File - SBVTS
advertisement

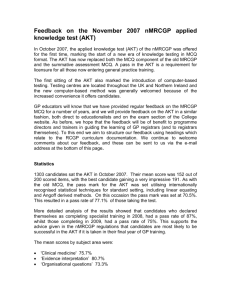
ST1 Induction Day The MAC Thursday 24.9.2015 Talk to your neighbour for a couple of minutes… • If you were suddenly to develop an illness that caused you to have regular contact with your GP, what sort of hurdles would you want to know that your GP had jumped, so that you could feel confidence in his / her ability to look after you competently and in an up-todate manner? Exams in training years • AKT – often done end of ST2 or early ST3 • CSA – usually done in ST3 • AKT – taken at Pearson Vue centre • CSA – taken at RCGP Context of exams • Miller’s Pyramid The 3rd exam…. • Or “the coursework” • WBA – the EP as a demonstration of competency and readiness for independent practice • Still needs to be deemed satisfactory for progression every 6m, for transition at end of each ST year, and for CCT Fees for exams • AKT – £489 • CSA - £1642 • WPBA – the price of your time! AKT – applied knowledge test • The Applied Knowledge Test is a summative assessment of the knowledge base that underpins independent general practice in the United Kingdom within the context of the National Health Service. • Trainees who pass this assessment will have demonstrated their competence in applying knowledge at a level which is sufficiently high for independent practice. What is the AKT? • The test takes the form of a three hour computerbased test consisting of 200 question items. • It is delivered three times a year at 150 Pearson VUE professional testing centres across the UK. • Approximately 80% of question items will be on clinical medicine, 10% on critical appraisal and evidence based clinical practice and 10% on health informatics and administrative issues. • All questions address important issues relating to UK general practice and focus mainly on higher order problem solving rather than just the simple recall of basic facts. Recent changes to AKT – from Oct 2014 • 1. Professor John Norcini, who conducted a review of the AKT, suggested that the RCGP should consider increasing the amount of time candidates have available to complete the AKT. Although there is no evidence that time constraints in the AKT contribute in any way to the differential pass rates, they might pose more of a challenge for those candidates who are less proficient in the English language. • The GMC gave permission to increase the duration of the AKT by 10 minutes on these grounds, and this came into effect in the AKT in October 2014. 2nd change • 2. In addition to the extra time, an on-screen calculator is now available. This is being provided at the request of candidates, but any calculation within the AKT will require only simple basic arithmetic, and most candidates will not need to use the calculator. • The additional time provided for the AKT will not change the standard required to achieve a pass in the AKT. When can you take the AKT? • The AKT can be taken during or after the ST2 stage of GP training. • A maximum number of four attempts will be permitted for those who have entered GP Specialty Training on or after 1 August 2010. Resources • Online question bank (e.g. Pass medicine, Onexamination) • AKT courses e.g. Emedica • AKT question books • Guidelines • BNF • Statistics books PDF on RCGP website • http://www.rcgp.org.uk/trainingexams/mrcgp-exams-overview Knowledge of basic statistical terminology including the following: • • • • • • • • • • • • • • • • • • • Absolute risk reduction (ARR) Meta-analysis Association Mode Bayesian probability Negative predictive value (NPV) Bias Nondirective interview Blinding Null hypothesis Case control Number needed to harm (NNH) Case fatality Number needed to treat (NNT) Cohort Odds & Odds Ratio Confidence intervals Positive predictive value (PPV) Confounding Prevalence 47AKT CONTENT GUIDE August 2014 Correlation Probability Crossover p-values Cross-sectional QALY (quality adjusted life year) DALY (disability adjusted life year) Randomised controlled trial (RCT) Data types (categorical, ordinal, continuous) Range Delphi Relative risk reduction (RR) Discrimination Reliability • • • • • • • • • • • • • • • • • • • Distributions (normal and non-parametric) Risk ratio Ethnography Risk reduction (RR) Event rate Sampling Focus group Sensitivity Generalisability Specificity Grounded theory Standard deviation (SD) Hazard Ratio Standardised mortality rates and ratios Incidence Systematic review Inclusion/exclusion criteria Trends Inductive reasoning Triangulation Likelihood ratios Type 1 and 2 errors Mean Validity Median Basic inferential statistical concepts to enable clinical interpretation