Yersinia. Francisella. Brucella. Bacilli
advertisement

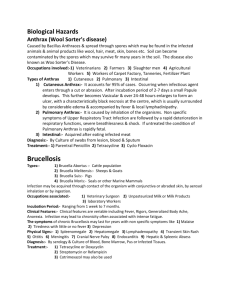
Chair of Medical Biology, Microbiology, Virology, and Immunology Yersinia. Francisella. Brucella. Bacilli. Prof. S. Klymnyuk Yersinia pestis belongs to Genus Yersinia which includes in family Enterobacteriaceae. The causative agent of plague, Yersinia pestis, was discovered by the French microbiologist A. Yersin in Hong Kong in 1894. Ukrainian scientists D. Samoilovich, D. Zabolotny and others contributed greatly to the study of the mechanisms of its transmission. The French microbiologists G. Girard and T. Robic obtained a live vaccine from the attenuated EV strain. Bubonic plague, caused by Y. pestis, is an ancient disease that has killed millions of people over the centuries. For example, it is believed to have killed more than 100 million persons in an epidemic in the sixth century. Another epidemic in the 14th century killed one fourth of the European population, and the London plague in 1665 killed more than 70,000 persons. In 1893, an epidemic began in Hong Kong and spread to India where more than 10 million individuals died over a 20-year period. Morphology. The plague bacillus, as seen in tissue smears, is ovoid-shaped. It is non-motile, forms no spores, and on solid media cultures is elongated in form. In preparations from tissues and cultures Y. pestis is found to have a delicate capsule. The organism stains with ordinary aniline dyes and gives a bipolar appearance, its ends staining more intensively. Y. pestis Cultivation. The optimum temperature for cultivation is 2530° C. On agar slants the culture forms a viscid translucent mucilaginous mass. On agar plates it forms colonies with turbid white centres and scalloped borders resembling lace or crumpled lace handkerchiefs. In meat broth the cultures form a pellicle on the surface with thread-like growth resembling stalactites and a flocculent precipitate. Sodium sulphite, fresh haemolytic blood, sarcinic extract, and live sarcina (“feeders”) are used as growth stimulators. They are of special value when the seeded material contains a small number of organisms. Differentiation of Yersinia Species adonitol arabinose arabitol arbutin sorbitol Production of Hydrogen sulphide xylose Carbohydrate fermentation Y. pestis – + – – + + + Y. pseudotuberculosis Y. enterocolitica + + – + – – – – + – + + + + Species Some diagnostic signs differentiating the bacteria of plague from those of pseudotuberculosis in rodents Yersinia pestis Yersinia pseudotuberculosis 1.Fresh strains do not usually 1. Fresh strains usually ferment rhamnose ferment rhamnose 2. Do not ferment adonite 2. Ferment adonite with the formation of acid 3. Do not ferment urea 3. Ferment urea 4. On desoxycholic citrate agar they grow with the formation of red colonies 4. On desoxycholic citrate agar they grow with the formation of yellow colonies 5. Are lysed by the plague phage to the titre 5. Do not undergo lysis Toxin production. Y. pestis is very virulent for humans. The important virulence factors of Y. pestis seem to be directed toward two goals for the organisms: (1) invasion and proliferation within host cells, and (2) resistance to killing by the host. The incredibly high fatality rate of bubonic plague is probably primarily because of septic shock resulting from the bacteremia occurring in the disease. Virulence factors that seem to be important in human disease. Factor Fraction 1 capsule V/W antigens Fibrinolysin Low Ca2+ response gene YOP H YOP K & L Apparent Function Antiphagocytic Suppress granuloma formation Tissue invasion YOP synthesis Protein tyrosine phosphatase Inhibit cell-mediated immune response Antigenic Makeup of Y. pestis Antigen Composition Function Protection Envelope (F1) A Soluble polysaccharideprotein Immunogen + B Soluble polysaccharidae Species-specific antigen – C Insoluble polysaccharidae Nonimmunogen – Antigen Antigenic Makeup of Y. pestis ComposiFunction tion Protection Somatic (O) 1 Unknown Virulence antigen + 3 Corresponds to F1 Species-specific antigen + 4 Heat-stable protein Nonimmunogen – 5 Heat-stable protein Shared with Y. pseudotuberculosis – 8 Heat-labile polypeptide Toxin - V Protein Associated with virukence inhibits phagocytosis + Antigenic Makeup of Y. pestis Antigen Composition Function W Protein Shared with Y. pseudotuberculosis Rough Heat-stable polysaccharidae Shared with Y. pseudotuberculosis Protection + – Pathogenicity for animals. Rodents, among them black rats, grey rats, mice, susliks, midday gerbils, tumarisks, and marmots (tarbagans) are susceptible to plague. More than 300 rodent species may spontaneously contract the disease. In addition, 19 rodent species are susceptible to laboratory infection with plague. Camels died in the Astrakhan steppes m 1911, and humans who ate camel meat contracted