Anesthesia Medication Effects on Cerebral Hemodynamics

Anesthesia Medication
Effects on Cerebral
Hemodynamics
CBF:
CBF:
CBV:
CBF:
CBV:
ICP:
CBF:
CBV:
ICP:
Ischemia:
CBF:
CBV:
ICP:
Ischemia:
CBF:
CBV:
ICP:
Ischemia:
CBF: Site of autoregulation
CBV:
ICP:
Ischemia:
CBF: Site of autoregulation
Site of medication effects
CBV:
ICP:
Ischemia:
CBF: Site of autoregulation
Site of medication effects
CBV: Difficult to measure
ICP:
Ischemia:
CBF:
Site of autoregulation
Site of medication effects
CBV: Difficult to measure
Varies to a lesser degree than CBF
ICP:
Ischemia:
CBF: Site of autoregulation
Site of medication effects
CBV:
Difficult to measure
Varies to a lesser degree than CBF
ICP:
Brain Tissue, CSF,
CBV
Ischemia:
CBF: Site of autoregulation
Site of medication effects
CBV:
Difficult to measure
Varies to a lesser degree than CBF
ICP:
Brain Tissue, CSF, CBV
Ischemia: Focal vs global
Affects all variables
(MAP-ICP)= CPP
Resistance
MAP- ICP
Directly Proportional
Resistance
MAP- ICP
Directly Proportional
Resistance
Inversely proportional
MAP- ICP Metabolism
Resistance
Normal Values:
CBF:
Normal Values:
15-20% of CO
CBF:
Normal Values:
15-20% of CO
CBF:
Normal Values:
15-20% of CO
CBF:
50 mL/100g/min
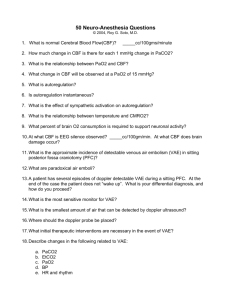
Questions
Question #1
In the normal patient, what is the largest component of the cranial vault?
A. Brain Tissue
B. CSF
C. CBV
D. MAP
Answer
Question #1: A) Brain Tissue
◦ The 3 components that make up the cranial vault are brain tissue, CSF, and CBV.
Brain tissue accounts for 80% of the space while CSF and CBV account for 10% each.
However, when ICP is altered it is typically caused by a change in CBV.
Question #2
Which of the following parameters is true for the normal patient?
A. 35% of cardiac output to the brain
B. Blood flow of 50 ml/min/100 g of brain tissue
C. ICP of 17 mmHg
D. Both A and B
Answer
Question #2: B) Blood flow of 50 ml/min/100 g of brain tissue
◦ Normal ICP is <15 and the brain normally receives
15-20% of cardiac output. The typical blood flow to the brain is 750 ml/min or 50 ml/min/100 g of tissue. Cerebral Ischemia begins when blood flow drops below 20 ml/min/100 g and infarct begins at
6 ml/min/100 g of tissue.
Question #3
All of the following increase CBF, except:
A. Hypercarbia
B. Hypoxia
C. Increased cerebral vascular resistance
D. They all increase CBF
Answer
Question #3: C) Increased cerebral vascular resistance
◦ Both hypercarbia and hypoxia increase CBF.
Hypoxia increases CBF by causing an increased metabolic demand. Hypercarbia has a direct vasodilatory effect on the cerebral vasculature. Increased cerebral vascular resistance would decrease CBF.
