Page 6 in the second box the fourth point
advertisement

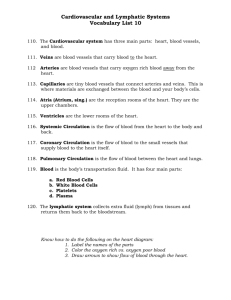
Quick review: Last lecture we discussed tissue blood flow and why it should be strictly autoregulated. Each tissue should receive the minimal amount of blood needed. Our heart is incapable of pumping the maximal blood volume needed constantly to all tissues due to the insufficiency of blood volume. We also said that each tissue blood flow is influenced according to its metabolic state. ( There is a linear relationship between the rate of metabolism and the rate of blood flow as you can see in figure 17-1) Remember also that O2 content is a key regulator of blood flow to different tissues. ↓ O2 ↑ Blood flow. ↑ O2 ↓ Blood flow. Auto-Regulation of tissue blood flow It is the ability of each tissue to control its own local blood flow in proportion to its metabolic needs. There are two theories explaining this phenomenon: 1. Vasodilator theory Different vasodilator substances are released in the circulation in response to decreased tissue blood flow. Scientists used to believe that this theory is derived by one sole vasodialator but lately they founded that many vasodialator enforce an accumulative effect all together. Those substances are: CO2 , Adenosine, H+, K+, Histamine, ADP compounds, Bradykinins, prostacyclins and NO. - Bradykinins: are peptides converted from kinins by the effect of kallekrein enzymes. Those are activated by laceration of tissue or by increase in metabolic state. - Prostacyclin (PGI2) : one of the prostaglandins converted from arachidonic acid ( 20 Carbon fatty acid with 4 d.bonds) by the effect of the enzyme prostacyclin synthase . - EDRF: endothelium derived relaxing factor – Nitric Oxide. In simple: Increase of tissue metabolism increase of vasodilators decreased arteriolar resistance increased blood flow. 1|Page 2. Oxygen lack theory: When there’s a deprivation of O2 ( in high need for oxygen) , this lack of oxygen is sensed in tissues especially around the capillaries, this drives a vasomotor effect towards opening of more capillaries. ( pre-capillary sphincter relaxes). Auto-Regulation of blood flow when the arterial pressure changes Tissues “sometimes” auto regulate their blood supply regardless of arterial pressure. We expect that when pressure decreases, blood flow will decrease accordingly then vasodilators will be released. What really happens is that within limits ( 60-180 mm Hg) the blood flow stays constant where pressure changes. ( doctor said this is very important for different events in the circulation, will be explained later). 2 points of view have been proposed in attempt to explain this theory: 1. Metabolic theory: Dr. says its mainly due to the release of local vasodilators. ( Book relates it more to the oxygen content of a tissue), explanation is not really clear. 2. Myogenic theory: less supported than the first one. States that when pressure decreases there are less stretching forces on the vessel wall vessel relaxes decrease in resistance flow increases Otherwise, when the pressure increases there is too much stretching of smooth muscles of the vascular wall this stretch tends to open Ca+ channels influx of calcium smooth muscles contracts pressure increases again. This is a positive feedback cycle which is incompatible with life ( our aim is to reduce P when its increases, not to exacerbate the condition) still, this theory is adapted by some scientists. Laplace law: Tension = P X Radius If pressure is increased, tension icreases and the radius is decreased. Laplace law explains the myogenic theory. 2|Page Long-Term theories to keep blood flow proportional to metabolic rate 2 more theories: 1. Collateral circulation theory: opening of collaterals ( as in MI). MI in elderly is not fatal because most collaterals are open at this age, its has severe outcomes in adults due to the lack of collaterals. 2. Angiogenic theory ( increase in vascularity) Doctors explains it the simple way ( no need for details) Oxygen deprivation stimulates angiogenesis more formation of blood vessels. Example on the angiogenic theory: A Female undergoes a preterm delivery (baby born before pregnancy reaches its full term) The supervisor doctor decided to put the baby within an incubator and supply him with 100% oxygen because due to his (the Dr.) evaluations the baby is having respiratory distress due to the absence of surfactants ** Surfactants are secreted during the last days of 3d trimester (short before delivery) the baby was born before gestation is complete surfactants deffecient. 2 weeks later baby was discharged. Mother came back a month later complaining the babys visual capabilities are impaired. Explaination : ** the retinal vessels weren’t yet mature when he was delivered ( they completely mature after pregnancy) ** O2 decrease is the stimulus for angiogenesis. When the dr. gave 100% oxygen to the baby, he delivered an amount of oxygen that is capable of suppressing angiogenesis and maturation of the retinal vessels. When the baby was out of the incubator (exposed to outer environment oxygen concentration ~20% ) angiogenesis started massively and went unregulated reterolental hyperplasia. ** incubator oxygen supply should be gradually decreased ( 90, 80 , 70 …) until reaching the regular environmental o2 concentration. Remember: collateral vessels are found in every human among all ages, but they are usually closed ( open when an obstruction is present.) Now doctors goes through vasodilator and vasoconstrictor substances. (should be memorized). 