast activation/proliferation - Increased collagen fibronectin synthesis/secretion - Inhibition of metalloproteinases OPN (osteopontin) also important in recent studies Please provide some examples Cirrhosis, chronic pancreatitis, pulmonary fibrosis, pneumoconiosis, constrictive pericarditis, glomerulonephritis 2011-1 Which mediators of inflammation are derived from cells? Preformed - Vasoactive amines (Histamines, Serotonin) Newly synthesized - Arachidonic metabolites (Prostaglandins, Leukotrienes, Lipoxins) - Reactive Oxygen Species - Platelet activating factors - Nitric Oxide - Cytokines (TNF, IL1) - Chemokines Which cells release histamine? Widely distributed in tissues, richest sources: - Mast cells - Basophils - Platelets What are the effects of histamines in an inflammatory response? - Dilation of the arterioles - Increased vascular permeability of the venules - Can cause constriction of large arteries 2008-2, 2006-2 What is the complement system? - Plasma protein system involved in immunity against microbes Most important are C1-9 (more than 20 proteins) Synthesized by the liver, circulate in plasma as inactive precursors Activated by proteases, the activated fragments also proteases -> amplification cascade Describe the main pathways by which complement activation occurs C3 -> C3a and C3b is the most important step - Occurs in three ways: 1. Classical pathway – triggered by C1 binding to antigen-antibody complexes 2. Alternative pathway – in absence of antibody by microbial surface molecules (e.g. endotoxin), complex polysaccharides, or cobra venom 3. Lectin pathway – C1 activated by microbe carbohydrates – to manose binding lectins - C3a is released, C3b is bound - C3b (after combining with other complement fragments) cleaves C5 -> C5a and C5b How do activated complement products mediate acute inflammation? 1. Cell lysis – C5b binds late components (C6-9) -> membrane attack complex MAC, made from multiple C9 molecules -> hole in cell membranes 2. Inflammation - Vascular effects (vasodilation and increased permeability): C3a and C5a (anaphylatoxins) stimulate histamine release from mast cells - C5a activates the lipooxygenase pathway (arachidonate-> leukotrienes) - C5a is a powerful chemokine 3. Opsonisation – C3b (or iC3b) promotes phagocytosis by C3b receptors on neutrophils and macrophages