Unit 4 Antidysrhythmic and Antihypertensive Agents
advertisement

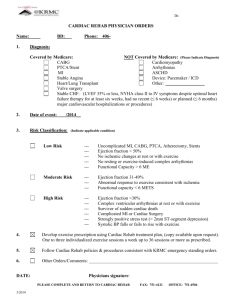
NURS 1950 Pharmacology Nancy Pares, RN, MSN Heart beat arises outside the sinoatrial (SA) node Terms: ◦ Inotropic ◦ Chromotropic ◦ Domotropic Arrhythmia or dysrhythmia Variation of normal rhythm-usually associated with cardiac ◦ An electrical activity initiated by a spontaneous discharge Decrease the automaticity of the cardiac tissues distant from the sinoatrial node. Alter the rate of conduction thru the heart Alter the refractory period between consecutive contractions. Classed according to action ◦ Class I: myocardial depressents-inhibit sodium ion movement preventing depolorization Ia: prolongs electrical stimulation (in cell) prolongs refractory time between impulses –delays repolarization Ib: shortens the duration of the e-stimulation and the time between impulses—accelerates repolerization Ic: most potent-slows conduction rate through atria and ventricles—no effect on repolorization Class II: beta-andrenergic blocking agents -block sympathetic stimulation (slows conduction and decreases HR Class III: slows the rate of electrical conduction and prolongs refractory time -potassium channel blocking Class IV:blocks calcium ion flow-prolongs elec stimulation and slows AV node conduction Misc: Adenosine and Digoxin: not related to any other agents Objective 5: List the side effects of antirrhythmics Includes: ◦ ◦ ◦ ◦ Disopramide phosphate (Norpace) Procainamide HCL (Pronestyl) Quinidine gluconate (Duraquin) Quinidine polygluconate (Cardioquin) ◦ Prototype: Procainamide (Pronestyl) -derived from the cinchona bark -cardiac depressant effects: reduces excitability of the cardiac muscle, prolongs refractory period between consecutive contractions ◦ Allows the sinoatrial node to take over Used for atrial tachycardia, flutter and fibrillation. Side effects severe: 1/3 of clients must d/c use S/E: ◦ GI distress ◦ CV disorders ◦ Rashes, respiratory arrest, hemolytic anemia, agranulocytosis ◦ Hypersensitivity Cinchonism: tinnitus, nausea, HA, dizziness impaired vision, vertigo Nursing Implications: ◦ Can reduce problems if nurse: Avoid use in CHF patients Monitor digitalis levels (if on digitalis) Monitor potossium (K+) levels Monitor sodium (Na+) levels Routes: ◦ Oral with meals ◦ Parenteral: give slowly Uses:ventricular arrhythmias (best), atrial fibrillation(helpful), paroxysmal atrial tachycardia (PAT) S/E: GI distress, ventricular tachy, hypotension and hypersensitivity ◦ Allergy most likely if allergic to ‘caine’ drugs (related to local anesthetics) ◦ Can cause agranulocytosis: lupus like syndrome S/E: hypotension, tachyarrythmias, anticholinergic effects Has lower incidence of adverse effects than quinidine or procainamide Oral dosing Lidocaine (Xylocaine) Mexiletine (Mexitil) Phenytoin (Dilantin) Tocainide (Tonocard) Use:Preventricular contractions (PVC), cardiac glycoside-induced tachyarrhythmias, cardioversion Action: very rapid onset (IV), short acting ◦ Shortens the duration of elec stim ◦ Gives precise control of cardiac status S/E/Route: ◦ ◦ ◦ ◦ Excessive decrease in cardiac electrical conductivity Hypotension, bradycardia, dizziness; CNS effects Hypermetabolism (malignant hyperthermia ineffective if given orally (metabolized in liver) Nursing Interventions: ◦ Continuous EKG ◦ Look at bottle before giving-should not contain preservatives or epinephrine -standard classification is neuroleptic, but used for arrythmias caused by cardiac glycoside intoxication Action: decreases automaticity of cardiac muscle, increases rate of conduction of the cardiac electrical impulses S/E/ Route: ◦ Neurological disturbances: peripheral neuropathy, diplopia, ataxia, vertigo, drowsiness, confusion ◦ GI disturbances ◦ Skin rash Similar to lidocaine Nursing Interventions: ◦ Given orally only ◦ Monitor EKG ◦ Client teaching: s/e and when to call MD S/E: ◦ Dizziness, nausea, parethesia, numbness, restlessness, tremor, GI distress, blood dyscrasias ◦ Should not be used in 2nd or 3rd degree AV block without a pacemaker Action: similar to lidocaine Use: ventricular arrhythmias S/E/route: ◦ N/V, heartburn, dizziness, tremor, impaired coordination ◦ Given orally Flecainide (Tambocor) Encainide (Enkaid) Rythmol Action: local anesthetic Use: ventricular arrhythmias S/E/route: ◦ Can cause new or worsen arrhythmias ◦ High degree of negative inotropy ◦ Dizziness, visual disturbances, HA, nausea, fatigue, chest pain Local anesthetic, membrane stabalizing, some beta blocking effect Use: life threatening ventricular arrhythmias S/E: may cause new or worsen existing arrhythmias, dizziness, GI disturbances, may see 1st degree AV block Nursing Interventions: monitor with EKG Contraindications: uncontrolled CHF, brady, bronchospasm, severe hypotension Acebutolol (Sectral) Esmolol (Brevibloc) Propranolol (Inderal) Action: ◦ Inhibits cardiac response to sympathetic nerve stimulation by blocking the beta receptors; reduces heart rate, systolic BP and cardiac output. Use: ◦ ◦ ◦ ◦ ◦ Ventricular arrhythmias Sinus tachycardia Paroxysmal atrial tachycardia (PAT) Premature ventricular contractions (PVC) Tachycardia associated with atrial flutter,or fibrillation S/E: ◦ What would we expect to see? Slow HR, orthostatic hypotension, SOB, painful urination, wt gain > 2 lbs/day, insomnia, drowsiness, confusion Mask the signs of hypoglycemia Nursing Interventions: Take pulse and report below 50, rise slowly, report symptoms, diabetics monitor BS closely Amiodarone (Cordarone) Dofetilidide (Tikosyn) Sotalol (Betaspace) Action: ◦ Prolongs the action potential of the atrial and ventricular tissues ◦ Antagonizes (non competitive) the alpha and beta receptors causing vasodilation Use: ◦ Life threatening arrythmias non responsive to other agents S/E/Route: ◦ Fatigue, tremors, sleep disturbances, numbness, ataxia, confusion, exertional dyspnea, nonproductive cough, pleuritic chest pain, photosensitivity ◦ s/e often cause clients to d/c use ◦ > 400mg/day cause problems ◦ Given oral or IV Nursing interventions: ◦ ◦ ◦ ◦ ◦ Loading dose is needed Watch monitor for new arrhythmias Dose adjustment is difficult Monitor/teach about post treatment arrhythmias Wear sunscreen Action/Use: ◦ slows conduction through the AV node causing relaxation of the coronary and peripheral vessels ◦ Dysrhythmias S/E: ◦ HA, dizziness, lower extremity edema, increases digoxin and quinidine levels Nursing interventions: ◦ Do not crush or chew extended release tablets ◦ Use with caution with other CV agents: digoxin, beta adrenergic blockers ◦ Monitor for partial or complete heart block, heart failure Adenosine (Adenocard) Digoxin (Lanoxin) Ibutilide ( Corvert) Action/Use: ◦ Strong depressant effect on SA and AV nodesslowing conduction ◦ Treatment of paroxysmal supraventricular tachycardia (PST) ◦ Physiologic roles: energy transfer, prostoglandin release, inhibits platelet aggregation, coronary vasodilation, suppresses heart rate S/E ◦ Flushing, SOB, chest pressure, nausea, HA, dizziness, peripheral edema, anxiety ◦ Half life is 10 seconds—s/e are not lasting Give meds on scheduled time Assess 6 cardinal signs of CV disease ◦ Chest pain, dyspnea, edema, fatigue, syncope, palpitations (C-D-E-F-S-P) Lab tests: CV markers (enzymes) Physical assessment of client: include EKG readings Be prepared for emergency care O2 as needed Assist with ADLs Client education ◦ Lifestyle ◦ Medications ◦ Report s/e and adverse effects Also called ‘idiopathic’ ‘essentially’ no known cause Cardiac output ◦ Increase cardiac output=increased BP Peripheral vascular resistance (PVR) ◦ Lumen inside vessels will constrict