plague. Pigs, sheep, goats, donkeys, mules, dogs, cats, monkeys, and certain carnivores are susceptible to the disease in natural environments. However, little epidemiological importance is attached to them. 1. Reservoir: Fleas and wild rodents (ground squirrel, gerbil, marmot, cavy) 1. Reservoir: Rodents in contact with man (house rat, sewer rat) 2. Vectors: Fleas on infected rodents, flea i rodent burrows 2. Vectors: Fleas 3. Rodent – Flea – Rodent Bubonic palgue: Rat – Xenopsilla – Man Man – Pulex irritans – Man Hangling infected rodents 4. Wild Rodent to man – Sporadic 4. Sepicemic plague: Primary – human plague. Usually direct entry throgh mucose contact Secondary – complication of bubonic 5. Wild rodent – flea – domestic rodent 5. Pneumonic plague: Secondary – complication of bubonic 6. Domestic rodent – flea – man: human plague 6. Primary – droplet infection man – to – man The disease is transmitted by the bites of fleas (e.g., Xenopsylla cheopis, the rat flea) which have previously sucked blood from an infected animal. The ingested bacilli proliferate in the intestinal tract of the flea and eventually block the lumen of the proventriculus. The hungry flea, upon biting another rodent, regurgitates into the wound a mixture of plague bacilli and aspirated blood. Bubonic plague Immunity. After recovery from the disease a stable immunity of long duration is acquired. Realizing this, in ancient times people living in countries invaded by plague made use of convalescents for nursing plague patients and burying corpses. Postinfection and postvaccinal immunities are predominantly due to the phagocytic activity of the cells of the lymphoid-macrophage system. An important role is played by the protective capsular antigen which serves as the basis in the preparation of chemical antiplague vaccines. Laboratory diagnosis. Examination is carried out in special laboratories and in antiplague protective clothing. A strict work regimen must be observed. Depending on the clinical form of the disease and the location of the causative agent, test specimens are collected from bubo content (in bubonic plague), ulcer secretions (in cutaneous plague), mucus from the pharynx and sputum (in pneumonic plague), and blood (in septicaemic plague). Test matter is also recovered from necropsy material (organs, blood, lungs, contents of lymph nodes), rodent cadavers, fleas, foodstuff's, water, air, etc. 1. Microscopy of smears, fixed in Nikiforov's mixture and stained by the Gram method or with methylene blue by Loeffler's method. 2. Inoculation of the test material into nutrient media, isolation of a pure culture and its identification. 3. Biological tests of the isolated pure culture and of material from which isolation of the organism is difficult are conducted on guinea pigs Treatment.At present streptomycin is used for treatment of plague, the drug being very effective and curing even pneumonic plague in a high per cent of cases. Good results have been obtained from a combination of streptomycin with chloromycetin or tetracycline with antiplague serum. Antiplague gamma-globulin and a specific bacteriophage are also used for treatment of plague patients. Penicillin, chlortetracycline, and sulphonamides are recommended in cases with complications. Prophylaxis. General prophylaxis comprises the following measures: (1) early diagnosis of plague, particularly the first cases; (2) immediate isolation and hospitalization of patients and enforcement of quarantine; (3) observation (i. e. isolation of individuals or groups of people suspected of having been in contact with infected material, daily inspection from house to house, temperature measurement twice a day, and observation during the possible incubation period); (4) thorough disinfection and extermination of rats in disease foci; (5) individual protection of medical personnel and prophylactic treatment with streptomycin and vaccination; (6) prophylactic measures and systematic observation carried out by plague control laboratories, stations, and institutes in endemic areas; (7) observance of international plague control conventions; (8) security measures from plague invasion at frontiers. Specific prophylaxis is accomplished with live EV vaccine. Causative Agent of Tularaemia The tularaemia bacteria are short coccal-shaped or rod-like cocci measuring 0.2-0.7 mcm. In old cultures the organisms retain the coccal form. They are non-motile, polychromatophilic, and Gram-negative. In the animal body they are sometimes surrounded by a fine capsule. Cultivation. The tularaemia organism is an aerobe which does not grow on ordinary media, but grows well at 37° C on media rich in vitamins, e. g. yolk medium which consists of 60 per cent of yolk and 40 per cent of a 0.85 per cent sodium chloride solution with pH 6.7-7A. The organisms are cultured in a thermostat