File
advertisement

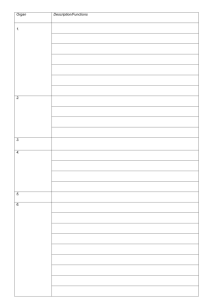
HANDOUT FOR PELVIC FLOOR AND BOWEL CONTINENCE PELVIC FLOOR Pelvic Floor: Formed by the pelvic diaphragm Funnel-shaped Muscular partition from the pubis to the coccyx and from lateral wall to lateral wall Separates pelvic cavity from perineum inferiorly Transmits urethra, vagina (in females) and anal canal Muscles of Pelvic Floor: The pelvic diaphragm is composed of two paired muscles o Levator ani o Coccygeus Levator ani muscle o Paired muscle o Principal muscle of pelvic floor o Supports pelvic contents o Actively maintains position of pelvic viscera Perineal body or central perineal tendon o A fibromuscular body extending from the perineum into the urogenital hiatus o The site of numerous muscle attachments in the perineum o perineal body is essential for the integrity of the pelvic floor, particularly in females o Components of the levator ani muscle Pubococcygeus Is anterior part of levator ani Main contributor to the levator ani Arises from the posterior body of the pubic bone and anterior part of the arcus Tendineus Runs posteriorly to attach to the anococcygeal ligament and the coccyx o Iliococcygeus Posterior part of the levator ani Is thin and poorly developed Arises from the posterior part of the arcus tendineus and the ischial spine Attaches to the anococcygeal raphe and the coccyx o Puborectalis is innermost and merges with the external anal sphincter. Unites with its partner to make a Ushaped sling around the rectum at its junction with the anus . Has a sphincter-like action by pulling the anorectal junction forward and contributing to anal continence. It causes 120 deg angulation of anorectum due to the pull against the pubic bones. By its action it also shuts the lumen by apposing the post and the side walls of rectum Pubococcygeous and iliococcygeous help to close the urogenital diaphragm by voluntary contraction, as well as elevate, straighten, steady, and suspend the rectum. The perineal body helps in the suspending action. A thickened band of muscle best seen inferior to the pubococcygeus Coccygeus muscle o o o o Reinforces pelvic floor posteriorly Arises from ischial spine Inserts on lower two sacral and upper two coccygeal segments Blends with sacrospinous ligament on its external surface Innervation of the levator ani and coccygeus muscles o Levator ani innervated by branches from the anterior rami of S3–S4 spinal nerves o Puborectalis also innervated by branch of pudendal nerve (S2,3,4) o Coccygeus supplied by branches of the anterior rami of S4–S5 spinal nerves Functions of the levator ani o Acting together raise the pelvic floor to increase abdominal pressure, such as when coughing, sneezing, urinating, defecating, lifting heavy objects. o Important in voluntary control of micturition (urinating) o Supports pelvic viscera o Supports head of the fetus NOTES ON BOWEL CONTINENCE EXTERNAL ANAL SPHINCTER: Superficial external sphincter Deep external sphincter – continuous with the puborectalis Subcutaneous part with the corrugate cutis ani INTERNAL ANAL SPHINCTER Circular layer of rectum becomes internal anal sphincter Continence during sleep and rest is by the continuous tonic contraction of the internal sphincter Continence during raised intra abdominal pressure is by the levator ani and the external sphincter The external anal sphincter and puborectalis muscles are innervated by the pudendal nerve The levator ani receives innervation from both the internal pudendal nerve and direct branches of S3- S5 Sensory innervation to the anal canal is provided by the inferior rectal branch of the pudendal nerve Rectum is relatively insensate, the anal canal below the dentate line is sensate. Supportive structures for continence: 1. Perineal body 4 muscles 2 paired, 2 unpaired Superficial transverse perinei, deep transverse perinei (paired) Arching fibers of the puborectalis around the rectum+fibers of bulbospongiosus (unpaired) 2. Anorectal angle 3. Rectal ampulla 4. Mucosal valves Neural organization of anorectal sphincters: Somatic from S2,3,4 (pudendal nerve) to the external anal sphincter Sympathetic from L2,3,4 (superior hypogastric plexus) Parasympathetic S2-4 (nervi erigentis also called pelvic splanchnic nerves) to the internal anal sphincter PELVIC PLEXUS- formed by sympathetic and parasympathetic nerves hypogastric plexus (by branches from the sacral