Medicare Australia Annual Report 2009
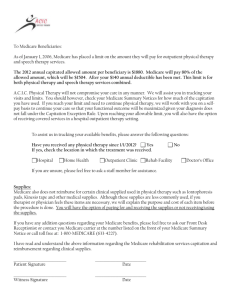
advertisement

Medicare Australia Annual Report 2009-10 If you have comments and questions about this report, contact: The Annual Report Project Manager Human Services Portfolio Corporate Communication Branch PO Box 7788 Canberra Business Centre ACT Australia 2610 Email: annualreport.medicare@centrelink.gov.au You can speak to Medicare Australia in languages other than English: Phone: 13 2011 You can contact Medicare Australia if you are deaf or have a hearing or speech impairment: Phone: Freecall™ 1800 552 152 (a TTY phone is required to use this service) If you are an Aboriginal or Torres Strait Islander person, you can contact Medicare Australia on: Phone: Freecall™ 1800 556 955 You can order a paper copy of this report: Email: annualreport.medicare@centrelink.gov.au You can access an online version of this report: Full PDF and HTML versions are available at www.medicareaustralia.gov.au. ISSN: 0313-1041 © Commonwealth of Australia 2010 This work is copyright. Apart from any use as permitted under the Copyright Act 1968, no part may be reproduced by any process without prior written permission from the Commonwealth. Requests and enquiries concerning reproduction and rights should be addressed to the Commonwealth Copyright Administration, Attorney-General’s Department, National Circuit, Barton ACT 2600 or posted at http://www.ag.gov.au/cca. Medicare Australia PO Box 1001 Tuggeranong DC ACT 2901 ABN 75 174 030 967 About this report This year the annual reports for the Department of Human Services, Centrelink and Medicare Australia reflect the move to integration within the Human Services portfolio. Although three separate reports are required under relevant legislation, the aim was to achieve some common content and design elements to signify the increasingly close working relationships between the three organisations. Given the implementation of service delivery reforms during the year across the Human Services portfolio, this report can be read as a companion with those of the Department of Human Services and Centrelink. This annual report was prepared according to the Requirements for Annual Reports, issued by the Department of the Prime Minister and Cabinet on 23 June 2010. The report focuses on Medicare Australia’s accountability and performance during 2009-10. The requirements have changed for annual reporting so that government agencies and departments now report against the programs they have in place, rather than report against their outputs. Therefore, this report is structured according to its four programs, with separate chapters on customer service and partnerships, and management and accountability. Chapter 1: Overview—This contains the review of the Chief Executive Officer, Lynelle Briggs, as well as an overview of the whole portfolio and how service delivery reform is being implemented. It also explains the structure of Medicare Australia, its new reporting framework and governance arrangements. Chapter 2: Delivery of medical benefits and services—sets out how Medicare Australia delivers its services, including on behalf of the Department of Veterans’ Affairs, and the results it achieved. Some of these services include the Immunisation Register, the Organ Donor Register, programs for GPs in rural areas and medical indemnity. Chapter 3: Delivery of pharmaceutical benefits and services—covers how the scheme works, including eligibility and the safety net, and how many benefits were paid and services processed. Chapter 4: Delivery of other benefits and services—highlights the many other services that Medicare Australia delivers—such as aged care initiatives, the Healthcare Identifiers Service, the Home Insulation Program and the new Small Business Superannuation Clearing House. Chapter 5: Medicare rebates—electronic claiming—highlights the three major ways in which Medicare Australia is encouraging customers to go online: Medicare Online, Medicare Easyclaim and the ECLIPSE program. It analyses the rapid take-up of its electronic business. Chapter 6: Customer service and partnerships—sets out Medicare Australia’s relationships across government, and with other stakeholders, including its customer service charter. It also explains how Medicare Australia is developing a ‘co-design’ practice as part of service delivery reform within the Human Services portfolio—this will involve the community, staff and stakeholders in shaping the reform activities. Chapter 7: Management and accountability—explains Medicare Australia’s measures to remain transparent and accountable in its expenditure and operating results. It also covers its compliance and communication activities, its ICT performance and how it manages staff. Chapter 8: Financial statements—Audited by the Australian National Audit Office, Medicare Australia’s financial statements are prepared according to the Financial Management and Accountability Act 1997. Fifteen appendices respond to a number of mandatory reporting requirements, including the compliance index. The back of the report contains a glossary, shortened forms, general index and contact details for Medicare Australia. Chapter 1 Overview CHIEF EXECUTIVE OFFICER’S REVIEW Medicare Australia has a long and proud history of delivering services to Australians—and it is certainly a great honour for me to be leading this organisation, especially at a time of major change. When I was appointed Chief Executive Officer (CEO) of Medicare Australia in August 2009, I was struck by the enormous goodwill shown by Medicare Australia staff and by the esteem in which Australians hold Medicare. That level of trust is reflected in this year’s Eye on Australia report by Sweeney Research, which ranks Medicare Australia as Australia’s fourth most trusted brand, after the Salvation Army, Google and Australia Post. In December 2009 the Minister for Human Services, the Hon. Chris Bowen, MP, announced major reforms to the way the Australian Government delivers services to the Australian people. The service delivery reform changes we are planning to make are some of the most exciting initiatives I have been involved in during my 30-year career. Six streams of service delivery reform were identified: greater convenience of access, through locational, phone and online improvements real improvements for people in remote areas or who are socially isolated greater coordination with a real case management approach across government services for people most in need of intensive support efficiencies in the back office functions through integration of information technologies, finances, human resources, property management and procurement a progressive implementation of a ‘tell us once’ experience for citizens and business when dealing with government agencies linked services with business and community sector organisations to deliver services more effectively to those who need and want them. Creating a single department comprising the current Department of Human Services, Medicare Australia and Centrelink is an enormous undertaking and something we should all be excited about. To put this in perspective—the organisations within the Human Services portfolio employ around 40 000 people. There are considerable expertise and resources invested in physical networks (offices and outreach services), virtual networks (telephony services) and online servicing (internet-based applications). With its objective of helping improve health outcomes through the provision of payments and information to customers and health service providers, Medicare Australia operates on a large scale—every year providing around 500 million services and $40 billion in payments. We are well positioned to move into the future. This year we have already started to make changes by bringing together the ‘enabling services’ from across the portfolio. These included areas such as information and communication technology (ICT), ministerial and parliamentary, legal services, corporate support, communication, audit and assurance, and people services. By integrating these functions we are building a solid foundation across the portfolio that will enable the rest of the organisation to follow seamlessly with more joined-up services. Achieving real reform in service delivery means thinking about issues and solutions in new ways. We are also very conscious of the need to maintain our ongoing business partnerships. During the year, we ensured our professional dealings with health sector providers continued to improve, and we have been working on a number of initiatives in this regard. We have been able to implement the first stage of the electronic record system—the Healthcare Identifiers Service. We are hoping to build on this in the future. This year a number of new and improved services were delivered through both major enhancements and the effective delivery of new and complex IT systems. We have responded to government policy initiatives, and we have delivered on time. The take-up of electronic Medicare patient claiming continues to grow, with general practitioners claiming at 47.5 per cent and specialists claiming at 15.1 per cent, giving an overall rate of 27.8 per cent at end June 2010. Over 91 per cent of bulk bill claims are submitted electronically. Ours is not a static business—nor is this a static organisation. While continuing to improve our Medicare Australia services we have also leveraged off our capability by picking up new responsibilities including a number of environmental programs and the Superannuation Clearing House for small business employers. This year we have built a stronger relationship with our key policy department, the Department of Health and Ageing, and I want to thank the Departmental Secretary, Jane Halton, and her staff for their generous and supportive engagement with us on service delivery reform. When I joined Medicare Australia, we restructured the organisation to better reflect our priorities. We now have two new deputy chief executive officers, Malisa Golightly and Gary Dunn. I know their talent and wealth of experience will stand us in good stead during this time of change. I want to thank Philippa Godwin as Acting CEO, and Rona Mellor, as Deputy CEO, who took Medicare Australia through a challenging transition that delivered significant savings, putting our budget back on track. I especially want to pay tribute to the staff of Medicare Australia who work hard and apply themselves conscientiously to provide service to all Australians. It is clear that we have a very solid foundation on which to build. We also have a strong direction from government, the unequivocal and vocal expectations of the Australian community, and the will and capability of our staff to move ahead on service delivery reform. Service delivery reform is about simplifying people’s dealings with government by giving them more control, and better support and assistance when they need it. Simply, we are working to give all Australians service delivery they deserve—easy, high-quality and that ‘works for you’. Lynelle Briggs Chief Executive Officer HUMAN SERVICES PORTFOLIO OVERVIEW The Human Services portfolio was established in October 2004 to improve the development and delivery of social and health-related services, including financial assistance, to the Australian people. The portfolio brings together the service delivery agencies Australian Hearing, Centrelink, Medicare Australia, and the Department of Human Services. The Department of Human Services includes the Child Support Program and CRS Australia. Minister On 9 June 2009 the Hon. Chris Bowen, MP, was appointed as the Minister for Human Services. The Minister for Human Services is responsible for administering the following legislation: Australian Hearing Services Act 1991, except to the extent it is administered by the Minister for Health and Ageing Child Support (Assessment) Act 1989, insofar as it relates to the exercise of the powers and functions conferred on the Registrar under the Act Child Support Legislation Amendment (Reform of the Child Support Scheme—Initial Measures) Act 2006, insofar as it relates to the exercise of the powers and functions conferred on the Registrar under the Act Child Support Legislation Amendment (Reform of the Child Support Scheme—New Formula and Other Measures) Act 2006, insofar as it relates to the exercise of the powers and functions conferred on the Registrar under the Act Child Support (Registration and Collection) Act 1988, insofar as it relates to the appointment of the Registrar and the exercise of the powers and functions conferred on the Registrar under the Act Commonwealth Services Delivery Agency Act 1997 Medicare Australia Act 1973. Portfolio structure At 30 June 2010 the Human Services portfolio consisted of the Department of Human Services, Centrelink, Medicare Australia and Australian Hearing. The Department of Human Services consists of the central department, the Child Support Program and CRS Australia. The central department directs, coordinates and brokers improvements to service delivery, provides policy advice on service delivery matters to government, and ensures efficient implementation of government service delivery. The Child Support Program provides support to separated parents to provide the financial and emotional support necessary for their children’s wellbeing. CRS Australia helps people with a disability, injury or health condition to get and keep a job, by providing individualised vocational rehabilitation, and helping employers to keep their workplaces safe. Centrelink delivers a range of government payments and services to Australians—including retirees, families, carers, parents, people with disability, Indigenous people, and people from diverse cultural and linguistic backgrounds—and provides services at times of major change. Medicare Australia looks after the health of Australians through efficient services and payments, such as Medicare, the Pharmaceutical Benefits Scheme, the Australian Childhood Immunisation Register and the Australian Organ Donor Register. Australian Hearing is a statutory authority that provides a full range of hearing services for children and young people up to the age of 21, eligible adults and age pensioners, and most war veterans. Across the Human Services portfolio there are more than 39 000 employees. Of these, approximately three-quarters work in front- line services. Front-line service staff deal with customers either in offices, or through phone and processing centres. Figure 1—Human Services portfolio structure at 30 June 2010 SERVICE DELIVERY REFORM On 16 December 2009 the Minister for Human Services announced the start of the reform to government service delivery to develop a modern, flexible, whole-of- government service delivery system. This will enable the Australian Government to better meet the needs and expectations of the Australian people, and to better achieve policy outcomes, while delivering services more efficiently. Service delivery reform represents a fundamental transformation of government services delivered through the Human Services portfolio. The portfolio has a combined customer base almost equal to the entire Australian population and a workforce which comprises nearly a quarter of the Australian Public Service. Service delivery reform is focused on several areas of service delivery improvement that will: provide more convenient services through the co-location of offices and the integration of portfolio websites and phone numbers to bring services together deliver more coordinated services through improved assistance and intensive case coordination support for those who suffer from multiple disadvantages use technological advances to provide modern services such as online forms and letters, single online accounts and the automation of customer transactions to reduce the time people have to interact with government provide tailored services that are targeted to the needs of people and their particular circumstances improve mobile and visiting services for those people living in remote areas or who are socially isolated build on providing improved and tailored services targeted to the needs of doctors and pharmacists, including those in rural areas. Service delivery reform aims to deliver government social and health-related services that are ‘Easy, High Quality and Works for You’: Easy—meaning it is easier for people to do business with government at a time and manner that suits their circumstances. High Quality—meaning people get better quality services and more intensive help and support at times in their lives when they need it. Works for You—meaning people get service from government that ensures they receive the benefits and support they are entitled to in ways that work for them. Services will be transitioned from fragmented and separated program and process-based approaches to service offers that are coordinated, tailored and put people first. Services will be simplified and automated, giving people the option to manage their own interactions with government. Moving away from this fragmented approach will progressively enable front-line staff to provide more managed services and improved case coordination for those in need of more intensive support. This will help to prevent people falling through the cracks and provide better policy outcomes for government. For the 2010 calendar year the government gave specific commitments to: co-locate 21 Centrelink and Medicare Australia offices by the end of 2010, and around 40 by 2012 implement a single phone number and a single website for the portfolio by the end of 2010 integrate enabling support services, including information and communication technology (ICT), ministerial and parliamentary, legal services, people services, communications, corporate support, audit and assurance functions, finance, property management, procurement and human resources. As part of the reform, the Department of Human Services, Centrelink and Medicare Australia are planning to reconstitute as a single department in 2011, subject to the views of government on the proposal. During 2009-10 work began on implementing service delivery reform. Progress on this work is detailed throughout this report and the Department of Human Services and Centrelink annual reports. MEDICARE AUSTRALIA OVERVIEW The organisation Medicare Australia delivers a broad range of payments and information for health-related and other programs, on behalf of the Australian Government. It plays an integral role in the Australian health sector, especially in developing eHealth initiatives. Medicare Australia’s objective is to improve the health and wellbeing of Australians through the delivery of information and payment services. Medicare Australia provides the best possible service delivery to increase access and convenience for the public and providers. It does this mainly through electronic channels but also through its national office network. Medicare Australia has a connection with almost all Australian residents, doctors, pharmacists, aged care providers and members of the health sector. The key programs that Medicare Australia delivers include: the Medicare program veterans’ treatment accounts processing the Pharmaceutical Benefits Scheme (PBS) and Repatriation PBS, including payments under the Community Pharmacy Agreement residential aged care subsidies the Australian Childhood Immunisation Register. Table 1—Medicare Australia at a glance Medicare Offices 242 Medicare Australia access points 886 Medicare Australia public satisfaction 96% Medicare Australia provider satisfaction 89% Total benefits paid In excess of $40 billion Medicare services claimed electronically 79% Website visits 7.8 million Calls received 15.3 million Employees 5705 Employee job satisfaction 65% Medicare Australia also administers programs for general practitioners including the General Practice Immunisation Incentives Scheme, the Practice Incentive Program, the Rural Retention Program, the General Practice Registrars’ Rural Incentive Payment Scheme and the Mental Health Nurse Incentive Program. Medicare Australia works hard to protect the integrity of the programs that it administers. This includes providing information, counselling and education on the appropriate use of the Medicare Benefits Schedule, the Schedule of Pharmaceutical Benefits and other programs it administers. Legislation Medicare Australia was established under the Medicare Australia Act 1973 (see Appendix A: Commonwealth legislation relevant to Medicare Australia on page 188) and is an Australian Government agency, delivering a range of payments and services to the Australian community. Medicare Australia is a prescribed agency under the Financial Management and Accountability Act 1997 and is a statutory agency under the Public Service Act 1999 The Financial Management and Accountability Act 1997 sets out the Chief Executive Officer’s functions and responsibilities relating to Medicare Australia’s financial management. Medicare Australia has issued Chief Executive Instructions supported by detailed practice statements, procedures and delegations to help staff comply with legislative obligations. This annual report includes appendices on reports required by the following legislation: section 74 of the Occupational Health and Safety Act 1991—see Appendix B: Occupational Health and Safety on page 189 section 8 of the Freedom of Information Act 1982—see Appendix C: Freedom of information on page 190 section 311A of the Commonwealth Electoral Act 1918—see Appendix D: Advertising and market research on page 192 section 516A of the Environment Protection and Biodiversity Conservation Act 1999— see Appendix E: Ecologically sustainable development and environmental performance on page 193 the Disability Discrimination Act 1992— see Appendix F: Commonwealth Disability Strategy on page 199. Delegations Delegations are also made under the Medicare Australia Act 1973 and other relevant legislation, including the: Health Insurance Act 1973 National Health Act 1953 Health and Other Services (Compensation) Act 1995 Private Health Insurance Act 2007 Medical Indemnity Act 2002 Aged Care Act 1997 Dental Benefits Act 2008 Midwife Professional Indemnity (Commonwealth Contribution) Scheme Act 2010 Income Tax Assessment Act 1936. Authorisations Authorisations are made under the: Freedom of Information Act 1982 Judiciary Act 1903 Public Order (Protection of Persons and Property) Act 1971. OUR PARTNERSHIPS Medicare Australia’s strong partnership with government departments and agencies helps ensure the delivery of efficient and convenient services to all Australians on behalf of the Australian Government (see Appendix G: Services delivered on behalf of our partners—2009-10 year in summary on page 201). Medicare Australia delivers services on behalf of the Department of Health and Ageing (DoHA) the Department of Veterans’ Affairs (DVA) the Department of Families, Housing, Community Services and Indigenous Affairs (FaHCSIA) the Department of Innovation, Industry, Science and Research (DIISR) the Department of Environment, Water, Heritage and the Arts (DEWHA) the Department of Climate Change and Energy Efficiency the Treasury. FUNDING ARRANGEMENTS Medicare Australia is part of the Human Services portfolio and reports to the Minister for Human Services. Medicare Australia is primarily funded through direct appropriation in the annual Budget cycle. In addition, Medicare Australia receives service- related revenue under