BBP Presentation
advertisement

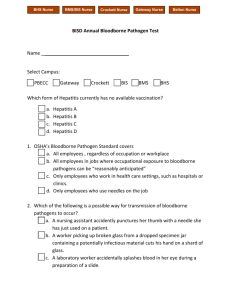
Bloodborne Pathogens Awareness Training 1 Introduction This is an awareness level course that will provide general information on bloodborne pathogens to help minimize serious health risks to people who may be exposed to blood and other potentially infectious materials. Version 1 2 Course Agenda Section 1: Bloodborne Pathogens: General Information, Regulations, Transmission, and Exposure Section 2: Exposure Control Plan and Compliance Methods Section 3: Hepatitis B Vaccination and Post-Exposure Follow-Up Section 4: Labeling, Training, and Recordkeeping Version 1 3 Section 1 Bloodborne Pathogens: General Information, Regulations, Transmission, and Exposure 4 Bloodborne Pathogens Bloodborne pathogens pose a potential risk to approximately 8 million U.S. workers in health care and other areas of the workforce OSHA’s Bloodborne Pathogens standard, published in Title 29 of the Code of Federal Regulations 1910.1030 prescribes safeguards to protect these workers against exposure to bloodborne pathogens and other potentially infectious materials (OPIM) and reduce the risk from exposure Version 1 5 What is a bloodborne pathogen? Bloodborne pathogens (BBPs) means pathogenic microorganisms that are present in human blood and can cause disease in humans. These pathogens include, but are not limited to, hepatitis B virus (HBV), hepatitis C virus (HCV), and human immunodeficiency virus (HIV) Blood means human blood, human blood components, and products made from human blood Other potentially infectious materials (OPIM) such as other body fluids contaminated with visible blood Version 1 6 Definition of OPIM Other potentially infections materials (OPIM) also include the following human body fluids: semen, vaginal secretions, cerebrospinal fluid, synovial fluid, pleural fluid, pericardial fluid, peritoneal fluid, amniotic fluid, saliva in dental procedures, any body fluid that is visibly contaminated with blood, and all body fluids in situations where it is difficult to differentiate between body fluids. It also includes any unfixed tissue or organ (other than intact skin) from a human (living or dead) and HIV- or HBV-containing culture medium or other solutions, and blood, organs, or other tissue from experimental animals infected with HIV or HBV. Version 1 7 Regulations Issued in 1991, OSHA’s Bloodborne Pathogens standard, published in Title 29 of the Code of Federal Regulations 1910.1030, is part of the Occupation Safety and Health Act of 1970 (OSH Act) under the US. Department of Labor Updated in January, 2001 (changes effective April, 2001) as a result of the Needlestick Safety and Prevention Act issued in November 2000 Includes additional guidelines for HIV and HBV research laboratories and production facilities Many states administer their own occupational safety and health programs through plans approved under the OSH Act Version 1 8 Bloodborne Pathogen Standard Summary Establish an Exposure Control Plan Use engineering controls Enforce work practice controls Provide personal protective equipment Make Hepatitis B vaccinations available Provide post-exposure follow-up Use labels and signs to communicate hazards Provide information and training to employees Maintain employee medical and training records Version 1 9 OSHA Enforcement Inspection Penalties/Sanctions – – – – – Serious Violation Other-Than-Serious Violation Willful Violation Repeated Violation Failure to Correct Prior Violation Compliance Assistance Version 1 10 Who is covered by the standard? The standard applies to all employees who may reasonably anticipate occupational exposure to blood or other potentially infectious materials (OPIM). “Good Samaritan” acts such as assisting a coworker with a laceration or nosebleed would not be considered occupational exposure. If an employer designates and trains employees to render first aid or medical assistance as a part of their job duties, they are covered by the protections of this standard. Version 1 11 Why is protection so important? Bloodborne pathogens have the potential to cause serious illness and death. These pathogens include, but are not limited to: – Hepatitis B Virus – Hepatitis C Virus – Human Immunodeficiency Virus (HIV) Prevention is the best method of protection against exposure to bloodborne pathogens Version 1 12 Transmission of Bloodborne Pathogens Transmission of bloodborne pathogens in the occupational