part of the sympathetic chain)- sympathetic pelvic splanchnic nerves (also called nervi erigentes) - parasympathetic Pudendal nerve supplies to all 3 muscles of levator ani Nervi erigentis or pelvic splanchnic nerves or pelvic nerves - parasympathetic -distal most nerve fibers relay on to the ganglia of Auerbach's plexus -Sensory reflex of rectal distention Presacral sympathetic nerves - Motor to involuntary internal sphincter Physiologic coordination- responsible for continence: Sensory reflex + motor reflex + unique rectal contractions Fine control over defecation reflex Mucosa contains - Nerve endings for pain - Meissner's corpuscles for touch - Krause end organs for pressure - Pacinian corpuscles for friction - The relaxation of internal sphincter allows the contents to come in contact with the above sensory receptors - They are able to discriminate air vs solid fecal matter - The relaxation of external sphincter will occur if air is leading the flow – if one wants. Motor reflex involves: Tonic contraction of the internal anal sphincter Reflex contraction of the levator ani and external sphincter DEFECATION REFLEX Initiation by voluntary abdominal contraction, gastrocolic reflex, colonic reflex, direct rectal mucosal stimulation, rectal distention 1. Filling and distention of lower rectum Fecal material passes to rectum by the longitudinal muscular contraction. When there is distension in the sigmoid colon and rectum, the internal sphincter relaxes at the same time as the external sphincter contracts. This allows some of the fecal contents to enter the anal canal and be sampled by its sensitive epithelium to determine if its solid, liquid or gas. 2. Increase rectal pressure If the individual decides to continue with defecation, the intrarectal pressure increases on straining. Added pressure from abdominal straining or Valsalva maneuver aids defecation. Straining requires intact innervation of the lower thoracic cord T6-T12. The intraabdominal pressure should be sufficient to overcome the external sphincter which relaxes with the pelvic floor that causing the rectum to straighten up reducing the rectal angle. This increase in intraabdominal pressure forces stool into the rectum with relaxation of the extenal anal sphincter allowing defecation. 3. Stimulation of receptors in the pelvic floor – desire to defecate –relaxation of the internal sphincter 2 alternatives: 1. If not voluntarily inhibited, the external sphincter also relaxes resulting to defecation. Fecal matter stimulate the anal canal further relaxing the external anal sphincter. 2. No social opportunity, contraction of external anal sphincter and puborectalis occurs, the rectum relaxes and the urge to defecate passes—accommodation or adaptation of the rectum. If the individual decides not to continue with defecation, the rectum relaxes further to allow accommodation of the contents which further stimulates the external sphincter to contract, the rectum relaxes and the urge to defecate passes—accommodation or adaptation of the rectum HOLDING – Puborectalis, external and internal sphincters contract INITIATION – puborectalis and external anal sphincter relax, levator ani, abdominal and diaphragm contract COMPLETION – internal and external anal sphincters relax, rectum contracts Upper motor neuron lesion- damage above the defecation reflex center in the sacral cord Results to: 1. Abnormal storage of feces 2. Inability to recognize urge and distinguish contents 3. External sphincter dyssynergia Lower motor neuron lesion – damage within the reflex defecation center Results to: 1. Fecal retention 2. Oozing of stool through the flaccid sphincter 3. Sensory and motor pathways are disrupted so the patient is unaware of urge to defecate and unable to exercise voluntary external anal sphincter Assessment is through the bulbocavernosus reflex and the anal relfex to determine UMN or LMN lesions. The bulbocavernosus reflex is a palpable or visible contraction of the anal sphincter when pressure is applied to the glans penis or clitoris. When contraction is present, (+) result. This indicates that the reflex activity of the sacral cord is intact and therefore the SCI is an UMN lesion. Should be tested soon after SCI, before the spinal shock passes. The anal reflex is a visible contraction of the anal sphincter in response to a pinprick. A positive response indicates an UMN lesion.