CBF Autoregulation
Overview
Intrinsic factors
Extrinsic factors
Ischemia
CBF Autoregulation
Overview
MAP 60-150
CBF Autoregulation
Overview
MAP 60-150
Rapid change will still affect CBF
CBF Autoregulation
Overview
MAP 60-150
Rapid change will still affect CBF
Disrupted by : volatile anesthetics
CBF Autoregulation
Overview
MAP 60-150
Rapid change will still affect CBF
Disrupted by : volatile anesthetics
HTN
CBF Autoregulation
Overview
Pt’s Baseline MAP
is the best indicator of their autoregulation range
CBF Autoregulation
Intrinsic Factors
Myogenic Response
CBF Autoregulation
Extrinsic Factors
PaCO2
CBF Autoregulation
Extrinsic Factors
PaCO2
Metabolism
CBF Autoregulation
Extrinsic Factors
PaCO2
Metabolism
CBF Autoregulation: Extrinsic
Factors
PaCO2:
Most potent vasodilator
CBF Autoregulation: Extrinsic
Factors
PaCO2:
Most potent vasodilator
Direct relationship to CBF
CBF Autoregulation: Extrinsic
Factors
PaCO2:
Most potent vasodilator
Direct relationship to CBF
CO2 Responsiveness Preserved with anesthetics
CBF Autoregulation: Extrinsic
Factors
Metabolism (CMRO2):
Main controllable factor intraop is temperature
CBF Autoregulation: Extrinsic
Factors
Metabolism (CMRO2):
Main controllable factor intraop is temperature: 7% change per 1 deg C
CBF Autoregulation
Ischemia
Focal vs Global
CBF Autoregulation: Focal
Ischemia
Cerebral Steal:
CBF Autoregulation: Focal
Ischemia
Cerebral Steal:
* Focal Ischemic areas are maximally dilated
CBF Autoregulation: Focal
Ischemia
Cerebral Steal:
* Focal Ischemic areas are maximally dilated
* Cerebral Vasodilation
CBF Autoregulation: Focal
Ischemia
Cerebral Steal:
* Focal Ischemic areas are maximally dilated
* Cerebral Vasodilation
Redirects blood flow away from ischemic areas
CBF Autoregulation: Focal
Ischemia
Inverse Steal:
CBF Autoregulation: Focal
Ischemia
Inverse Steal:
* Focal Ischemic areas are maximally dilated
CBF Autoregulation: Focal
Ischemia
Inverse Steal:
* Focal Ischemic areas are maximally dilated
* Cerebral Vasoconstriction
CBF Autoregulation: Focal
Ischemia
Inverse Steal:
* Focal Ischemic areas are maximally dilated
* Cerebral Vasoconstriction directs blood flow toward ischemic areas.
Questions
Question #1
In the normal person, cerebral autoregulation maintains a constant CBF between what MAP values?
A. 45-100 mmHg
B. 50-115 mmHg
C. 55-125 mmHg
D. 60-150 mmHg
Answer
Question #1: D) 60-150 mmHg
◦ While some sources have varying values of cerebral autoregulation, most have the low value of between 50 and 60 in the healthy patient.
Question #2
What is the most potent cerebral vasodilator?
A. PaO2
B. PaCO2
C. Isoflurane
D. Nitrous Oxide
Answer
Question #2: B) PaCO2
◦ While isoflurane and nitrous oxide are cerebral vasodilators, the most potent cerebral vasodilator is PaCO2. High PaO2 is a vasoconstrictor.
Question #3
In the case of focal ischemia, which of the following would be a desirable effect to reduce damage?
A. Vasodilation of non-ischemic tissue
B. Vasoconstriction of ischemic tissue
C. Vasoconstriction of non-ischemic tissue
D. None of the above
Answer
Question #3: C) Vasoconstriction of nonischemic brain tissue
◦ In focal ischemia a small area of brain tissue is receiving too little blood flow. The process of inverse steal involves vasoconstriction of nonischemic tissue and vasodilation of ischemic tissue.