setting is primarily through percutaneous (needlestick/sharps) or mucous membrane exposure to infected blood and body fluids Version 1 13 Hepatitis B Virus Infection A serious liver disease that can cause lifelong infection, cirrhosis (scarring) of the liver, liver cancer, liver failure, and death Symptoms can include: – Jaundice, fatigue, abdominal pain, loss of appetite, nausea, vomiting, joint pain – About 30-40% of people infected with HBV have no signs or symptoms Transmission – By percutaneous (needlestick/sharps) or mucous membrane exposure to blood and body fluids infected with HBV (acute or chronic HBV) Incubation period 45 to 180 days (avg. 60-90 days) Can live on a dry surface for at least 7 days and still be capable of causing infection Version 1 14 Hepatitis C Virus Infection A serious liver disease that can lead to long-term infection, chronic liver disease, cirrhosis (scarring of the liver), liver cancer, and death Symptoms can include: – Jaundice, fatigue, dark urine, abdominal pain, loss of appetite, nausea – About 80% of people infected with HCV have no signs or symptoms Transmission – By percutaneous (needlestick/sharps) or mucous membrane exposure to blood and body fluids infected with HCV (acute or chronic HCV) Incubation period is 6 to 7 weeks Limited data on survival of HCV in the environment Version 1 15 HIV Infection HIV is the Human Immunodeficiency Virus that causes AIDS; many people with HIV infection will develop AIDS as a result Symptoms may include: – Rapid weight loss; dry cough; recurring fever or profuse night sweats; profound and unexplained fatigue; swollen lymph glands in armpits, groin, or neck; diarrhea lasting >1 week; white spots/blemishes on the tongue, mouth, throat; pneumonia; red, brown, pink, or purplish blotches on or under skin or inside the mouth, nose, or eyelids; memory loss, depression, and other neurological disorders Transmission – By percutaneous (needlestick/sharps) or, infrequently, mucous membrane exposure to blood or body fluids containing blood infected with HIV HIV antibody usually develops within 6 months of exposure Does not survive well outside the body—environmental transmission is remote Version 1 16 What is Exposure? Occupational Exposure means reasonably anticipated skin, eye, mucous membrane, or percutaneous contact with blood or other potentially infectious materials (OPIM) that may result from the performance of an employee’s duties Exposure Incident means a specific eye, mouth, or other mucous membrane, non-intact skin, or percutaneous contact with blood or OPIM that results from the performance of an employee’s duties Version 1 17 Who is at risk for exposure? Employers are responsible for determining the hazard risk for exposure to bloodborne pathogens in their company – Assistance in determining a hazard risk in your company is available through OSHA Examples of who may be at risk: – Nurses, physicians, emergency personnel (emergency room employees, paramedics, EMTs), and other healthcare workers, especially those providing first-response medical care – Laboratory and blood bank technologists and technicians – Dentists and other dental workers – Law enforcement personnel and firefighters – Houskeeping personnel and laundry workers – Medical waste treatment employees – Medical examiners and morticians Version 1 18 How can exposure happen? The most common means of exposure is from percutaneous injuries (through the skin) with contaminated sharps (needles and scalpels) (82%) Contact with mucous membranes of the eyes, nose, or mouth (14%) Exposure of broken or abraded skin (3%) Human bites (1%) Version 1 19 How can exposure be prevented? Universal Precautions – Treat all blood and body fluids as potentially infectious Immunization with the Hepatitis B Virus Vaccine Engineering Controls – Safer medical devices for medical procedures and sharps disposal Work Practice Controls – Safer techniques for medical procedures – Personal Protective Equipment (PPE) Appropriate barriers such as gloves, gowns, eye and face protection Version 1 20 Section 1 Q & A Any questions on information covered in this section? Version 1 21 Section 2 Exposure Control Plan and Compliance Methods 22 Exposure Control Plan Each employer must establish an Exposure Control Plan (ECP) to eliminate or minimize employee exposures Must be written Must be reviewed annually and updated, as necessary, to reflect changes in: – Technology that will help