of results from common statistical tests used for parametric data e.g: o Bayesian probability [Candidates would not be expected to be able to conduct these tests.] o t-tests, analysis of variance, multiple regression) and non-parametric data (e.g. chi squared, Mann-Whitney U) Research design • Qualitative research and quantitative research: – – – – – • The hierarchy of design and the advantages and disadvantages of study designs including: – – – – • Differences in forms of research and when each is appropriate Techniques such as pilot studies, questionnaire design, field observations, interviews, focus groups and analysis of transcripts of narrative material, ethnography and observation, action research, case study; consensus methods such as Delphi or nominal groups systematic reviews and meta-analysis; experimental: randomised controlled double blind quasi-experimental: non-randomised control group; observational: cohort (prospective, retrospective), case-control, cross-sectional The most appropriate research design to examine the hypothesis proposed in prospective and retrospective studies: – the limitations and strengths of research methodologies – knowledge of the “hierarchy of evidence” ranging from case reports through case control and cohort studies to randomised controlled trials and systematic reviews and meta-analyses Lethargy A 50-year-old man has become increasingly tired and lethargic over the past six months and has developed erectile dysfunction. His wife comments that he looks tanned even in the winter months. His serum ferritin and transferrin levels are significantly raised, but his haemoglobin is normal. Which is the SINGLE MOST likely diagnosis? Select ONE option only. A. Addison’s disease B. Chronic active hepatitis C. Diabetes mellitus D. Haemochromatosis E. Hypothyroidism Visual disturbance A 20-year-old woman notices bright lines of light in both visual fields followed shortly afterwards by a partial loss of her vision. Her visual symptoms resolve after one hour but she has slight nausea. Which is the SINGLE MOST likely diagnosis? Select ONE option only. A. Acute glaucoma B. Migraine C. Optic neuritis D. Retinal detachment E. Vitreous detachment Drug dose calculation A three-year-old girl has recurrent urinary tract infections and the paediatricianhas recommended trimethoprim prophylaxis at a dose of 2 mg/kg at night. She weighs 12.5 kg and trimethoprim suspension is available as 50 mg/5mls. What volume of suspension (in mls) should the child’s mother give her every evening? Type your answer in the following text box. Use figures NOT words. Percentages and fractions are NOT acceptable. Disorders of glucose metabolism A. B. C. D. E. F. G. H. Gestational diabetes Impaired fasting glycaemia Impaired glucose tolerance Maturity Onset Diabetes of the Young (MODY) Normal Prediabetes Type 1 diabetes Type 2 diabetes For the patient described, select the SINGLE MOST likely diagnosis from the list of options. A 47-year-old overweight woman had a screening blood test because of her family history of type 2 diabetes. Her result is as follows: HbA1c 40 mmol/mol A 15-year-old obese boy has significant glycosuria on more than one occasion. He is well with no symptoms. His father and brother both have diabetes. Random blood glucose 12 mmol/L Blood ketones negative Consent for disclosure of medical information Which TWO of the following statements are the MOST APPROPRIATE considerations when providing information to third parties such as insurers? Select TWO options only. A. B. C. Disclose all information written in the medical record Do not disclose the content of the report to your patient Ensure the patient has sufficient information about the likely consequences of disclosure D. Relevant information can be withheld under certain circumstances E. Use the proforma provided by the third party F. Patient consent can be automatically assumed by receipt of the insurers’ request Statistics from April 2015 – 1487 candidates sat AKT Scores in AKT 24 ranged from 89 to 184 out of 200 questions with a mean overall score of 72.9%. The mean scores by subject area were: – ‘Clinical medicine’ 74.0% (160 questions) – ‘Evidence interpretation’ 76.5% (20 questions) – ‘Organisational’ 60% (20 questions) The pass mark was set at 134 - pass rates as below: All Candidates 1487 74.4% ST2 First time takers ST3 First time takers 1058 82 81% 74.4% Our record Here in S Bham we have some very high achievers on the record E.g. we gained the top marks (>90%) in AKT at the last 2 sessions No pressure! CSA – Clinical Skills Assessment • The CSA is a summative