BBP Training slides - USC Administrative Operations
advertisement

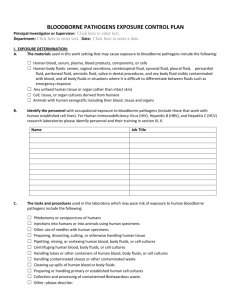
University of Southern California Bloodborne Pathogens Training USC Environmental Health and Safety **For annual refresher training ONLY (initial training must be taken in class) Outline Objective Introduction to Bloodborne Pathogens Epidemiology and Symptoms Modes of transmission Case Reports Preventive methods Summary Objective To inform USC healthcare workers (HCW), students, staff and other personnel about: Occupational risk, vaccination program, exposure control plan, etc. Comply with OSHA Bloodborne Pathogen Standard 29 CFR 1910.1030 & CCR Title 8, section 5193 Cal-OSHA BBP Std. Guide Comply with CA Medical Waste Management Act Safety Code, Sections 117600-118360 Bloodborne Pathogens Microorganisms that are present in human and non-human primate blood and can cause disease in human: Transmitted by blood or other bodily fluids/tissue via: HBV, HCV, HIV most prevalent (Herpes B, Malaria & Syphilis) contaminated sharps, mucosal exposure, or exposure with non-intact skin Needlestick – HBV ~30% risk of transmission, HCV 1-10%, HIV ~.3% Hepatitis B has been the most frequent laboratory-acquired viral infection, with a rate of 3.5–4.6 cases per 1000 workers. Any laboratory personnel who collects or handles tubes of blood is vulnerable Exposure to Blood: What Healthcare Personnel Need to Know, http://www.cdc.gov/ncidod/dhqp/pdf/bbp/Exp_to_Blood.pdf Disease characteristics Hep B – Acute: liver inflammation, cold/flu-like symptoms and vomiting. Chronic: cirrhosis, liver cancer, death Hep C – many cases asymptomatic, mostly chronic infection, liver transplant HIV – once immunocompromised, succumb to opportunistic infections(CMV, Pneumocystis pneumonia) Occupationally acquired HIV among healthcare personnel 1981-2006 Occupation Documented Possible Nurse 24 35 Clinical Laboratory Worker 16 17 Nonsurgical Physician 6 12 Non-Clinical Laboratory Technician 3 - Housekeeping or Maintenance 2 13 Dentist or Dental Worker - 6 Other healthcare occupation - 6 Surveillance of Occupationally Acquired HIV/AIDS in Healthcare Personnel, as of December 2006, http://www.cdc.gov/ncidod/dhqp/bp_hcp_w_hiv.html Needlesticks ~85% occupationally acquired HIV 600K-800K injuries annually Half are estimated to be unreported. Most needlesticks due to poor work practices Preventable Panlilio AL, et al. Infect Control Hosp Epidemiol, 2004 Tasks that may put you at risk Phlebotomy Handling containers of blood, fluid, tissue, or cultures Pipetting, mixing, or handling blood, fluid, tissue Using finger stick device for blood testing Using capillary tube Providing injections Cleaning blood or broken contaminated glass Handling medical waste Assisting diabetic patient with blood glucose monitoring Performing first aid or CPR Finding improperly discarded needle An introduction to Bloodborne Pathogens in the Pharmacy, https://webapp.walgreens.com/cePharmacy/viewpdf?fileName=blood_borne_pathogens.pdf Case Report Controlling Risk Risk Assessment Universal precautions Engineering controls, work practice controls, personal protective equipment Proper Waste Disposal Disinfection Risk Assessment Process What is Risk? A measure of the likelihood that a loss will occur (probability) and its potential seriousness (severity) Risk Assessment Process (I.A.M) Identify the hazards Assess the potential impact of the hazards Manage the potential impact of the hazards through risk reduction strategies: (Engineering, Administrative, PPE) Engineering controls Biosafety Cabinet (BSC) Safety-engineered sharps must be used, such as self-retracting needle, hinged cap needle Proven to reduce number of needlestick injuries Plastic capillary tubes/ aspirating pipettes Biosafety Cabinets (Engineering Controls) BSC work practices: 1. Disinfect working area with appropriate disinfectant and contact time. 2. Do not block front or back grilles 3. Divide BSC’s working area into: clean, working and dirty areas. 