eliminate or reduce exposure – Employee tasks, assignments, procedures which affect exposure Annually document that employer has considered and implemented safer medical devices (if feasible) – Employers must solicit input from frontline workers (potentially exposed) in identifying, evaluating, and selecting engineering controls Plan must be accessible to employees Version 1 23 Exposure Control Plan Exposure Determination – Identify worker exposure to blood or OPIM – Review all processes and procedures with exposure potential – Re-evaluate when new processes or procedures are used Exposure determination must be made without regard to the use of personal protective equipment Version 1 24 Engineering and Work Practice Controls Employer Responsibility: Review/evaluate available engineering controls (safer medical devices) at least annually – Document review/evaluation in ECP Review new devices and technologies at least annually – Must solicit input from non-managerial employees in the selection of controls – Document review in ECP Version 1 25 Engineering and Work Practice Controls Employer Responsibility: Implement engineering controls/devices as appropriate – Document evaluation and implementation in ECP – Controls must be used if they reduce employee exposure either by removing, eliminating, or isolating the hazard Train employees on safe use and disposal – Document in ECP Train employees to use current and new devices and/or procedures – Document in ECP Version 1 26 Compliance Methods Universal Precautions Engineering and Work Practice Controls Personal Protective Equipment Housekeeping – Laundry – Regulated Waste Version 1 27 Universal Precautions OSHA’s required method of control to protect employees from exposure to all human blood and OPIM Refers to a concept of bloodborne disease control which requires that all human blood and certain human body fluids are treated as if known to be infectious for HIV, HBV, HCV and other bloodborne pathogens Must be observed in all situations where there is a potential for contact with blood or OPIM Intended to prevent percutaneous, mucous membrane, and non-intact skin exposure to bloodborne pathogens Version 1 28 Engineering Controls Primary methods used to control transmission of bloodborne pathogens Controls that reduce employee exposure to bloodborne pathogens in the workplace by isolating or removing the hazard from the workplace – Sharps disposal containers – Self-sheathing needles – Safer medical devices Sharps with engineered sharps injury protections Needleless systems OSHA does not approve or endorse any medical device product Version 1 29 Work Practice Controls Controls that reduce the likelihood of exposure by altering the manner in which a task is performed – Handwashing After removing gloves As soon as possible after exposure Use of gloves does not eliminate the need for handwashing! – Needle and Sharps Safety Do not recap needles with 2-handed technique Do not bend or break sharps Use appropriate containers for disposal or re-use – Perform procedures involving blood or OPIM to minimize splashing, spraying, spattering and generation of droplets – No food or smoking in work areas Version 1 30 Personal Protective Equipment Specialized clothing or equipment worn by an employee for protection against potentially infectious materials General work clothes (e.g., uniforms, pants, shirts or blouses) not intended to function as protection against a hazard are not considered to be personal protective equipment (PPE) Employers must provide “appropriate” PPE at no cost to employees Version 1 31 Personal Protective Equipment PPE must be properly used, cleaned, decontaminated, laundered, repaired, and disposed of at no cost to employees – The manufacturer’s instructions for use, cleaning, and decontamination must be followed in order for PPE to remain effective Must be removed when leaving the area or upon contamination with potentially infectious materials – DO NOT take PPE home to launder, clean, or disinfect Version 1 32 Personal Protective Equipment Examples of PPE: – – – – Gloves Gowns, Aprons, Laboratory Coats Surgical caps, hoods, shoe covers Face shields or masks and eye protection – Mouthpieces, resuscitation bags, pocket masks, or other ventilation devices Version 1 33 Housekeeping Ensure that the worksite is maintained in a clean and sanitary condition Determine and implement an appropriate written schedule for cleaning and method of