and dilate which determines PVR Total Blood volume (see diagram in Adams) Carbonic anhydrase inhibitors ◦ Rarely used for hypertension Thiazides Loop diuretics Potassium sparing ◦ Used in combination therapy with thiazide or loop diuretic Deplete blood volume Help excrete sodium Dilate peripheral aterioles ◦ Specific action unknown Often used in combination ◦ Potentiates activity of other antihypertensives Cheap and effective Thiazides: ◦ Most effective if creatinine clearance >30 ◦ Most commonly used: Hydrochlorothiazide Loop diuretics ◦ Used when creatinine clearance <30 ◦ Most commonly used Furosemide (Lasix) Potassium sparing ◦ Contraindicated with renal disease, pregnancy, gout or kidney stones ◦ Nursing interventions: Monitor labs (WBC decrease, liver and kidney) Client education ◦ Most commonly used: Spirolactone (aldactone) S/E: gynecomastia, testicular atrophy, hirsutism Beta-adrenergic blockers Angiotensin converting enzyme (ACE) inhibitors Calcium channel blockers Action/use: Propranolol (Inderol) ◦ Inhibit cardiac response to sympathetic nerve stimulation (block the beta receptors) Decreases BP by decreasing cardiac output and heart rate Drugs of choice for Stage 1 & 2 hypertension ◦ Clinical advantages: Minimal postural or exercise hypotension No effect on sexual function Minimal slowing of CNS S/E/contraindications: ◦ Bradycardia, peripheral vascular resistance, bronchospasm, wheezing, heart failure, hypoglycemia Dose related ◦ Avoid use in clients w asthma, type 1 diabetes, heart failure, peripheral vascular resistance disease Nursing implications: ◦ Give lowest dose giving desired effect ◦ Needs days-weeks to get optimal effect ◦ Do not d/c suddenly Action/use ◦ Prevent angiotensin I converting to angiotensin II =no vasoconstriction, no aldosterone secretion, no sodium retention ◦ Preserve cardiac output, increase renal blood flow; use with diuretic ◦ Does not aggrevate asthma, COPD, diabetes, gout, or cholesterol levels S/E: ◦ Nausea, fatigue, HA, diarrhea, orthostatic hypotention: REPORT: swelling of face, eyes, lips, tongue and SOB Action: ◦ Binds to angiotensin II receptor sites=no vasoconstriction ◦ Does not affect bradykinin=no chronic cough ◦ As effective as ACE inhibitors ◦ Need to add diuretic with African-American population Action/uses: ◦ Inhibits calcium movement across cell membrane: reduces arrhythmias, slows rate of contraction of heart, relaxes smooth muscle of vessels. ◦ Antihypertensive, antianginal, alternative to beta blockers ◦ Effective in African Americans S/E: ◦ Hypotension and syncope ◦ Edema Diltiazem (Cardizem) Nifedipine (Procardia) Action/Use: ◦ Aterial and venous vasodilation=reduced PVR ◦ Does not reduce cardiac output, does not cause produce reflex tachycardia, reduces HDL, increases HDL ◦ Additive effect with beta blockers and diuretics to decrease BP ◦ Stage 1-3 hypertensions ◦ Helpful in BPH S/E: ◦ Drowsiness, HA, dizziness, weakness, lethargy (these are self limiting) ◦ Dizziness, tachycardia, fainting Take with food, lie down if s/s Action: ◦ Stimulates adrenergic receptors in brain stem; reduces sympathetic outflow from CNS===decreases HR and PVR Uses/routes: ◦ Combination with other antihypertensive agents; when other antihypertensive agents do not work. ◦ Patch: action=one wk duration; causes more S/E:sedation, dry mouth, fatigue, sexual dysfunction Nursing interventions: ◦ Monitor vitals ◦ I&O ◦ Do not d/c suddenly: causes rebound effect with rapid rise in BP Agitation, restlessness, tremors, HA, nausea, increased salivation. Nursing diagnoses: ◦ ◦ ◦ ◦ Excess fluid volume Risk for fluid volume deficit Altered urinary elimination Ineffective health maintenance Monitor lab values Observe for changes in LOC Monitor for hydration I/O; daily wt, diet monitor Monitor caffeine and alcohol intake photosensitivity