service arrangements from other Australian Government agencies and non-government entities. Direct appropriation Direct appropriation comprises 85 per cent of Medicare Australia’s revenue. Medicare Australia’s funding agreement with the Australian Government includes both fixed and variable components. The number of health and payment services processed within any financial year determines the variable component. The revenue for Medicare Australia under this arrangement was $652 million in 2009-10 and is estimated to decrease to $619.1 million in 2010-11. The reduction is mainly due to net cash funding arrangements introduced by the government from 2010-11 under Operation Sunlight. Revenue estimates may also vary depending on how underlying demand for health services impacts on Medicare Australia’s processing activities, and as a result of new policy proposals approved in the Budget context. The direct appropriation funding also includes revenue of $1.5 million in 2009-10 and $5.3 million in 2010-11 for the Superannuation Clearing House. The total appropriation of $16.1 million over three years was transferred from the Australian Taxation Office to Medicare Australia in February 2010. Department of Health and Ageing Medicare Australia provides additional services to the Department of Health and Ageing under business partnership agreements. These include the administration of the Aged Care payments function and the National Bowel Cancer Screening Register. Under these arrangements Medicare Australia received revenue of $26.6 million in 2009-10. Department of Veterans’ Affairs Medicare Australia provides services to the Department of Veterans’ Affairs through a service agreement. Medicare Australia processes claims for veterans’ treatments, including medical, hospital and allied health services, and administers the Repatriation Pharmaceutical Benefits Scheme. As with health outputs, the pricing structure for Department of Veterans’ Affairs services is based on a variable price per processed service, with fixed revenue covering related infrastructure costs. Revenue received under the service level agreement in 2009-10 was $15.3 million. Department of Families, Housing, Community Services and Indigenous Affairs/Centrelink Medicare Australia provides Family Assistance services through the Medicare branch office network on behalf of the Department of Families, Housing, Community Services and Indigenous Affairs. Revenue from this program includes a fixed amount from the department and a variable amount from Centrelink. In 2009-10 Medicare Australia received $9.2 million from the department (fixed) under this arrangement. Variable revenues of $7.8 million were also received from Centrelink under this agreement. Other sources of funding Medicare Australia is developing the Healthcare Identifiers Service under contract to the National eHealth Transition Authority. Funding under this contract was $31.8 million in 2009-10. Funding of $11.7 million was provided in 2009-10 to administer components of the Home Insulation Program on behalf of the Department of the Environment, Water, Heritage and the Arts. Revenue from other sources in 2009-10 was $7.8 million. Medicare Australia also recovers costs for the provision of statistical information and accommodation space in sub-lease arrangements. PLANNING AND REPORTING Outcome and programs In 2009-10 Medicare Australia had one outcome and four programs—see Figure 2. This is based on the outcome and program structure set out in the Department of Human Services Portfolio Budget Statements and Portfolio Additional Estimates Statements for 2009-10. Figure 2—Outcome and program structure—2009-10 STRATEGIC STATEMENT Medicare Australia’s Strategic Statement 2009-12 forms the foundation of the vision to ‘build 21st century service delivery’ through strategic themes, goals and priorities. The strategic statement has a three-year focus on aligning the organisation to: optimise the use of electronic channels to increase convenience and streamline delivery of payments and information services for the Australian community and providers partner across government to reform the way we deliver services continue to meet Australian Government and community expectations by improving cost effectiveness enhance efforts to improve the integrity of the programs delivered. Strategic themes Medicare Australia’s strategic themes focus on relationships with the Australian Government, the Department of Human Services and its agencies, including policy partners, providers, the public and an internal focus on the organisation—people, systems and values. Strategic goals Medicare Australia’s strategic goals provide direction to expand capabilities ensuring we can deliver on the government’s current and future expectations. Medicare Australia’s goals are to: partner effectively across the Australian Public Service to deliver the mandate build and strengthen partnerships with providers to deliver timely and accurate services effectively support providers to enable the public to receive more convenient services provide Australians with timely and accurate payments and information in the most convenient way deliver a new way of business through our people, systems and values. Strategic Directions 2010-11 The Human Services portfolio is integrating many of its processes and systems to be more flexible and effective in delivering easy, high quality services that work for all Australians. Medicare Australia works collaboratively across the portfolio to ensure the best outcomes for government and the Australian community. The Strategic Directions 2010-11 has been developed in collaboration with the Department of Human Services and Centrelink, as the portfolio begins to align its service delivery reform and integration. The Medicare Australia Strategic Directions 2010-11 can be viewed on the Medicare Australia website: www.medicareaustralia.gov.au. MEASURING OUR PERFORMANCE During 2009-10 Medicare Australia measured its performance using the balanced scorecard. Key performance indicators in the scorecard measure a range of financial and non-financial functions against targets and benchmarks and are refined to improve alignment with corporate and management reporting. The indicators are categorised under the seven perspectives of: business performance business integrity electronic business financial performance enabling services people compliance. Table 2—Balanced scorecard Actual 2007-08 Actual 2008-09 Target 2009-10 Actual 2009-10 Revenue $691.0m $713.9m N/A $762.3m Operating expense $697.3m $722.3m N/A $724.2m Net result ($6.3m) ($8.4m) N/A $38.1m 89% 93% ≥90% 96% Finance Service (public and government) Community satisfaction Actual 2007-08 Actual 2008-09 Target 2009-10 Actual 2009-10 Medical practitioner satisfaction 86% 74% ≥70% 85% Practice manager satisfaction 89% 87% ≥85% 91% Pharmacist satisfaction 91% 86% ≥90% 92% 93% 85.8% ≥90% in 30 seconds 87.6% 97.9% Telephone response time Medicare claim processing accuracy 97.8% 98.1% ≥98.0% Medicare average appropriated expense per billable service - - $1.32 PBS claim processing accuracy 98.3% 98.3% ≥98% PBS average appropriated expense per billable service - - $0.74 Briefs meet satisfactory standard of above N/A 98% 95% Ministerial replies to correspondence are submitted within agreed timeframes N/A N/A 95% Prompt payment of software vendor incentive N/A N/A ≥90% 90% ICT service availability 99.9% 99.81% ≥99.90% 99.98% ICT service performance 99.7% 99.46% ≥99.90% 99.89% Online claiming take-up-Medicare bulk bill 67.4% 83.6% ≥90% 91.25% Online claiming take-up - Medicare patient claim 12.6% 14% 25% 25.39% Online claiming for PBS take-up – number and percentage of participating pharmacies 4962 5099 98% 5198 95%1 97.03% Residential Entry Record (RER) Admission Form online N/A N/A $1.26 98.4% $0.73 100% 96% Internal business processes Growth and development 96.22% ≥49% 44.4% Actual 2007-08 Actual 2008-09 Target 2009-10 Actual 2009-10 Residential Classification (ACFI) online N/A N/A ≥80% 80.6% Residential Care Claim online N/A N/A ≥49% 30.5% Community Care Claim online N/A N/A ≥8% 7.4% Aged Care Client Record (ACCR) ACAT’s online N/A N/A ≥70% 37.6% Overall staff satisfaction 70% 56%2 N/A 65%^ Unscheduled absenteeism rate 13.2% 13.55% 13.4% 14.36% 6467MJ ≤10 000MJ People Social and environmental Energy usage – office – tenant light and power per 6944MJ person 6596MJ^^ 1 It was incorrectly reported in the balanced scorecard section of the 2007-08 Annual Report that the percentage of participating pharmacies was 99%. The correct figure was 95% 2 For the 2009 Staff Survey a different engagement methodology calculation was used. The reported result was 11% higher than the Australian Public Sector average. ^This figure should not be compared to previous years’ figures, as the survey methodology differed again this year. Different questions were asked and different calculations were used to produce the engagement measures. ^^To be independently verified in October 2010. GOVERNANCE Organisational structure Medicare Australia’s structure supports its strategic direction and the achievement of its outcome of improving Australia’s health through payments and information. During 2009-10 Medicare Australia’s executive management team consisted of the Chief Executive Officer and two Deputy Chief Executive Officers. Nine general managers support the Chief Executive Officer, including two working across the portfolio on the integration of staff and the development of the portfolio’s staff capability and services. Medicare Australia’s National Office is located in Canberra. There are six capital city offices that serve the public and service providers. In addition, there is a network of 242 branch offices strategically located around the country and six contact and payment processing centres Executive The Chief Executive Officer of Medicare Australia, through the Secretary of the Department of Human Services, reports to the Minister for Human Services. Section 8AB of the Medicare Australia Act 1973 sets out the responsibilities of the Chief Executive Officer under the direction of the Minister, for: deciding the objectives, strategies, policies and priorities of Medicare Australia managing Medicare Australia ensuring that Medicare Australia performs its functions in a proper, efficient and effective manner. Figure 3—Medicare Australia organisational structure at 30 June 2010 Notes This organisational chart reflects changes to organisational structures within the Human Services portfolio as part of the government’s service delivery reform agenda. From 1 March 2010 enabling services across the portfolio were integrated to provide services for the whole of the portfolio. The enabling services included ICT infrastructure, finance, legal, corporate support, communications, property management, procurement and human resources functions. Centrelink has lead responsibility for the integration of corporate functions. Medicare Australia has lead responsibility for managing the integration of staff within the portfolio and the development of the portfolio’s staff capability and services. The integration of the portfolio’s information and communications technology platform is led by the Department of Human Services. Minister’s expectations The Minister for Human Services has chosen not to continue with the Statement of Expectations and Statement of Intent arrangement used in previous financial years. Instead, in 2009-10 the Minister wrote a letter to the Chief Executive Officer outlining Medicare Australia’s directions for the financial year. To support this letter a strategic directions document was developed. Strategic committee framework Corporate Management Committee The primary governance committee in Medicare