for 2-14 days. Fermentative properties. Tularaemia bacteria break down proteins with the elimination of hydrogen sulphide, and do not produce indole. They ferment glucose, levulose, mannose, and maltose, with acid formation. Dextrin, saccharose, and glycerin fermentation is not a stable property. Biochemical properties are unstable and liable to comparatively rapid changes. Toxin production. The existence of a soluble toxin in tularaemia bacteria has not been demonstrated. The organism's virulence is associated with its K-antigen. The tularaemia bacterium grows poorly in liquid media, and for this reason it is difficult to isolate any toxin. Pathogenicity for animals. The organism is pathogenic for water rats, field voles, grey rats, common field mice and house mice, hares, susliks, chipmunks, hamsters, muskrats, gerbils, moles, shrews, and other animals. Among the domestic animals camels, sheep, cats, dogs, and pigs are susceptible to the disease, and among laboratory animals, guinea pigs and white mice. Laboratory diagnosis. 1. Allergy develops on the thirdfifth day of the disease. For this reason, intracutaneous and cutaneous tests with tularine are made for early diagnosis. In tularaemia patients the test gives a positive reaction 6-12 hours after inoculation of tularine. 2. In the second week of the disease agglutinins begin to accumulate in the blood. They are detected by carrying out the agglutination reaction by the blood-drop and volume methods. In some cases this test may give a positive reaction with material containing brucella organisms, since they possess antigens common to tularaemia bacteria. 3. The tularaemia culture is isolated by the biological method as it is impossible to recover the pathogen directly from a tularaemia patient. For this purpose white mice or guinea pigs are infected by material obtained from people suffering from the disease (bubo punctate, scrapings from ulcers, conjunctiva! discharge, throat films, sputum, and blood). 4. Laboratory diagnosis of rodent tularaemia is made by microscopy of smears from organs, precipitin ring reaction (thermoprecipitation), and biological tests. Water, foodstuffs, and blood-sucking arthropods are examined by biological tests. Prophylaxis comprises the following measures: (1) systematic observation, absolute and relative registration of rodent invasion, and extermination of rats; (2) prevention of mass reproduction of the rodents; (3) protective measures in agricultural enterprises against contamination by tularaemia-infected rodents; (4) protection of foodstuffs and water from rodents; (5) control of ticks, horseflies, stable-flies, mosquitoes, and protection from these insects; (6) specific prophylaxis with a live vaccine. The vaccine is prepared in a dry form. A single application is made by rubbing it into the skin and it produces immunity for a period of 3-6 years. Brucellae Brucella abortus Brucella melitensis Brucella cuis Brucellae are small, coccal, ovoid-shaped micro-organisms 0.5-0.7 mcm in size. Elongated forms are b.6-1.5 mem in length and 0.4 mcm in breadth. Under the electron microscope Brucella organisms of cattle, sheep and goats appear as coccal and coccobacilary forms, while those of pigs are rod-shaped. They are Gram-negative, non-motile, and do not form spores or capsules (in some strains capsules are sometimes present). DNA contains 56 to 58 per cent of G+C. Cultivation. The organisms are aerobic. When cultivated from material recovered from patients, they grow slowly, over a period of 8-15 days. Brucella organisms may be cultivated on ordinary media, but they grow best on liver-extract agar and liver-extract broth. On liver-extract agar the organisms form round, smooth colonies with a white or pearly hue. In liver-extract broth they produce a turbidity, and subsequently a mucilaginous precipitate settles at the bottom of the tubes Brucella organisms grow well on unfertilized eggs and on the yolk sac of a 10-12-day-old chick embryo. The brucellae of bovine origin (Brucella abortus) only grow in an atmosphere of 10 per cent carbon dioxide, which serves as a growth factor. Colonies of Brucella Fermentative properties. Brucellae do not liquefy gelatin and do not produce indole. Some strains produce hydrogen sulphide, break down urea and asparagin, reduce nitrates to nitrites, and hydrolize proteins, peptones and amino acids, with release of ammonia and hydrogen sulphide. No carbohydrates are fermented, although a small number of strains ferment glucose and arabinose. Toxin production. Brucellae do not produce soluble toxins. An endotoxin is produced as a result of disintegration of the bacterial cells. This endotoxin possesses characteristic properties and may be used in allergic skin tests Antigenic structure. The organism contains four antigens: A, M, O, Vi, G and R. The M-antigen