CBF and Anesthetics
Inhaled Anesthetics
IV General Anesthetics
CBF and Anesthetics: Inhaled Anesthetics
CBF and Anesthetics: Inhaled Anesthetics
Decrease CMRO2 (except N2O)
CBF and Anesthetics: Inhaled Anesthetics
Decrease CMRO2 which CBF
CBF and Anesthetics: Inhaled Anesthetics
Are direct cerebral vasodilators which CBF
CBF and Anesthetics: Inhaled Anesthetics
Net effect determined by MAC
MAP- ICP Metabolism
Resistance
MAP- ICP Metabolism
Resistance
MAP- ICP Metabolism
Resistance
MAP- ICP Metabolism
Resistance
MAP- ICP Metabolism
Resistance
MAP- ICP Metabolism
Resistance
CBF and Anesthetics: Inhaled Anesthetics
Over 1 MAC, cerebral vasodilation greatly increases
CBF and Anesthetics: Inhaled Anesthetics
Over 1 MAC: cerebral vasodilation greatly increases
& autoregulation is impaired
CBF and Anesthetics: Inhaled Anesthetics
Over 1 MAC: cerebral vasodilation greatly increases
& autoregulation is impaired
CBF: Site of autoregulation
Site of medication effects
CBV:
Difficult to measure
Varies to a lesser degree than CBF
ICP:
Brain Tissue, CSF, CBV
Ischemia: Focal vs global
Affects all above variables
CBF and Anesthetics: Inhaled Anesthetics
Inhaled Anesthetics in normal patients with normal PaCO2 will cause minimal
ICP changes
CBF and Anesthetics: Inhaled Anesthetics
Inhaled Anesthetics in patients with reduced intracranial compliance can greatly increase CBV and ICP.
Questions
Question #1
A trauma patient comes into the OR with suspected head injury. Which volatile anesthetic would be least appropriate for anesthesia maintenance?
A. Sevoflurane
B. Isoflurane
C. Enflurane
D. Halothane
Answer
Question #1: D) Halothane
◦ All volatile anesthetics have the potential of increasing ICP, but halothane increases
CBF the most. Other volatile anesthetics would be more appropriate in this scenario.
Question #2
Which volatile anesthetic would increase CSF absorption?
A. Desflurane
B. Sevoflurane
C. Isoflurane
D. Volatile anesthetics do not increase CSF absorption
Answer
Question #2: C) Isoflurane
◦ Isoflurane is unique in that it is the only volatile agent that facilitates the absorption of CSF and has a favorable effect on CSF dynamics.
Question #3
Which of the following inhalation agents have been shown to increase ICP?
A. Nitrous oxide
B. Sevoflurane
C. Isoflurane
D. All of the above
Answer
Question #3: D) All of the above
◦ Nitrous has the potential to increase ICP substantially. The other volatile anesthetics increase ICP as well, but not to the same degree as nitrous.
Question #4
During global ischemia, what is a potentially beneficial effect that can be induced by volatile anesthetics?
A. An increase in CMRO2 with an increase in CBF
B. An increase in CMRO2 with a decrease in CBF
C. A decrease in CMRO2 with an increase in CBF
D. A decrease in CMRO2 with a decrease in CBF
Answer
Question #4: C) A decrease in CMRO2 and an increase in CBF
◦ Volatile anesthetics can produce what is referred to as luxury perfusion, a reduced
CMRO2 with an elevated CBF. This can be particularly beneficial during global ischemia.
Question #5
Which anesthetic drug would decrease CMRO2 the most?
A. Isoflurane
B. Sevoflurane
C. Fentanyl
D. Meperidine
Answer
Question #5: A) Isoflurane
◦ The mechanisms by which iso, sevo, and des decrease CMRO2 is similar, but iso is the one that reduces CMRO2 the most.