Australia is the Corporate Management Committee—its role is to provide strategic advice to the Chief Executive Officer. Its objective is to help the Chief Executive Officer to discharge her obligations to ensure that Medicare Australia: operates effectively to deliver the government’s service delivery objectives is strategically positioned to meet future requirements has appropriate governance frameworks in place conforms with all legislative requirements. Two internal committees support the Corporate Management Committee to ensure that Medicare Australia’s business proceeds efficiently during the portfolio integration process. They are the: Business Management Committee—to provide governance and appropriate decision making for strategic issues that impact on business and operational performance in Medicare Australia Compliance Committee—to provide governance and appropriate decision making for Medicare Australia compliance responsibilities. Figure 4—Medicare Australia’s strategic committee framework at 30 June 2010 Key project steering committees Two key steering committees advise the Chief Executive Officer on the implementation and progress of major projects. These committees report directly to the Chief Executive Officer. They are the: Aged Care Steering Committee Healthcare Identifiers and e-Health Steering Committee. Audit Committee Established in line with the Financial Management and Accountability Act 1997, the Audit Committee provides assurance to the Chief Executive Officer on the appropriateness of the agency’s accountability and control framework, especially the proper use of Australian Government resources and the management of risks. It is chaired by an external member, and is directly accountable to the Chief Executive Officer. The Audit Committee generally meets quarterly. Human Services portfolio governance committees In October 2009 the Secretary and Chief Executive Officers Committee was introduced, replacing the agency heads’ meeting. In line with the service delivery reform agenda, five other portfolio committees were formed in March 2010 and met regularly. The portfolio committees are: ICT Infrastructure Integration Program Steering Committee ICT Governance Committee Portfolio Finance Committee Portfolio Customer Committee Portfolio People and Leadership Committee. Figure 5 shows the Human Services Portfolio governance committee structure at 30 June 2010. To guide work on service delivery reform across the portfolio, the Service Delivery Reform Board (SDR Board) was formed. The board is made up of the Secretary, the Chief Executive Officers of Centrelink and Medicare Australia, and all of the Deputy Secretaries and Deputy Chief Executive Officers from the Department of Human Services, Medicare Australia and Centrelink. The work of the SDR Board and each of the five portfolio governance committees sitting under the Secretary and Chief Executive Officers Committee is outlined further below. The portfolio governance committees provide assurance to the Secretary of the Department of Human Services and the Chief Executive Officers of Centrelink and Medicare Australia in the following areas: ICT Infrastructure Integration Program Steering Committee—oversees the progress of the DHS ICT infrastructure integration so that it meets its stated outcomes and returns value to government. ICT Governance Committee—provides assurance that government expectations relating to service delivery reform are delivered through the building of an integrated, innovative and responsive ICT capability. The ICT Investment Sub-committee sits under the ICT Governance Committee and is responsible for the review and assessment of ICT investment proposals. Portfolio Finance Committee—provides assurance that the management of financial resources is aligned with, and supports, the portfolio’s strategic directions and government priorities. The Portfolio Investment Subcommittee sits under the Portfolio Finance Committee and provides advice to and supports the SDR Board in relation to funding and financial management of SDR activities. Portfolio Customer Committee—provides assurance that all aspects of customer service in the portfolio support the implementation and progression of the portfolio’s strategic directions. Portfolio People and Leadership Committee—provides assurance on all cross-portfolio people matters including service delivery reform and integration within the Human Services portfolio and shared services. It also provides advice to the portfolio agencies on agency-specific people matters. SDR Board—responsible for driving and setting the direction for service delivery reform. The board also ensures that key goals and agreed outcomes are achieved and are in line with government objectives. Various committees sit under the board and assist with SDR planning, performance management, communication and coordination. External governance Interdepartmental committees Several external governance forums create the opportunity to reinforce the interdependence between policy formulation, design and implementation and to more effectively deliver outcomes for the government. The Strategic Partnerships Interdepartmental Committee provides strategic oversight of the Centrelink service delivery system. This includes strategic management of system performance as well as capability development that is in line with the government’s service delivery reform agenda. It also focuses on ensuring current service delivery approaches are effectively implemented and not compromised by the implementation of service delivery reform initiatives. The Interdepartmental committee consists of the Secretaries of the Department of Human Services (Chair); the Department of Education, Employment and Workplace Relations; and the Department of Families, Housing, Community Services and Indigenous Affairs; and the CEO of Centrelink. Figure 5—The Human Services portfolio governance committee structure A Health and Human Services Chief Executive Officers’ Forum, established by the Secretaries of the Department of Human Services and the Department of Health and Ageing, and the Chief Executive Officer of Medicare Australia facilitates the successful implementation of service delivery reform and health reform agendas. Service delivery reform A Service Delivery Reform Interdepartmental Committee chaired by the Department of Human Services first met in January 2010. Its role is to ensure alignment between service delivery reform and the outcomes of the government’s broader reform agenda. Membership of the committee is drawn from central agencies, key policy departments, service delivery organisations and the Office of the Privacy Commissioner. The Department of Human Services is also represented on the Secretaries’ Committee on Service Delivery, which is chaired by the Secretary of the Department of Finance and Deregulation. Chapter 2 Delivery of medical benefits and services Program 1.1 Case study Medicare opens a new co-located office in Belmont, Western Australia The new Medicare office in Belmont,Western Australia Perth’s inner suburb of Belmont is the site of a state-of-the-art co-located office with Medicare and Centrelink, serving the many families, migrants and elderly people in the area. The Minister for Human Services, Chris Bowen, opened the office in December 2009 and since then, customer numbers have grown from about 88 a day to more than 250. Says Medicare officer Steve Hoskins, ‘It’s been very successful. ‘People are really happy to be able to do all their Medicare and Centrelink business in one place. ‘They have also been very accepting of our credit EFTPOS, which means we have a cashless office. ‘We simply credit payments straight into people’s accounts. ‘ Four full-time Medicare Australia staff, one part-timer and one full-time Centrelink staff work together to provide services that meet people’s needs. PERFORMANCE HIGHLIGHTS Medicare processed 308.4 million services, involving more than $1 5 billion in Medicare benefits. Medicare Australia successfully implemented various budget and other government initiatives throughout 2009-10 including: the implementation of bulk bill incentives for Diagnostic Imaging and Pathology services the restructure of MBS benefits for assisted reproductive technology services to better reflect current clinical practice. Medicare Australia and the Department of Veterans’ Affairs improved processes, resulting in less red tape, more automatically paid claims and lower payment times. More services were processed electronically—rising from 76 per cent in 2008-09 to 79 per cent in 2009-10. Medicare Australia opened three new Medicare offices at Belmont and Warrawong in NSW, and Belmont in WA, and now has a network of 242 offices throughout Australia. Medicare Australia extended the Australian Childhood Immunisation Register to include notification of the H1N1 swine flu vaccine. Medicare Australia supported the Australian Organ Donor Awareness Week in February 2010, helping to raise the number of people on the Donor Register to 5 642 015 at 28 February 2010. Medicare Australia promoted the awareness of breast cancer throughout its offices and on its website. Medicare Australia sent invitations to 515 593 eligible people to participate in the National Bowel Cancer Screening program. First payments under the new Rural Locum Education Assistance Program were made in March 2010. MEDICARE Medicare, which began in 1984, ensures that all Australians have access to free or low-cost medical, optometric and hospital care while being free to choose private health services and, in special circumstances, allied health services. Medicare Australia administers Medicare enrolments and benefit payments through its network of Medicare offices and online claiming services. Medicare Australia processed 308.4 million services in 2009-10, involving more than $15 billion in Medicare benefits. The figures in the following tables are adjusted using accrual accounting. The Department of Health and Ageing develops program policy for Medicare, including the Medicare Benefits Schedule. Table 3—Medicare enrolments, claims and benefits 2008-09 2009-10 % change Enrolments People enrolled at 30 June1 21.7 million 22.1 million + 1.8% Active cards at 30 June 12.2 million 12.4 million + 1.6% 217.4 million 229.3 million +5.5% 76.6 million 79.1 million +3.3% 294.0 million 308.4 million +4.9% $48.71 $50.19 +3.0% 12.9 days 12.4days -3.9% 2.8 days 2.3days -17.9% $14.3 billion $15.4billion +7.7% Services Medicare bulk billed services Patient claimed services Total services processed Benefits Average benefit per service Average period service to lodgment2 Average period lodgment to processing3 Total benefits paid 1 People enrolled include some people who are not Australian residents, such as visitors from countries that have reciprocal health care agreements with Australia and people covered under ministerial orders. 2 Time between date of a medical service and lodgment of a Medicare claim. 