assessment of a doctor’s ability to integrate and apply clinical, professional, communication and practical skills appropriate for general practice. • Simulating a typical NHS surgery clinic the CSA assesses a range of scenarios from general practice relevant to most parts of the curriculum which can also target particular aspects of clinical care and expertise. RCGP – 30 Euston Square Inside….. CSA – type of OSCE • Morning or afternoon exam • 13 x 10mins consultations, with a break between 7 & 8 • Role player and examiner enter room, candidate stays in room • May be a telephone triage or home visit scenario CSA room Equipment • You should bring your doctor’s bag containing the usual diagnostic equipment with you, including: • BNF • BNF for children • Stethoscope • Ophthalmoscope • Auroscope • Thermometer • Patella hammer • Tape measure • Peak flow meter and disposable mouthpieces (N.B. These must be EU standard) • Please note that there is no need to bring a sphygmomanometer CSA - marking • • • • • • Marked by 13 different examiners Marked in 3 domains of equal weighting: Data gathering Clinical management Interpersonal skills Feedback given, and breakdown of marks for scenarios Resources for CSA • • • • • • Books of case scenarios CSA cards Joint surgeries / video analysis w trainer Courses Feedback from COTs Practice with people who have recently passed! • Pennine VTS website cases CSA May 2015: Results summary 550 candidates sat CSA examinations during eight days in May. 358 candidates were successful resulting in an overall pass rate of 65.1%. 40.5% (223) of the candidates were sitting the examination for the first time, the pass rate for this particular group being 73.1%. The mean score for the entire cohort was 77 out of 117 with the highest mark on this occasion being 109, which was achieved by a candidate sitting the examination for the first time. A further 11 candidates scored 100 marks or more, 10 of whom were making a first application. Of the lowest scoring candidates, 11 obtained overall scores of 20 marks or more below the passing threshold for the day on which they sat the examination, and all but two of this group were re-sitting. Name of Patient: John Major Description of the patient & instructions to simulator: • John is 56, married with two children who have now left home. He developed foot drop 5 years ago and was diagnosed as having MS. Over the years his foot drop and gait have become worse. He was a keen walking until this. His neurologist recommended physio which has not helped, a leg brace which was a ‘nightmare’ (caused more trouble that it was worth) and then functional electrical stimulation but this has been no help. He struggles to walk any distance as he has to lift his foot high resulting in an abnormal gait. He was reading in the Daily Mail about a new medication called ‘Wundercin’ in which a chap with MS and foot drop was transformed by this new medication. In the article that chap was able to go back to fell walking just after three months! It said in the Daily Mail that it had been through a number of trials, all showing the same results. You have booked an appt with your GP to see if you can start ‘Wundercin’. • SH – Married, non smoker, 14 units per week of alcohol. Retired last year (early retirement) from teaching. Frustrated but not depressed with disability. • PMH – Foot drop & MS • DH – none • Allergies none • Ideas- Wundacin might help his foot drop • Concerns – It might not be funded in Pennine • Expectations – GP will know something about it and might prescribe it Name & age of patient John Major 56 Summary Card • PMH: MS and foot drop • DH: None • Allergies: None • BP/BMI/ Non smoker Case Notes - Last few entries in records: • Upset that FES had not helped his foot drop – rev prn • Patient Name: John Major • Examination findings: Foot drop CSA Case Marking Sheet Case Name: John Major Case Title: The unknown drug Context of case How a GP deals with a request for a drug unknown to him 1. Data-gathering, technical and assessment skills Positive descriptors: • Finds out what the patients knows about MS and the symptoms he has. • Identifies what impact the foot drop has caused • Explores prior treatments he has had • Explores the content/details of the article, what was said in the article re benefits, risks, numbers in the trial etc • Identifies ICE: Ideas - Wundacin might help his foot drop. Concerns – it might not be funded in Pennine. Expectations – GP will know something about it & might prescribe it Negative descriptors: • Fails to explore patients knowledge and personal experience of MS • Fails to