CBF and Anesthetics
Inhaled Anesthetics
IV General Anesthetics
CBF and Anesthetics: IV General Anesthetics
CO2 responsiveness is preserved
CBF and Anesthetics: IV General Anesthetics
CO2 responsiveness is preserved
Unlike Inhaled Anesthetics, autoregulation is also preserved
CBF and Anesthetics: IV General Anesthetics
All Gen Anesthetics except
Ketamine reduce CMRO2, which reduces CBF
CBF and Anesthetics: IV General Anesthetics
Many also have direct cerebral vasoconstriction
CBF and Anesthetics: IV General Anesthetics
Many also have direct cerebral vasoconstriction
Global/ Near Global: Barbs, Propofol
Regional (Not Uniform): Etomidate
MAP- ICP Metabolism
Resistance
MAP- ICP Metabolism
Resistance
MAP- ICP Metabolism
Resistance
MAP- ICP Metabolism
Resistance
MAP- ICP Metabolism
Resistance
MAP- ICP Metabolism
Resistance
CBF and Anesthetics: IV General Anesthetics
Net Effect:
Substantial Reduction in CBF (30-
60%)…
CBF: Site of autoregulation
Site of medication effects
CBV:
Difficult to measure
Varies to a lesser degree than CBF
ICP:
CSF, CBV, Brain Tissue
Ischemia: Focal vs global
Affects all above variables
CBF and Anesthetics: IV General Anesthetics
Net Effect: Reduction in CBF (30-
60%) leads to smaller reduction in
ICP (10-20%)
CBF and Anesthetics: IV General Anesthetics
CBF 30-60%
CBV 20-40%
ICP 10-20%
CBF and Anesthetics: IV General Anesthetics with Hypocapnia
CBF 3060%
CBV 2040%
ICP 1020%
CBF and Anesthetics: IV General Anesthetics
But, in Normocapnia, if MAP falls below autoregulation range, cerebral vasodilation will increase.
Questions
Question #1
At anesthetic doses all of the following drugs would preserve cerebral autoregulation except:
A. Propofol
B. Sodium Thiopental
C. Sevoflurane
D. All preserve cerebral autoregulation
Answer
Question #1: C) Sevoflurane
◦ All volatile anesthetics impair cerebral autoregulation at anesthetic levels.
Barbiturates and propofol preserve it.
Question #2
Which of the following agents decreases both cerebral blood flow and cerebral metabolism in the normocarbic patient?
A. Halothane
B. Ketamine
C. Nitrous Oxide
D. Propofol
Answer
Question #2: D) Propofol
◦ Of the drugs on the list propofol is the only drug that decreases CBF and CMRO2.
Ketamine, halothane, and nitrous oxide all increase CBF.
Question #3
Ketamine increases which of the following?
A. CBF
B. CMRO2
C. ICP
D. All of the above
Answer
Question #3: D) All of the above
◦ Ketamine increases CBF, CMRO2, and ICP.
Question #4
Which statement best describes the reasoning for using barbiturates over etomidate for cerebral protection in focal ischemia?
A. Barbiturates have a more global reduction in CBF and CMRO2 than etomidate
B. Etomidate has a more global reduction in CBF and CMRO2 than barbiturates
C. Barbiturates have a more focal reduction in CBF and CMRO2 than etomidate
D. Etomidate has a more focal reduction in CBF and CMRO2 than barbiturates
Answer
Question #4: A) Barbiturates have a more global reduction in CBF and CMRO2 than etomidate.
Question #5
Barbiturates do all of the following except:
A. Decrease cerebrovascular resistance
B. Reduce cerebral blood flow
C. Reduce cerebral metabolic rate
D. Produce hypnosis
Answer
Question #5: A) Decrease cerebrovascular resistance.
◦ Like most other IV anesthetics, barbiturates increase cerebrovascular resistance by direct vasoconstriction as well as by decreasing
CMRO2.
References
Evers, A. S., and Maze, M. (2003). Anesthetic Pharmacology -- Physiologic Principles and Clinical
Practice. Churchill Livingston: New York.
Morgan, G.E., Mikhail, M.S., & Murray, M.J. (2005). Clinical Anesthesiology 4 th Ed. McGraw-Hill.
Stoelting, R. K., and Miller, R. D. (2007). Basics of Anesthesia 5 th Ed. Elsevier: Philadelphia.