3 Time between date of lodgment and processing of a Medicare claim. Analysis/trends The number of people enrolled in Medicare and the number of active Medicare cards continued to increase in line with previous years’ trends. The Medicare benefits paid totalled $15.4 billion, and the number of bulk billed services increased to 229.3 million. MEDICARE CLAIMING There were 308.4 million services processed for payment by electronic funds transfer, cheque and cash for paid accounts. Unpaid patient accounts were paid by cheques issued to the practitioner via the claimant (see Table 4 and Figure 6). Analysis/trends Bulk bill services increased to 229.3 million in 2009-10 (74.3 per cent of all Medicare services). At the same time there was an increase in services paid via electronic funds transfer and Easyclaim. This was offset by a decrease in services paid by cash. Table 4—Medicare services by bill type 2008-09 % 2009-10 % Bulk bill services 217.4 million 73.9% 229.3 million 74.3% Services paid by cash (Medicare offices) 34.1 million 11.6% 30.2 million 9.8% Services paid by simplified billing—inhospital claims lodged electronically 18.0 million 6.1% 18.5 million 6.0% Services paid by cheque to practitioner via claimant 10.9 million 3.7% 11.3 million 3.7% Services via electronic funds transfer 8.4 million 2.9% 12.1 million 3.9% Services paid by cheque to claimant 4.1 million 1.4% 3.4 million 1.1% Easyclaim account paid—patient claim paid by system (over EFTPOS network) 1.1 million 0.4% 3.7 million 1.2% 294.0 million 100% 308.4 million 100% Total services Figure 6—Medicare services by bill type MEDICARE SAFETY NET The Medicare Safety Net helps eligible individuals and families meet high medical costs for out-ofhospital medical services. The threshold for the Medicare Safety Net is indexed annually from 1 January and operates on a calendar year from 1 January to 31 December. There are three Medicare Safety Net thresholds: the original Safety Net the Concessional and Family Tax Benefit Part A the Extended Medicare Safety Net. The original Medicare Safety Net applies to everyone enrolled in Medicare. A threshold of $388.80 applies for 2010. If the difference between the specified MBS fee and the Medicare benefit paid by an individual exceeds the threshold over the calendar year, Medicare will then pay up to 100 per cent of the MBS fee for subsequent individual services. The Concessional and Family Tax Benefit Part A threshold applies to concession cardholders and families eligible for Family Tax Benefit Part A. The threshold for 2010 is $562.90 in out-of-pocket costs— that is, the difference between the Medicare benefit paid and the provider’s charge. The Extended Medicare Safety Net threshold applies to all members of the public enrolled with Medicare (apart from those who come under the Concessional and Family Tax Benefit Part A threshold)—the threshold for 2010 is $1126. Once one of these two thresholds has been reached, Medicare will pay the Medicare benefit plus 80 per cent of the out-of-pocket costs for medical services provided out-of-hospital, apart from when a capped item is claimed. Certain capped items were introduced on 1 January 2010. They place an upper limit on the amount of benefit that can be paid under the Extended Medicare Safety Net for a small number of Medicare services. For these services, the benefit will be the lower of either the capped amount or 80 per cent of the out-of-pocket costs. MEDICARE ELIGIBILITY To be eligible for Medicare benefits a person must reside in Australia and be either: an Australian citizen a permanent resident or New Zealand citizen an applicant for permanent residency and meet certain other criteria (noting that restrictions and other requirements apply to people who have applied for a parent visa) covered by a ministerial order a resident or citizen from a country with which Australia has a reciprocal health care agreement. Australian citizens who have lived overseas for more than five years, and permanent residents who have lived overseas for more than 12 months, must provide documents to show they intend to reside permanently in Australia upon their return before a Medicare card can be issued to them. MEDICARE CARDS Medicare Australia issues three different types of Medicare cards: green, blue and yellow. Green Medicare cards are issued to Australian citizens and permanent residents. Green Medicare cardholders have access to all eligible Medicare services. Blue Interim Medicare cards are issued to people who are granted eligibility for Medicare while their application for Australian permanent residency is being considered. Blue Interim Medicare cardholders have access to all eligible Medicare services. Yellow Medicare Reciprocal Health Care cards are issued to visitors to Australia who are residents of countries with which Australia has reciprocal health care agreements. Table 5—Medicare cards and Medicare levy exemptions 2008-09 2009-10 % change 7 967 483 4 561 103 -42.8% Total applications 42 328 60 859 +43.8% Accepted applications 37 672 59 366 +57.6% Rejected applications 4656 1493 -67.9% Cards Total cards issued Medicare levy exemption These cardholders’ access to Medicare services is time limited and does not cover treatment as a private patient in a public or private hospital. In administering the Medicare Levy Exemption, Medicare Australia assesses applications for a certificate that confirms the applicant was ineligible for Medicare during all or part of any financial year. If a person is not eligible for Medicare, they may apply for exemption from payment of the Medicare levy for the whole financial year or part of the year. If approved, they are issued with a Medicare Levy Exemption Certificate which is submitted with their tax return to the Australian Taxation Office. When an application is approved, a certificate is issued to the applicant. The person can then include the certificate with their tax return for that financial year and will be exempt from paying the Medicare levy for the period covered by the certificate. The Australian Taxation Office administers payment of the Medicare levy. Analysis/trends There was a 42.8 per cent reduction in the number of cards issued in 2009-10. This was due to a bulk reissue in 2008-09 resulting in a higher than usual number of cards being issued during that period. ELIGIBLE VISITORS TO AUSTRALIA The Australian Government has signed reciprocal health care agreements with some countries, which means residents of those countries can receive necessary treatment while visiting Australia. Currently, these countries are Finland, the Republic of Ireland, Italy, Malta, New Zealand, Sweden, the Netherlands, Norway, Belgium and the United Kingdom. MEDICARE AUSTRALIA SPECIAL ASSISTANCE SCHEMES Through Medicare Australia the Australian Government helps individuals meet health and community care costs arising from adverse events, such as natural disasters and terrorist attacks. Medicare Australia currently administers the following special assistance schemes: Balimed (2002) Tsunami Healthcare Assistance (2004) London Assist (2005) Bali (2005) Dahab Egypt Bombing Health Care Costs Assistance (2006) Mumbai Disaster Health Care Assistance (2008)—this scheme ceased on 28 November 2009. VETERANS’ AFFAIRS PROCESSING Medicare Australia processes claims on behalf of the Department of Veterans’ Affairs (DVA). It assesses claims and makes payments to medical, hospital and allied health providers who treat eligible veterans, their spouses and dependants (as assessed by DVA). During 2009-10 Medicare Australia (in consultation with DVA) improved a number of system and business processes. This resulted in less red tape for some health professionals, and an increase in automatic processing of claims. Medicare Australia and DVA continue to support the move to electronic claiming. For health professionals, electronic claiming means faster payment times, paperless submission and reconciliation of claims, reduced administrative burden and electronic confirmation of patient details. Analysis/trends DVA online claiming increased in 2009-10, resulting in lower administrative costs to DVA and reduced payment times for health professionals. In 2009-10, 63.5 per cent of all services processed on behalf of the DVA were received electronically. This increased from 56.6 per cent in 2008-09. VISITING MEDICAL PRACTITIONERS PROGRAM Treatment of patients in public hospitals is governed by national healthcare agreements between the Australian Government, states and territories. Under the rules of the agreements, public patients do not generate charges against the patient or against Medicare. Where a patient elects to be treated as a private patient in a public hospital, treatment may attract Medicare benefits if the rendering practitioner has the right to private practice and is not acting as a salaried employee of the public hospital. The arrangements under which medical practitioners are employed to work in public hospitals vary between the states/territories and individual hospitals. In Western Australia, the state has an arrangement whereby the various public hospital boards make payments to visiting medical practitioners for services provided at various public hospitals throughout the state. Medicare Australia and the State of Western Australia entered into an agreement on 17 June 1999, where Medicare Australia administers, on the Western Australian Government’s behalf, a fee-for-service payment and information system for visiting medical practitioners who treat public hospital patients under individual contracts with participating Western Australian public hospitals. Table 6—Veterans’ Affairs activities 2008-09 2009-10 % change 53 662 61 329 + 14.3% Services processed 21.5 million 21.7 million +0.9% Total benefits paid $2.1 billion $2.1 billion 0.0% Cards produced1 1 Personal Treatment Entitlement cards, Repatriation Pharmaceutical Benefits cards, Specific Treatment Entitlement cards and Totally Permanently Incapacitated Gold cards This service provides public non-teaching hospitals in Western Australia a real-time intranet processing system, which connects via the internet to the Medicare Australia system to access and pay invoices of visiting medical practitioners for services to public patients. In 2009-10 Medicare Australia assessed invoices valued at more than $63 million for around 317 000 paid services. EXTENSION OF 90 DAY PAY DOCTOR CHEQUE SCHEME TO SPECIALISTS The 90 Day Pay Doctor Cheque Scheme covers patient claims where the provider has not bulk billed the service, the patient has not paid the account in full and Medicare Australia has issued a pay doctor via claimant cheque. Under the 90 Day Pay Doctor Cheque Scheme, Medicare Australia will automatically cancel Medicare cheques made payable to eligible health professionals through their patient when the cheque has not been banked after 90 days from issue. The amount is then paid directly into the health professional’s nominated bank account via electronic funds transfer. Eligible health professionals include: general practitioners who do not use electronic claiming and who are registered to participate in the scheme general practitioners, specialists and consultant physicians (including pathologists) who are automatically considered eligible because they lodge their patients’ unpaid claims electronically with Medicare Australia. The scheme does not extend to optometrists, allied health professionals and dentists. From March 2010 eligible health professionals can subscribe to receive their 90 Day Pay Doctor Cheque Scheme EFT payment statements through the Medicare Australia Health Professional Online Services (HPOS) mail box. This means they no longer have to wait for EFT statements in the mail once they have subscribed to this service. CO-LOCATION Medicare Australia, in collaboration with colleagues from across the Human Services portfolio, is colocating Medicare and Centrelink services to provide easy access to a range of government services under one roof. Medicare was co-located with Centrelink in 15 sites across Australia and, during 2009-10, four more colocated sites opened in Narooma NSW, Belmont NSW, Belmont WA and Warrawong NSW. The criteria for the co-location of Medicare and Centrelink face-to-face services were signed off by the Minister on 12 March 2010. On 21 May 2010 the Minister announced the first 21 sites to be co-located by the end of 2010 as part of service delivery reform. Centrelink Customer Service Centres and Medicare offices in these locations will either physically merge to