is predominant among brucellae of sheep and goats, and the A-antigen, in the other species. Substances of polysaccharide character, with no type specificity, have been extracted from brucellae of cattle, sheep and goats. Pathogenity for animals. Goats, sheep, cattle, pigs, horses, camels, deer, dogs, cats, and rodents (rats, mice, susliks, hamsters, rabbits, field-voles, water rats, and other animals) are all susceptible to infection by brucellae. The high concentration of brucellae in the placenta of cattle is explained by the presence in this tissue of the growth stimulator erythrol. In human beings brucellosis is characterized by undulant fever with atypical and polymorphous symptoms. The disease may assume an acute septic or a chronic metastatic course. The structural and motor systems, haemopoietic, hepatolienal, nervous and genital systems are often involved. Pregnant women may have miscarriages. Often brucellosis recurs, continuing for months and years. The death rate is 1-3 per cent. The diagnosis of mild, asymptomatic forms presents difficulties and is based on laboratory tests. Laboratory diagnosis. The patient's blood and urine (for isolation of the pathogen), serum (for detection of agglutinins), milk and dairy products (for detection of brucellae or agglutinins in milk) are examined. The microbe is isolated in special laboratories. 1. Culture isolation. Since brucellosis is often accompanied by bacteraemia, blood is examined during the first days of the disease (preferably when the patient has a high temperature). The cultures are grown for 3-4 weeks or more. Five to ten per cent of carbon dioxide is introduced into one of the flasks (for growth of the 23 bovine species of the bacteria). Inoculations on agar slants are made every 4-5 days for isolation and identification 'of the pure culture. Brucella susceptibility to stains An antiphage serum is introduced into the cultures for neutralization of the phage which inhibits the growth of brucellae. The best results are obtained when the blood is inoculated into the yolk of an unfertilized egg or the yolk sac of a chick embryo. Growth is examined every 2-3 days. If the blood culture produces a negative result bone marrow obtained by sternum puncture is inoculated onto solid and liquid media for isolation of myelocultures. Susceptibility to phages The urine is also examined. It is obtained with a catheter, centrifuged, and 0.1 ml of the precipitate is seeded onto agar plates containing 1 :200000 gentian violet. In some cases faeces, cow's and human milk, and amniotic fluid of sick humans and animals are examined for the presence of Brucella organisms. Brucella cultures may be isolated by the biological method. For this purpose healthy guinea pigs or white mice are injected with 0.5 or 3 ml of the test material. A month later the guinea pigs' blood is tested for agglutinins, the allergic test is carried out, and the pure culture is isolated. White mice are tested bacteriologically every three weeks. 2. Serological test. The Wright (in test tubes) and Huddleson (on glass) reactions are carried out. The Wright reaction is valued highly positive in a 1 800 serum dilution, positive in a 1:400-1:200 dilution, weakly positive in 1 :100 dilution, and doubtful at a titre of 1 :50. 3. Skin allergic test. To determine allergy, Burne's test is made beginning from the fifteenth-twentieth day of the disease. A 0.1 ml sample of the filtrate of a 3- or 4-weekold broth culture (brucellin) is injected intracutaneously into the forearm. The test is considered positive if a painful red swelling 4 by 6 cm in size appears within 24 hours. 4. Opsono-phagocytic test. This test detects changes in the phagocytic reaction. The index of healthy individuals averages 0-1 and occasionally 3-5. In sick persons the reaction is considered high if the index is 50-70, mild, if it is 25-49, and low, if it is 10-24. For detecting brucellae in the external environment the reaction for demonstrating a rise in bacteriophage titre is carried out. 5. In some cases the complement-fixation test, the indirect haemagglutination reaction, and the immunofluorescence reaction are used. Treatment. Patients suffering from brucellosis are treated with antibiotics (amphenicol, tetracycline, etc.). Chronic cases are best treated by vaccine therapy. X-ray therapy, blood transfusions, electropyrexia, and balneotherapy, hormonotherapy. Injection of antibrucellosis gammaglobulin is recommended for the prevention of recurrences. Prophylaxis comprises a complex of general and specific measures carried out in conjunction with veterinary services. Immunization with the live or killed vaccine is an additional measure in districts where there are cases of goat-sheep brucellosis. B. anthracis belongs to the family Bacillaceae. Anthrax bacilli are large organisms, measuring 