3|Page Auto-regulation of skeletal muscles A person’s metabolic rate is high during exercise, this causes the release of different vasodilators vasodilatation increase in blood flow. *Skeletal muscle is regulated by local means* A 2nd type of regulation may take over: the extrinsic sympathetic stimulation which eventually causes vasoconstriction decrease in blood flow Overall, the local factors overcome the extrinsic effect. Net outcome Vasodilatation. Tissue blood flow during exercise is increased by one of two mechanisms: 1. Active hyperemia when exercising the skeletal muscle blood flow increases accordingly. ↑Exercise ↑ Blood flow 2. Reactive hyperemia If a cuff is wrapped around the arm of a patient and then its inflated until preventing blood to reach the lower part of the arm and the palm local vasodilators released in attempt to adapt the decreased blood flow. Then, the cuff is rapidly removed there is a tremendous instantaneous increase of blood flow to overcome the decrease that took place before (reactive). Same concept applies for a thrombus in coronary arteries, which blocks the blood passage leading to release of vasodilators. If the thrombus is removed vast increase of blood flow. This will lead to the well known phenomenon: REPERFUSION INJURY (same as reactive hyperemia) ** the more the vessel is obstructed, more severe is the injury. Isotonic and Isometric contraction in skeletal muscles: Isotonic: shortening of muscle. Blood flow graph goes up and down as you can see. Explaination: shortening of muscle is due to contraction which actuates a pressure over the vessels decrease of blood flow. (when the muscle relaxes blood flows back normally) rythmatic increase and decrease of blood flow 4|Page Isometric: no shortening occurs. Permanent contraction presses the vessels, blood flow decreases and vasodialator substances. When the muscles relaxes reactive hyperemia. Now we’ll talk about different circulations and their regulation in brief: Skin and GIT are neurally regulated. Brain is regulated by local mechanisms. Lungs: will be discussed later. Heart: mainly local (remember the coronary thrombus example) Heart is also regulated by extrinsic means: sympathetic vasoconstriction parasympathetic vasodilatation e.g. ↑ sympathetic tone ↑ Heart rate ↑ contractility ↑ metabolic rate release of vasodilators (especially adenosine, bradykinins and NO) net effect is vasodilatation. Again, the vasadilatory effect overrides the neurogenic (sympathetic) effects. Remember that this theory hold true within certain limits, when the sympathetic system is vigorously stimulated cardiac ischemia will occur. Pulmonary circulation: Pressure in the LV is 0-120 mm Hg LA is 5 mm Hg RV is 0-25 mm Hg RA is 2 mm Hg MAP is ~ 100 mm Hg (systemic) MAP is ~ 15 mm Hg ( pulmonary) You don’t have to memorize those number, they are introduced to explain this concept: 1st remember that the Cardiac output (CO) = MAP / TPR The CO is the same and doesn’t change in regular resting condition, MAP are different so the Resistance should be different as well. The resistance in the pulmonary circulation is only 1/6 of that in the systemic circulation. 5|Page Auto-Regulation in lungs In most of our body tissues high levels of CO2 cause vasodilatation while high O2 levels cause vasoconstriction. The absolute contrary takes place in the lungs. More O2 in the lungs lead to more blood flow towards the lung for gas exchange purposes. ↑ O2 ↑ Vasodilatation of the pulmonary vessels. Intraalveolar O2 / CO2 are the key regulators for dilatation/constriction in pulmonary vessels respectively. Auto-Regulation in Heart Regulated chiefly by local vasodilators. During systole the ventricles are contracted pressing the coronary arteries, they receive less blood and release vasodilator substances accordingly vasodilatation In early parts of diastole there’s an increase in blood flow too ( but more than systole) this is mainly witnessed in the LV due to high blood needs. This is very important to know when it comes to Aortic regurgitation . During Aortic regurgitation the diastolic pressure is low decrease of blood flow to the heart. When coronaries are occluded, cardiologist use either: Bypass operations: preferred when theres a minimal occlusion of 3 vessels. Angioplasty (or stent insertion) : preferred when there are 1-2 obstructed vessels. Slides of edema, starling law … are shown rapidly – left for self studying. Done By: 3asem Z. Abu-Shtaya Dedicated to the soul of M.A.S 6|Page Corrections on sheet 17 physiology CVS Special thanks to Mahmoud Madi ــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ 1. Page 3 in the box the second point: increased MSFP will take the curve of venous return (on Y-axis) and RAP (on X-axis) upward and to the RIGHT 2. Page 3 just below the box: INCREASED compliance decreased MSFP decreased venous return decreased CO. N.B.: I can't find a strong relationship between the diameter of the blood vessel and its compliance. However, the largest the artery, the more compliant it is (according to a previous sheet) 3. Page 3 Under the title "Autonomic Supply of…etc" The sympathetic nervous system does NOT supply the capillaries unlike what is written in the sheet 4. Page 4 in the first box: Aortic baroreceptor Vagus nerve (X) Carotid baroreceptor Hering's nerves of the glossopharyngeal (opposite to what is written in the sheet) 5. Page 6 in the second box the fourth point Constriction of the arterioles more TPR LESS venous return ـــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــــ It is a quite large number of mistakes. Sorry for that and I hope that my next sheet will be much better! Thanks for everyone who commented on the sheet. Abdullah M. Abukar 7|Page