create a single point of entry or begin delivering services from both agencies in an existing site: Altona Gate VIC Mildura VIC Ballarat VIC Moree NSW Ballina NSW Mount Druitt NSW Bathurst NSW Mount Gambier SA Burwood NSW Newcastle NSW Campsie NSW Smithfield QLD Elizabeth SA Toronto NSW Frankston VIC Tuggeranong ACT Goulburn NSW Ulladulla NSW Hobart TAS West Lakes SA Ipswich QLD MEDICARE OFFICE NETWORK With the opening of three new Medicare offices at Belmont and Warrawong (NSW) and Belmont (WA) in December 2009, Medicare Australia now has a network of 242 Medicare offices located throughout Australia. Medicare offices provide the Australian public with convenient access to a full range of services, including: processing of enrolments and registrations electronic funds transfer, cheque and cash payments for claims lodgment of participating health fund claims under Medicare two-way arrangements processing of claims for the 30 per cent Private Health Insurance Rebate benefits under the Pharmaceutical Benefits Scheme statements for the Australian Childhood Immunisation Register lodgment of Organ Donor Register application forms. Across Australia there are 48 Medicare offices that are open for extended hours on Thursday or Friday evenings and 117 Medicare offices open on Saturday mornings. Medicare office locations within each state and territory can be found on Medicare Australia’s website. Medicare non-cash services are provided at five Centrelink offices located in Sutherland (NSW), Earlville (QLD), Broome (WA), Launceston (TAS) and Hastings (VIC). Medicare Australia continues to improve the design features and accessibility of its Medicare offices including a national look and feel. The current Medicare office design incorporates a combination of modular and standard seating arrangements. This seating provides the public with the convenience of comfortable, sit-down waiting. Medicare Australia has electronic queue management software installed across the branch office network. There are 138 offices with a full ticketing system and sit-down waiting facilities, as well as the queue management software. The remaining 109 offices (including five Medicare non-cash service sites located at Centrelink offices) use this software to record and report on all transactions, including volumes, types and time to complete. This system allows managers to best use staff, identify trends in requirements and tailor staff training effectively to better meet the needs of the public. MEDICARE AUSTRALIA ACCESS POINTS There are 886 Medicare Australia Access Point booths located across Australia which complement the Medicare office network by providing easy access to Medicare claiming and information. Medicare Australia Access Points are claiming booths that are usually located in pharmacies, post offices or community centres. To access Medicare services, members of the public simply pick up a handset to be connected to a Medicare Australia service officer, who will guide them through the claiming process step-by-step. If paid accounts are lodged at these facilities and the EFT option is selected, the claimant just needs to supply the operator with the BSB and account number of their chosen bank account and the refund will be deposited into the claimant’s account. For unpaid accounts, a cheque made payable to the doctor will be forwarded to the claimant. The service officer can also assist with enquires about lost Medicare cards, change of address and other information on services such as the PBS, Australian Organ Donor Register, Australian Childhood Immunisation Register, Family Assistance payments and the Medicare Safety Net. The locations of Medicare Australia Access Points are available on Medicare Australia’s website: www.medicareaustralia.gov.au. MEDICARE TEEN DENTAL PLAN On 1 July 2008 the Australian Government introduced the Medicare Teen Dental Plan to help with the cost of an annual dental preventative check. The plan makes it more affordable for families to keep their teenagers’ teeth in good health. Over one million teenagers are eligible for the Medicare Teen Dental Plan each year. Eligible teenagers are aged between 12 and 17, entitled to Medicare and fit one of the following categories: they are receiving Family Tax Benefit Part A, ABSTUDY, Carer Payment, Disability Support Pension, Parenting Payment, Special Benefit, Youth Allowance their family/carer/guardian receives Family Tax Benefit Part A, Parenting Payment or the Double Orphan Pension for the teenager their partner receives Family Tax Benefit Part A or Parenting Payment they are 16 years or older and receiving financial assistance under the Veterans’ Children Education Scheme (VCES) or the Military Rehabilitation and Compensation Act Education and Training Scheme (MRCAETS) from the Department of Veterans’ Affairs. In January and February each year Medicare Australia sends eligible families and teenagers a voucher for a preventative dental check using client information provided by Centrelink or the Department of Veterans’ Affairs. Teenagers who become eligible later in the year are sent a voucher once Medicare Australia receives information about their entitlement. In 2009-10 Medicare Australia processed approximately 423 000 services and paid more than $63 million in benefits. AUSTRALIAN CHILDHOOD IMMUNISATION REGISTER The Australian Childhood Immunisation Register was established in January 1996 to improve the rate of age-appropriate immunisation. The register also helps parents and immunisation providers keep track of a child’s immunisation status, regardless of where the child was immunised. Details of vaccinations given to children under the age of seven who live in Australia are recorded on the register and are available on request to authorised immunisation providers and each child’s parent or guardian. This data also helps determine eligibility for the Maternity Immunisation Allowance and Child Care Benefit available through the Family Assistance Office. Medicare Australia’s website gives providers a secure channel to access and update children’s immunisation details. Health professionals use the register to monitor immunisation coverage and service delivery and to identify regions at risk during disease outbreaks. Immunisation coverage information is available at the state, territory or national level. Data from the Australian Childhood Immunisation Register is used to provide an immunisation history statement for parents and guardians. From September 2009 Medicare Australia improved this service by enabling parents and guardians to access immunisation history statements for children until they turn 14. Previously this information was only available until children turned seven. In 2009 Medicare Australia further improved the register by allowing the notification of the new H1N1 Panvax (swine flu) vaccine given to children. Children had been identified in the media as one of the atrisk groups earmarked for the vaccine and this change means important health information will be available to parents, immunisation providers, other health professionals for research purposes and to government long after the child has been immunised. Table 7—Australian Childhood Immunisation Register 2008-09 2009-10 % change Valid immunisation episodes recorded at 30 June 4.6 million 4.7 million +2.2% Children under 7 years registered at 30 June 2.0 million 2.1 million +5.0% Total amount paid to immunisation providers1 $9.1 million $8.9 million -2.2% Children registered with appropriate immunisation coverage at 30 June 1 Children aged 12-15 months 91.3% 91.5% +0.2% Children aged 24-27 months 92.9% 92.4% -0.5% Children aged 60-63 months 82.4% 89.6% +7.2% Payments made on completion of the aged-based immunisation schedule of a child, not registration of a child. At 30 June 2010, 2.1 million children under the age of seven were included on the register. In 2009-10, 180 231 immunisation history statements had been viewed online and 84 677 immunisation history statements had been given to parents at Medicare offices. Almost $9 million was paid to immunisation providers and 4.7 million valid immunisations were recorded. Analysis/trends June 2010 immunisation coverage showed an increase of 7.2 per cent for the 60-63 month age group since the same quarter last year. The increase in coverage can be linked to changes in the Australian Childhood Immunisation Register’s assessment of children in the 60-63 month age group to bring them in line with the assessment for all other age groups. These changes, which affect children turning five from 1 January 2010, mean that children are considered overdue for their vaccinations aged four years and one month, instead of at five years of age. This has encouraged parents to get their children immunised earlier, which has in turn positively affected the number of children assessed as fully immunised for this age group. AUSTRALIAN DEFENCE FORCE FAMILY HEALTHCARE PROGRAM The Australian Defence Force Family Healthcare Program began on 1 May 2009. It is a governmentestablished trial to provide free basic medical and dental care to families of Australian Defence Force personnel living in remote and regional locations. It supports a broader defence recruitment and retention strategy. Medicare Australia administers the program on behalf of the Department of Defence and provides an extra payment to registered medical practitioners who bulk bill eligible services for Australian Defence Force family members within an accepted location. The Australian Defence Force Family Healthcare Program is open to families located in: Queensland—Cairns, Mt Isa, Weipa, Thursday Island, Townsville, Mission Beach and Tully Victoria—Sale and Puckapunyal New South Wales—Singleton Northern Territory—Darwin, Nhulunbuy, Alice Springs and Katherine Western Australia—Broome, Derby, Kununurra, Karratha, Carnarvon, Exmouth, Port Hedland, Tom Price and Newman. Table 8—Australian Defence Force Family Healthcare Program 2008-09 2009-10 Number of registered provider locations 106 252 Number of registered dependants 625 3810 Number of services provided 107 4310 Total amount paid N/A $0.08 million Analysis/trends The Australian Defence Force Family Healthcare Program began on 1 May 2009, with the first payments to service providers being made in July 2009. The growth in number of services provided and the numbers of registered dependants and registered provider locations reflects that 2009-10 was the first full financial year of the program. AUSTRALIAN ORGAN DONOR REGISTER Medicare Australia administers the Australian Organ Donor Register on behalf of the Australian Government. The Donor Register provides a simple way for people to record their consent (or objection) to organ and/or tissue donation. If a registered person dies, the Donor Register provides access to authorised medical personnel to verify the person’s donation decision 24 hours a day, seven days a week, anywhere in Australia. Medicare Australia supported the Australian Organ Donor Awareness Week in February 2010. This involved targeted promotions in Medicare offices, through the Medicare Australia website and alongside the Brumbies ‘sign on to save lives’. More than 5.6 million people have registered their organ and/or tissue donation decision on the Donor Register. This figure includes the intent registrations of 16-17 year olds. The Donor Register website provides an online mechanism for people to register their donation decision with general information about organ and tissue donation for transplantation and the number of registered organ and tissue donors in Australia. Go to the Medicare Australia website: www.medicareaustralia.gov.au/public/services/aodr/register.jsp. Analysis/trends There has been a steady increase in the numbers of