3-5 mcm in length and 1-1.2 mcm in breadth. In the body of animals and man they occur in pairs or in short chains, while in nutrient media they form long chains. In stained preparations the ends of the bacilli appear either to be sharply cut across or slightly concave, resembling bamboo canes with elbow-shaped articulations. The G+C content in DNA is 32 to 62 per cent. B. anthracis In the bodies of man and animals the bacilli produce capsules which surround a single organism or are continuous over the whole chain. Capsules are also produced on nutrient media which contain blood, serum, egg yolk, or brain tissue. Colony of B. anthracis Colony of B. anthracis Fermentative properties. The anthrax bacilli possess great biochemical activity. They contain the enzymes — dehydrogenase, lipase, diastase, peroxidase, and catalase. In gelatin stab-cultures growth resembles an inverted fir tree, the gelatin being liquefied in layers. The organisms cause late liquefaction of coagulated serum and produce ammonia and hydrogen sulphide. They slowly reduce nitrates to nitrites and coagulate and peptonize milk. The organisms ferment glucose, levulose, saccharose, maltose, trehalose, and dextrin with acid production. Toxin production. When growing on semisynthetic medium, B. anthracis discharges an exotoxin (oedema factor) into the culture fluid. The capsular substance is very toxic, it contains Brayle's aggressins. Loss of the capsule results in loss of virulence. It has been established that some strains of B. anthracis produce in the animal's body a lethal toxin (mouse factor), which on addition of the oedema factor or the protective antigen causes death of the animal. The serum of guinea pigs who died from anthrax possesses the property of causing death of albino mice and guinea pigs on being injected intra-venously in small doses. Components of Anthrax Toxin Component EE LF PA Function Inactive adenylate cyclase activated by calmodulin Causes pulmonary edema and death in rats; cytolytic for macrophages Required for the binding of both EF and LF to host cell EF, edema factor; LF, lethal factor; PA, protective antigen Differential-Diagnostic Signs of B. anthracis, Antracoides Properties B. anthracis Anthracoides Motility Capsule formation Hemolysis Lysis with specific phage “Pearl necklace” test + + + + + - + - Pathogenicity for rabbits + - Pathogenesis and diseases in man. Anthrax is a typical zoonosis. Anthrax is primarily a disease of sheep, goats, cattle, and, to a lesser extent, other herbivorous animals. Once the disease is established in an area, bacterial endospores from infected or dead animals are able to contaminate the soil and, because of the resistant endospores, the pasture areas remain infectious for other animals for many years In most animal infections, the spores enter the body by way of abrasions in the oral or intestinal mucosa, and after entering the bloodstream, they germinate and multiply to tremendous numbers, causing death in 2 to 3 days. Humans acquire the disease from sick animals or articles and clothes manufactured from contaminated raw materials: sheepskin coats, fur mittens, collars, hats, shaving-brushes, etc. In summer the infection may be transmitted by blood-sucking insects. Anthrax occurs in three main clinical forms: cutaneous, respiratory, and intestinal. Lesion of cutaneous anthrax (eighth day of illness) on the arm of a person who had been a carder in a wool factory Laboratory diagnosis. In cases of cutaneous anthrax the malignant pustular exudate is examined; it is obtained from the deep layers of the oedematous area where it borders with the healthy tissues. Sputum is examined in cases of the respiratory form, faeces and urine, in intestinal form, and blood is examined in cases of septicaemia. 1. The specimens are examined under the microscope, the smears are Gram-stained, or stained by the RomanowskyGiemsa method. The presence of morphologically characteristic capsulated bacilli, arranged in chains, allows a preliminary diagnosis. 2. For isolation of the pure culture the specimens are inoculated into meat-peptone agar and meat-peptone broth. The isolated culture is differentiated from other morphologically similar bacteria by its morphological and biochemical properties. 