find out what was in the article • Fails to identify psychosocial impact of MS • Fails to identify ICE 2.Clinical Management Skills Positive descriptors: • Identifies patients knowledge re ‘Wundercin’ • GP admits lack of knowledge • Agrees on what the patient might do e.g. drop off the article/find out more. • Agrees with the patient what the GP might do e.g. Read the article the patient drops off, ‘google’ the drug, phone local neurologist, speak to the lead pharmacist etc • Shares with the patient that the outcome may indicate that a) it may not be available, b) the risks may out weight the benefits c) If available may require him to see his neurologist • Arranges to see the patient with the outcome Negative descriptors: • Unable to identify a suite of options • Unable to come to a shared management plan • Fails to safety net 3. Interpersonal skills Positive descriptors: • Explores ICE with sensitivity • Establishes and maintains rapport • Expresses sympathy for his position • Able to come to a mutually agreed management plan. Negative descriptors: • Dismissive about the article • Not sympathetic with his situation • Failure to establish and maintain rapport • Doctor centred approach Other aspects ….. e.g. time keeping, consultation structure, comment on consultation skills etc Positive descriptors: Negative descriptors: Lucinda Smythe Description of the patient & instructions to simulator: • 17 year old. Living with mum and dad. Doing A levels and hoping to go to University. • Opening line – “I want to start the pill”. - In a ‘stable’ relationship for last 6/52 with boyfriend, also 17. Not using any contraception and not used any previously. • LMP 5/52 ago, last unprotected intercourse 3/52 ago. • No contraindications for the pill, no previous STIs or related symptoms. Non smoker. • Real reason for attendance – she thinks she is pregnant – do not mention this unless directly asked about LMP/pregnancy/concerns. • • • • Ideas – she might be pregnant Concerns - she might be pregnant and if so mum will go ballistic and it will destroy her University aspirations Expectation – Preg test and if negative – the pill but if positive a Termination of Pregnancy. When other methods of contraception mentioned quickly refuse as needle phobic, not interested in coil or having something in your arm, friend had patches, they just fell off. Solely wanting contraceptive pill. Lucinda Smythe - 17 year old female Summary Card • PMH: None • DH: None • Allergies: None • BP/BMI/ ?smoking and alcohol hx: Not known (as infrequent attender) Case Notes - Last few entries in records: • Jan 2006 – pain in left ear, temp – otitis media, conservative management. Lucinda Smythe Examination findings: • Pregnancy test negative • BP 124/78 • BMI 24 Case – Lucinda Smythe Case Title: Contraception Context for the Case: • Using Ideas (I might be pregnant) Concerns (If I’m pregnant mum will go ballistic) and Expectation (a pregnancy test and if that ok the cocp) to explore reason for attendance • Sharing preg test & safe sex & contraceptive options • Clear explanation of chosen option Data gathering, technical and assessment skills Positive descriptors: • Clear structure to consultation • Good history, covering relevant points – sexual hx, STIs, LMP, unprotected intercourse etc • Using ICE to focus consultation Negative descriptors: • Not eliciting full history or taking sexual history • No structure shown • ICE not explored Clinical Managemnent Skills Positive descriptors: • Gaining consent for PT • Examination – BP, BMI • Clear explanation , S/E, missed pills etc • Safety netting, review dates explained Negative descriptors: • Starting pill without full history, examination or exploring ICE. • Not sharing options • Confusing explanations, no safety netting Interpersonal Skills Positive descriptors: • Emphathic and non judgemental approach • Using ICE to find out real concern Negative descriptors: • Judgemental attitude Global comments • Positive descriptors: • Well structured consultation, history, ICE, examination, shared options, safety netting • Use of leaflets to reinforce explanation • Negative descriptors: • Not taking full history or not finding out real concerns. • Starting medication inappropriately Look at … • http://pennine-gp-training.weebly.com/csacase-scenarios.html WPBA • Think of it as “the coursework” • You don’t have to rely on memory for it, and it is relatively easy to do well if you follow guidance and engage with it • A GP who knows the academic stuff but is not a team player or does not get on well in a practice situation is going to struggle Any questions?