individuals registering their donation decision over the last year. The increase in registrations is attributed to a number of factors including Medicare Australia’s partnership with the Brumbies in promoting organ donation at home games as well as the Australian Organ Donor Awareness Week held in February. Table 9—Australian Organ Donor Register 1 2008-09 2009-10 % change Number of consent registrations (including intent registrations of 16-17 year olds) 1 286 342 1 395 792 +8.5% Number of registrations of potential organ donors1 4 303 639 4 276 990 -0.6% Number of serviced calls to inquiry line 26 320 23 020 -12.5% Potential organ donors are those people who had previously registered their intent but have not updated this to consent to donate. Table 10—Compensation recovery cases and benefits 2008-09 2009-10 % change Cases finalised 45 057 47 876 +6.3% Total amount of benefits recovered $33.2 million $37.9 million +14.2% COMPENSATION RECOVERY PROGRAM Medicare Australia administers the Compensation Recovery Program on behalf of the Department of Health and Ageing under the Health and Other Services (Compensation) Act 1995. The program began in February 1996 and prevents ‘double dipping’ in Medicare benefits, nursing home benefits and residential care subsidies paid by the Australian Government when a person receives compensation for an injury or illness by way of judgment or settlement. If the amount of compensation is more than $5000 (including costs), the value of the Medicare benefits, nursing home or residential aged care subsidies must be repaid. Medicare Australia recovers only the amount of benefits or subsidies paid for those services relating to the compensable injury or illness. Medicare Australia issues a Medicare history statement listing all Medicare services received from the date of injury to the date of judgment or settlement as a means of identifying the amount of benefits or subsidies to be recovered. The claimant must identify the services relating to the compensable injury or illness and return the Medicare history statement. These services are then calculated to determine the repayment amount, if any. Analysis/trends An additional 2819 compensation cases were processed in 2009-10, resulting in an additional $4.7 million in past Medicare and residential care benefits being recovered. EXTERNAL BREAST PROSTHESES REIMBURSEMENT PROGRAM Medicare Australia administers the External Breast Prostheses Reimbursement Program on behalf of the Department of Health and Ageing. Reimbursements for the program began on 24 November 2008. It offers a nationally consistent approach in providing financial support towards the cost of prostheses. All Australian women who have had a mastectomy as a result of breast cancer and hold a current Medicare entitlement are eligible to be reimbursed up to $400 for new or replacement external breast prostheses. During October 2009 Medicare Australia promoted the awareness of breast cancer, together with Breast Cancer Network Australia, by publicising the program throughout Medicare offices and on its website. Table 11—External Breast Prostheses Reimbursement Program 2008-09 2009-10 Number of claims processed 10 780 13 315 Total amount paid $3.6 million $4.8 million Note: In 2009-10 program participation is for a full 12-month period. The program participation in 2008-09 was for a period of seven month Table 12—General Practice Immunisation Incentive payments 1 2008-09 2009-10 % change Practices registered (calculated at the time of the May quarterly payment calculation) 5508 5555 +0.9% Outcomes payments1 $18.8 million $20.2 million +7.4% Average outcomes payment $1052 $1086 +3.2% Outcomes payments are made to practices who have reached the required target level. Information about the program is available on Medicare Australia’s website, in Medicare offices and from Breast Cancer Nurses associated with the McGrath Foundation. Links are available on Medicare Australia’s website to the Breast Cancer Network Australia and National Breast and Ovarian Cancer Centre websites. At 30 June 2010 Medicare Australia had received 13 315 claims and has reimbursed eligible Australian women over $4.8 million. GENERAL PRACTICE immunisation INCENTIVE The General Practice Immunisation Incentive provides financial incentives to general practitioners who monitor, promote and provide immunisations to children under seven years of age. The program aims to encourage at least 90 per cent of medical practices to achieve immunisation coverage of 90 per cent of children under the age of seven. Registered general practices receive a quarterly outcomes payment if they achieve this target of full immunisations for children who have attended the practice. Analysis/trends At 30 June 2010 the program involved 5555 registered practices. The average immunisation coverage rate for practices was 91.4 per cent for 2009-10, with 77.2 per cent of participating practices achieving rates of 90 per cent or higher. GENERAL PRACTICE REGISTRARS’ RURAL INCENTIVE PAYMENTS SCHEME The General Practice Registrars’ Rural Incentive Payment Scheme began in 2001 and promotes careers in rural medicine, increasing the number of doctors in rural and regional areas of Australia. The scheme provides incentive payments to general practice registrars participating in the Australian General Practice Training program for training in rural areas. Eligibility is assessed on registrars training in Rural, Remote and Metropolitan Areas 3-7 locations and payment levels are based on the General Practice Accessibility and Remoteness Index of Australia. Table 13—General Practice Registrars’ Rural Incentive Payments Scheme 2008-09 2009-10 % change Number of medical practitioners paid 587 664 + 13.1% Number of payments made 1092 1248 + 14.3% Total amount paid $13.3 million $17.3 million +30.1% 2008-09 2009-10 % change Services processed1 1 024 969 1 099 690 +7.3% Total amount paid2 $263.6 million $294.0 million +11.5% Table 14—Hearing Services Program services and payments 1 Service provided to individuals 2 Payments made to hearing contractors From 1 July 2010 a new General Practice Rural Incentive Program system will replace the General Practice Registrars’ Rural Incentive Payment Scheme. Payments to registrars will be made according to the Australian Standard Geographical Classification—Remoteness Area. Analysis/trends In 2009-10 the value of payments increased, reflecting the increased number of GP registrars receiving payments as well as an increased number of payments made under the scheme. HEARING SERVICES PROGRAM The Australian Government provides hearing services and products to eligible people. Medicare Australia processes and pays claims to accredited hearing service contracts for the Hearing Services Program on behalf of the Office of Hearing Services, within the Department of Health and Ageing. The Office of Hearing Services manages the program’s policy and eligibility criteria. In 2009-10 Medicare Australia processed more than one million services and made payments totalling $294 million to accredited hearing service contractors. On 1 July 2008 Medicare Australia began receiving 100 per cent of claims electronically. Analysis/trends An extra 74 721 services were provided to individuals in 2009-10, resulting in an additional $30.4 million in payments to hearing contractors. HIGHER EDUCATION CONTRIBUTION SCHEME REIMBURSEMENT SCHEME The Higher Education Contribution Scheme (HECS) Reimbursement Scheme encourages medical graduates to pursue a career in rural medicine and increase the number of doctors in rural and regional areas. Access to health services in these communities improves as more doctors work in these areas. Under the scheme, eligible graduates who complete their medical degree in 2000 or later have one-fifth of their HECS debt reimbursed for each year of training undertaken or service provided in Rural, Remote and Metropolitan Area (RRMA) 3-7 locations. Table 15—HECS Reimbursement Scheme 2008-09 2009-10 % change Number of medical graduates paid 450 462 +2.7% Number of payments made 699 826 +18.2% Total amount paid $4.2 million $5.4 million +28.6% From 1 July 2010 the HECS Reimbursement Scheme will scale payments to provide the greatest rewards for medical practitioners working in the most remote areas and the RRMA classification system will be replaced with the Australian Standard Geographical Classification—Remoteness Area system. Analysis/trends In 2009-10 the value of payments increased, reflecting a slightly higher number of medical graduates participating in the scheme as well as an increased number of payments made under it. MEDICAL INDEMNITY The Australian Government’s medical indemnity framework consists of five schemes to strengthen the longer-term viability of the medical insurance industry and create an environment in which the industry can operate successfully. This is achieved by providing financial support to reduce the impact of large claims and by making medical indemnity insurance more affordable for medical practitioners. Medicare Australia administers the schemes under the Medical Indemnity Act 2002 and associated legislation. United Medical Protection Support Payments The United Medical Protection Support Payment was introduced in 2002 when the Medical Defence Organisation United Medical Protection (now known as Avant Insurance Limited) entered provisional financial liquidation. The payment provides ongoing assurance for medical professionals who were members of United Medical Protection on 30 June 2000, in the form of indemnity for past incidents. To provide this assurance, the government agreed to fund most of these claims with members of United Medical Protection funding around one-third of the arrangement over six years through the support payments (formerly Incurred-But-Not-Reported Levy). This contribution ratio was subsequently reduced to four years. In 2008-09 the United Medical Protection Support Payment operated for the last time. Outstanding debts of $6277 are still being recovered. Incurred-But-Not-Reported Indemnity Claims Scheme Under the Incurred-But-Not-Reported Indemnity Claims Scheme, the government covers the costs of claims from medical defence organisations that do not have adequate reserves to cover their liabilities. United Medical Protection Limited (now known as Avant Insurance Limited) is the only medical defence organisation actively participating in the scheme. The scheme covers Incurred-But-Not- Reported indemnity claims and united Medical Protection support payments. Ongoing costs associated with the scheme are partly funded through a contribution payment (the united Medical Protection Support Payment) imposed on those people who were members of united Medical Protection Limited on 30 June 2000. Table 16—Incurred-But-Not-Reported Indemnity Claims Scheme 2008-09 2009-10 Number of claims received 197 184 Total benefits paid $12.1 million $9.5 million Analysis/trends The reduction in claims received in 2009-10 is due to the demand-driven nature of this scheme. For example, a number of years can elapse between the date of a medical incident and the date that legal action against the practitioner is initiated. It may also take a number of years to finalise a claim once it is initiated and the costs of individual claims is also variable. A small number of large claims may significantly affect the overall cost of the scheme. High Cost Claims Indemnity Scheme Under the High Cost Claims Indemnity Scheme, the government funds 50 per cent of the cost of medical indemnity insurance payouts that are greater than the applicable threshold amount, up to the limit of a medical practitioner’s insurance cover. This scheme has three threshold levels that depend on the date the claim was first notified to the