decontamination based upon: – – – – Location within the facility Type of surface to be cleaned Type of soil present Tasks or procedures being performed in the area Version 1 34 Housekeeping Work surfaces must be decontaminated with an appropriate disinfectant: – After contact with blood or OPIM – Completion of procedures – Immediately or as soon as feasible with obvious contamination or after any spill of blood or OPIM – At the end of the work shift Version 1 35 Laundry Handle contaminated laundry as little as possible using appropriate PPE Place and transport in labeled or colorcoded bags or containers at the location where used – Wet laundry with potential for leakage must be placed and transported in bags or containers that prevent leakage of fluids to the exterior No sorting or rinsing at location where used Version 1 36 Regulated Waste Liquid or semi-liquid blood or OPIM Contaminated items that would release blood or OPIM in a liquid or semi-liquid state if compressed Items that are caked with dried blood or OPIM and are capable of releasing these materials during handling Contaminated sharps Pathological and microbiological wastes containing blood or OPIM Version 1 37 Regulated Waste Must be placed in closeable, leakproof containers built to contain all contents during handling, storing, transporting, or shipping and be appropriately labeled or colorcoded Close prior to removal If outside contamination of the regulated waste container occurs, it should be placed in a second container that meets the above requirements Version 1 38 Regulated Waste Additional requirements for discarding and containing contaminated sharps: – Discard immediately or as soon as feasible – Containers must be puncture resistant and leak-proof on sides and bottom – During use, sharps containers should be Easily accessible to personnel in the immediate area where sharps are used/found Maintained upright throughout use Replaced routinely and not be allowed to overfill Version 1 39 Section 2 Q & A Any questions on information covered in this section? Version 1 40 Section 3 Hepatitis B Vaccination and Post-Exposure Follow-up 41 Hepatitis B Vaccination Employers must make the Hepatitis B Vaccine available to all employees at risk of exposure: – – – – Within 10 working days of initial assignment Free of charge At a reasonable time and place Vaccination must be performed by or under the supervision of a licensed healthcare professional The following are exceptions: – Employee has had the vaccination – Antibody testing reveals immunity – Vaccine is contraindicated for medical reasons Version 1 42 Hepatitis B Vaccination Employees who decline vaccination must sign a declination form Employers must provide the vaccination to Employees who decline and then at a later date decide to accept the vaccination Employers cannot require employees to participate in an antibody prescreening program in order to receive the vaccination Employers must provide a booster dose(s) of the vaccine if it is recommended by the US Public Health Service at a future date Version 1 43 What happens if an exposure occurs? Wash exposed area with soap and water Flush splashes to the nose, mouth or skin with water Irrigate eyes with water, saline, or sterile irrigants Report the exposure Seek the assistance of a health care professional to determine what follow-up actions or treatment may be needed Version 1 44 Post-Exposure Follow-up Employer must immediately make available to the employee a confidential medical examination and followup Document date and time of exposure Document routes of exposure and how the exposure occurred Identification of the source individual (if feasible and allowable by applicable laws) – Obtain consent from source individual for blood to be tested as soon as feasible (unless there is a known HBV or HIV infection) – Results to be made available to the exposed employee Obtain exposed employee’s consent for blood to be collected and tested as soon as feasible Version 1 45 Post-Exposure Follow-up Record injuries from contaminated sharps in a sharps injury log Provide risk counseling and offer post-exposure protective treatment for disease, when recommended by a healthcare professional in accordance with current US Public Health Service guidelines Provide written opinion of findings to employer and copy to employee within 15 days of the evaluation Version 1 46 Section 3 Q & A Any questions on information covered in this