4. Work from clean to dirty area 5. Have only items needed for procedures *Do not overcrowd BSC 6. Minimize rapid movements inside BSC: *Move arms in and out slowly (minimize sweeping motion) 7. Disinfect thoroughly at the end of experiment. * UV light is not recommended Potential Risk of Using Glass Pasteur Pipettes Work practice controls No recapping of needles Place sharps container as close to you as possible, don’t exceed fill line Immediately dispose of medical waste When using sharps, focus on task at hand Practice before using device on patients Practice good hand hygiene (soap and water, alcohol based hand sanitizer) Hand Hygiene Frequently missed areas Personal Protective Equipment Gloves for any vascular access(latex alternatives), remove carefully to minimize contamination of hands, wash hands afterwards Lab coat/scrubs Eye and face protection when splash potential Closed-toe shoes Working with commercial blood bank samples? Samples are tested for Hepatitis B core antigen Hepatitis B surface antigen Hepatitis C virus HIV 1 & 2 A, B, O and Rh • • • • • Samples are NOT tested for • • • • • Eastern Equine encephalitis virus (EEEV) St. Louis encephalitis virus (SLEV) West Nile Virus (WNV) Brucellosis Others Hazardous Waste Disposal Biomed PATHOLOGICAL SOLID PHARMACEUTICAL SHARPS Chemotherapy Waste Hierarchy + + + + + + Decontamination of Biohazardous Liquid Waste Decontaminate tissue and media with 10% bleach solution with a 30 minute contact time Flasks must be emptied and surfaces must be decontaminated at the end of a shift Disinfection 1-10% household bleach 70% Ethanol Make 10% solution weekly for effectiveness Not suitable for non-enveloped viruses Sani-wipes Must be EPA approved Labeling Place International biohazard symbol on: Biohazardous waste Door signs Incubators Freezers Refrigerators Shipping boxes Any equipment use for biological samples Handling, storage, transport procedures Specimens must be placed in a container which prevents leakage during collection, handling, processing, storage, transport, or shipping (use secondary container), container must be labeled with biohazard symbol Hep B Vaccination Recombinant vaccine Anti-cancer Anaphylaxis rare Contact EH&S for more information and forms: 323-442-2200 or IBC@admin.usc.edu **In-class training required to obtained vaccination form Handling Exposures Wash affected area with soap and water, if mucosal exposure, rinse with water/saline Report immediately and seek medical evaluation (Internal Medicine, White Memorial after-hours) Counseling, baseline testing, test source if possible, possibly initiate PEP, schedule follow-up testing various timepoints up to 1 year Post exposure prophylaxis HBV: HBIG + vaccine if unvaccinated HIV: Standard Antiretroviral Therapy (ART) antiretrovirals, 2 or 3 drug expanded regimen depending on type of exposure (percutaneous vs. mucosal), status of the source, bodily fluid HCV: Rivavirin & pegylated-interferon alpha-2b. In summary Practice safe techniques • • • • • • Use safety-engineered sharps Dispose of needles into sharps containers Don’t recap needles Wear gloves, lab coat/scrubs, closed-toe shoes Good hand hygiene Follow post-exposure procedures Exposure control plan Cal-OSHA BBP & Exposure Control Plan info: http://www.dir.ca.gov/dosh/dosh_publications/bbpbest1.pdf Internal Medicine (HCC II) and White Memorial Hospital References Cal OSHA Bloodborne Pathogen Standard, http://www.dir.ca.gov/title8/5193.HTML Surveillance of Occupationally Acquired HIV/AIDS in Healthcare Personnel, as of December 2006, http://www.cdc.gov/ncidod/dhqp/bp_hcp_w_hiv.html Panlilio AL, et al. Infect Control Hosp Epidemiol, 2004 Exposure to Blood: What Healthcare Personnel Need to Know, http://www.cdc.gov/ncidod/dhqp/pdf/bbp/Exp_to_Blood.pdf An introduction to Bloodborne Pathogens in the Pharmacy, https://webapp.walgreens.com/cePharmacy/viewpdf?fileName=blood_borne_pathogens.pdf Aoun, H.: When a house officer gets AIDS. N Eng J Med 321(10):693-696, 1989. FDA Safety Alert: Hepatitis B Transmission via Spring-loaded Lancet Devices http://www.fda.gov/downloads/MedicalDevices/Safety/AlertsandNotices/PublicHealthNotifications/ucm063124.pdf NIOSH Alert: Preventing Needlestick Injuries in Health Care Settings, 1999