3. Laboratory animals (white mice, guinea pigs and rabbits) are inoculated with the pathological material and with the pure culture derived from it. B. anthracis causes the death of white mice in 24-48 hours and of guinea pigs in 2-3 days following inoculation. Microscopic examination of smears made from blood and internal organs reveals anthrax bacilli which are surrounded by a capsule. Phagolysis of B. anthracis A rapid biological test is also employed. The culture obtained which has to be identified is introduced intraperitoneally into white mice. Several hours after inoculation smears are prepared from the peritoneal contents. Detection of typical capsulated bacilli gives a basis for con-firming the final result of the biological test. The allergic test with anthracin (a purified anthrax allergen) is employed when a retrospective diagnosis is required in cases which have yielded negative results with microscopical and bacteriological examination. Postmortem material as well as leather and fur used as raw materials are examined serologically by the thermoprecipitin reaction (Ascoli's test) since isolation of the bacilli is a matter of difficulty in such cases. As can be seen in Fig., the result in the first test tube (containing the test material) may be either positive or negative, in the second test tube (control) it must be only positive, and in the third, fourth, fifth, and sixth control test tubes the results must always be negative. When employing laboratory diagnosis of anthrax, one must bear in mind the possibility of the presence of bacteria identical with B. anthracis in their biological properties. These sporing aerobes are widely distributed in nature and are normally sporeforming saprophytes. They include B. cereus, B. subtilis, B. megaterium, etc. The anthrax bacilli may be differentiated from anthracoids (false anthrax organisms) and other similar sporing aerobes by phagodiagnosis. The specific bacteriophage only causes lysis of the B. anthracis culture. Treatment comprises timely intramuscular injection of antianthraxglobulin, and the use of antibiotics (penicillin, tetracycline, and streptomycin). Prophylaxis. General measures of anthrax control are carried out in joint action with veterinary workers. These measures are aimed at timely recognition, isolation, and treatment of sick animals. They also include thorough disinfection of premises for live-stock, territory an dall objects found on it, and ploughing over of pastures. Carcasses of animals which have died of anthrax are burnt or buried on specially assigned territory, not less than 2 meters deep, and covered with lime chloride. The veterinary authorities also enforce regulations banning the use of contaminated meat for food and introduce thorough control of manufactured articles from animal hide and fur which are to be marketed. Ever since Pasteur's celebrated field trial, in which animals were successfully immunized with a living attenuated suspension of B. anthracis, efforts have been directed toward the production of effective vaccines that possess little or no toxicity. Because killed vaccines are of little value, two different approaches for the stimulation of artificial immunity have been undertaken: (1) the isolation and use of the protective antigenic component of the anthrax toxin, and (2) the use of attenuated living bacteria to induce antitoxic immunity. At present, a vaccine, prepared from non-capsulated anthrax bacilli and consisting of a suspension of live spores of vaccine strains, is used. It is employed for immunization of man and domestic animals. The vaccine is completely harmless, producing immunity quite rapidly (in 48 hours) and for a period of over a year. It is inoculated in a single dose. Vaccination is carried out among people who work at raw-material processing factories (processing of animal hide and hair), at meatpacking factories, and at farms where anthrax is encountered. Reinoculation is performed after a period of 12 months. However, all effective living vaccines possess some toxicity, and they have not been used in the United States for humans. The vaccine licensed in the United States for use in humans is an aluminum hydroxide-adsorbed supernatant material from ferment or cultures of a toxigenic, but nonencapsulated strain of B. anthracis. Unfortunately, it induces a short-lived immunity and requires annual boosters. Individuals who have been in contact with material contaminated with anthrax organisms (when dressing infected carcasses or using such meat for food) are given intramuscular injections of 20-25 ml of antianthrax globulin together with penicillin. PA seems to be the only effective component of the vaccine because neither EF nor LF induced protection. It has been cloned in Bacillus subtilis, and guinea pigs immunized by the intramuscular injection of the B subtilis cell suspension were protected against challenge by B. anthracis. PA also has been cloned in vaccinia virus, where it induced at least partial immunity to challenge in guinea pigs and mice. It is, therefore, possible that a cloned source of PA will be used in future anthrax vaccines for humans. The vaccine used in domestic animals consists of a living spore culture, which is designated the Sterne strain. It still carries the plasmid encoding for PA, EF, and LF, but its avirulence is attributed to the loss of the plasmid encoding the antiphagocytic capsule.