section? Version 1 47 Section 4 Labeling, Training, and Recordkeeping 48 Biohazard Warning Labels Warning labels must be predominantly fluorescent orange or orange-red with lettering and symbols in a contrasting color Warning labels are required for: – Containers of regulated waste – Refrigerators and freezers containing blood or OPIM – Other containers used to store, transport or ship blood or OPIM Red bags or red containers may be substituted for labels Version 1 49 Training Employers must ensure that all employees with occupational exposure participate in a training program – Provided at no cost and during working hours – Provided at the time of initial assignment to tasks with occupational exposure (and at least annually) – Provide additional training when existing tasks are modified or new tasks are required which affect the employee’s potential exposure Maintain training records for 3 years Version 1 50 Training Elements Copy of the standard with explanation of the contents Epidemiology and symptoms of bloodborne disease; modes of transmission of bloodborne pathogens Exposure Control Plan specific to the site Recognition of hazards Use of engineering controls, work practices and PPE Exposure Incidents and Post-exposure follow-up Labels/signs/color coding Opportunity for live question and answer session Version 1 51 Recordkeeping Medical Records Medical Recordkeeping for Employee Exposure must include: – Employee’s name and social security number – Employee’s hepatitis B vaccination status – Results of all examinations, medical testing, and follow-up procedures – Copy of information provided to the healthcare professional – Employer’s copy of the healthcare professional’s written opinion Version 1 52 Recordkeeping Medical Records Employee medical records: – Must be kept CONFIDENTIAL – Not disclosed or reported to any person within or outside the workplace without the employee’s written consent (unless required by law and/or this regulation) – Maintained for the duration of employee’s employment plus 30 years Version 1 53 Recordkeeping Training Records Training Record maintenance is required for 3 years from the training date. The following information must be included: – Dates of the training – Contents or summary of the training – Names and qualifications of persons conducting the training – Names and job titles of all persons attending the training Version 1 54 Recordkeeping Sharps Injury Log Employers must establish and maintain a sharps injury log to record injuries from contaminated sharps The log must be maintained in a way to ensure employee privacy The log must at a minimum contain: – Type and brand of device involved in the incident – Location where the incident occurred – Explanation of how the incident occurred Requirement applies to any employer who is required to maintain a log of occupational injuries and illnesses under 29 CFR 1904 Version 1 55 Section 4 Q & A Any questions on information covered in this section? Version 1 56 Summary OSHA’s Bloodborne Pathogens Standard is intended to provide safeguards to protect workers against the health hazards from exposure to blood and other potentially infectious materials (OPIM) and to reduce the risk from exposure – Create a safer work environment through the use of engineering and work practice controls – Reduce the risk of exposure by the proper use of personal protective equipment and through proper housekeeping and waste handling and disposal – Provide guidance on handling an exposure incident Implementation of this standard is expected to prevent hepatitis B cases and significantly reduce the risk of occupationally-acquired HIV, hepatitis C, and other bloodborne pathogens Version 1 57 Q&A Any questions on any information covered in this course? Test your knowledge of Bloodborne Pathogens….. Version 1 58 References 29 CFR 1910.1030 Bloodborne Pathogens OSHA’s website at: http://www.osha.gov CDC website at: http://www.cdc.gov NIOSH website at: http://www.cdc.gov/niosh/topics/bbp/ Version 1 59 Where to Get More Information Regional OSHA office for Pennsylvania (Region III, DE, DC, MD, PA, VA, WV): Regional Office U.S. Department of Labor/OSHA The Curtis Center-Suite 740 West 170 S. Independence Mall West Philadelphia, PA 19106-3309 TELE: (215) 861-4900 FAX: (215) 861-4904 Pittsburgh Area Office Federal Office Building, Room 1428 1000 Liberty Avenue Pittsburgh, Pennsylvania 15222-4101 (412) 395-4903 (412) 395-6380 FAX Version 1 60