insurer. Notification dates (inclusive) Threshold amount 1 January to 21 October 2003 $2 million 22 October to 31 December 2003 $500 000 On or after 1 January 2004 $300 000 In 2009-10 Medicare Australia paid benefits of $21.4 million for the 98 claims received. Analysis/trends The increase in claims received in 2009-10 reflects the demand-driven nature of this scheme. The number of medical negligence claims exceeding the scheme’s threshold amount is only a small proportion of the total number of medical negligence claims occurring each year and can be expected to vary from year to year. The total benefits paid each year are also influenced by the amount of each individual claim, which is highly variable. A small number of large claims may significantly affect the overall cost of the scheme. Table 17—High Cost Claims Indemnity Scheme claims processed 2008-09 2009-10 Number of claims received 82 98 Total benefits paid $19.5 million $21.4 million Exceptional Claims Indemnity Scheme The Exceptional Claims Indemnity Scheme was introduced in November 2003. Under this scheme, medical practitioners are protected against personal liability for eligible claims that exceed the level of their insurance cover. The scheme has two threshold levels that depend on the date the claim was first notified to the insurer. No claims have been submitted against this scheme. Notification dates (inclusive) Threshold amount 1 January to30 June 2003 $15 million On or after 1 July 2003 $20 million Run-off Cover Scheme support payment Under the Run-off Cover Scheme, the government guarantees funding for claims against eligible medical practitioners who have left the private medical workforce and been provided with free run-off cover. The Run-Off-Cover Support Payment is imposed as a tax on each medical indemnity insurer for each contribution year. This is used to fund eligible claims made under the Run-Off Cover Scheme. Under the scheme, medical indemnity insurers will be reimbursed implementation and compliance costs under section 34ZN(1)(c) of the Medical Indemnity Act 2002. Analysis/trends Administration fees are generally increased annually, therefore it is expected these fees will continue to rise in future years. There is no expectation of any further applications for implementation fees as all medical indemnity insurers have been paid for developing and implementing their IT systems. Run-off Cover Scheme Under the Run-off Cover Scheme, the government covers the cost of claims for eligible doctors who have left the private medical workforce. The government uses funds paid into the Run-off Cover Scheme by medical indemnity insurers to cover incidents that occur in connection with a doctor’s practice as a medical practitioner. Indemnity cover for eligible doctors will mirror the last claims arrangement they had with their medical indemnity insurer. Analysis/trends The increase in Run-off Cover Scheme claims is consistent with an expected increase in the number of medical practitioners becoming eligible for the scheme since the scheme commenced in 2004. Medical practitioners may become eligible for the scheme when they cease private medical practice, for example through retirement (after a three-year qualifying period), maternity leave, transferring to the public hospital system or death. Table 18—Run-off Cover Scheme support payment 2008-09 2009-10 Total implementation fees paid $0.3 million N/A Total administration fees paid $0.3 million $0.8 million 2008-09 2009-10 Number of claims received 21 28 Total benefits paid $1.6 million $2.1 million Table 19—Run-off Cover Scheme Premium Support Scheme Under the Premium Support Scheme, eligible medical practitioners receive financial assistance through a subsidised reduction in their insurance premium costs, effective from 1 July 2004. Insurers are then reimbursed the subsidised amount. The Premium Support Scheme ensures that if a doctor’s gross medical indemnity costs exceed 7.5 per cent of their gross private medical income, they will pay 20 cents in the dollar for the cost of the premium beyond that threshold limit. Analysis/trends Actual income is used as part of the formula for determining medical practitioners’ eligibility for a subsidy under the Premium Support Scheme. Given income generally rises each year the 2009-10 figures are within the expected variances. Competitive Advantage Payment Under the Competitive Advantage Payment scheme, medical indemnity insurers that benefit from the Incurred-But-Not-Reported Indemnity Claims Scheme are required to make a payment to the government that reflects their level of competitive advantage. In 2009-10 no competitive advantage payments were made under the scheme. MENTAL HEALTH NURSE INCENTIVE PROGRAM The Mental Health Nurse Incentive Program began on 1 July 2007. It provides funding to communitybased general practices, private psychiatric practices and other eligible organisations to engage mental health nurses in providing coordinated clinical care for people with severe mental health disorders. Based on a set of defined criteria, general practitioners and psychiatrists determine whether patients have a severe mental health disorder and would benefit from receiving mental health services under this initiative. Analysis/trends The increase in payments under the Mental Health Nurse Incentive Program for 2009-10 is due to a significant increase in new organisations registering for the initiative and the fact that participating organisations have claimed more weekly sessions. Table 20—Premium Support Scheme participation and revenue 2008-09 2009-10 Total eligible practitioners 2567 2439 Total amount paid $16.1 million $17.2 million Total administration fees $2.4 million $2.4 million Table 21—Mental Health Nurse Incentive Program 1 2008-09 2009-10 % change Number of practices participating at 30 June 472 629 +33.3% Total incentive amounts paid $12.7 million $21.1 million +66.1% Number of eligible organisations in receipt of establishment payments 90 661 -26.7% Total establishment amounts paid $0.8 million $0.5 million -37.5% Total amount paid $13.5 million $21.6 million +60.0% This number is expected to decline annually as eligible organisations complete registration NATIONAL BOWEL CANCER SCREENING REGISTER The National Bowel Cancer Screening Program aims to reduce the morbidity (that is, the rate of incidence of a disease) and mortality associated with bowel cancer. The second phase of the National Bowel Cancer Screening Program began on 1 July 2008 and offers testing to people turning 50 years of age between January 2008 and December 2010, and those turning 55 or 65 between July 2008 and December 2010. Medicare Australia administers the National Bowel Cancer Screening Register on behalf of the Department of Health and Ageing. Medicare Australia is responsible for: identifying and inviting eligible participants to screen using Medicare and Department of Veterans’ Affairs enrolment files issuing reminders to participants recording participants’ screening and detection histories operating the Program Information Line for the general public and health professionals overseeing the mailing house services for the program making payments to medical professionals for providing information to the register about consultations and medical procedures for program participants who have received positive test results. During 2009-10 Medicare Australia sent invitations to 515 593 eligible people to participate in the program. Table 22—National Bowel Cancer Screening Register 2008-09 2009-10 % change Invitations distributed 789 697 515 593 -34.7% Faecal occult blood test results processed 290 645 291 159 +0.2% Replacement FOBT kits issued to remedial cohort NIL 385 816 N/A Information line calls received 2008-09 2009-10 % change 91 656 63 114 -31.1% Analysis/trends From May 2009 the Department of Health and Ageing suspended program invitations as a result of possible unreliability of the self-test kits. The program recommenced in November 2009. The invitation volumes distributed by the program register were significantly lower compared to 2008-09 due to the suspension of the program. PRACTICE INCENTIVES PROGRAM The Practice Incentives Program (PIP) encourages continuing improvements in general practice through financial incentives to support quality care and improve access and health outcomes for patients. To be eligible for the PIP, practices must be accredited or registered for accreditation against the Royal Australian College of General Practitioners’ Standards for General Practices and be fully accredited within 12 months of joining the PIP payments are in addition to other income earned by general practitioners and the practice, such as patient payments and Medicare rebates. Medicare Australia administers the program on behalf of the Department of Health and Ageing, which has overall policy responsibility for the program, including determining eligibility criteria. Practices may qualify for any or all of the 13 program incentives in Table 23. At 30 June 2010, 4881 practices were registered as participating in the program. Incentive payments of approximately $229 million were provided during 2009-10. Analysis/trends Overall the number of practices participating in the program increased in comparison to last year’s figures. There was, however, a decrease in the total amount paid due to the abolition of the Information Management/Information Technology (IM/IT) Incentive. This was replaced by the eHealth Incentive which has had a lower participation rate than the IM/IT Incentive. There was also a significant increase in the number of Service Incentive Payments due to the introduction of the Aged Care Access Incentive. Table 23—Types of Practice Incentives Program payments Payment type Description After hours Incentive payments to encourage general practices to ensure their patients have access to quality after-hours care. Aged care access Service Incentive Payments (SIPs) to GPs to encourage increased and continuing services in Commonwealth-funded residential aged care facilities. Asthma Sign-on payments to practices to encourage GPs to better manage the clinical care of people with moderate to severe asthma. SIPs to GPs for each asthma cycle of care completed for a patient with moderate to severe asthma. Payment type Description Cervical screening Sign-on and outcomes payments to practices to encourage GPs to screen underscreened women (i.e. women who have not had a cervical smear in the past four years) and to increase overall screening rates. SIPs to GPs for each cervical smear taken on an under-screened woman aged between 20 and 69 years. Diabetes Sign-on and outcomes payments to practices to encourage GPs to provide earlier diagnosis and effective management of people with established diabetes mellitus. SIPs to GPs for completing an annual diabetes cycle of care. Domestic violence Incentive payments to practices to encourage general practices in rural and remote areas to act as a referral point for women experiencing domestic violence. eHealth Incentive payments to practices to encourage the adoption of new eHealth technology as it becomes available to assist practices in improving administration processes and the quality of care provided to patients. Indigenous health Payments to practices to provide better health care for Aboriginal and Torres Strait Islander patients, including best-practice management of chronic disease. Practice nurse Incentive payments to practices in rural and remote areas or eligible urban areas of workforce shortage and to Aboriginal Medical Services, to support them to employ a practice nurse, Aboriginal health worker and/or allied health worker (urban areas only). Procedural GP payment Incentive payments to practices to encourage rural GPs to provide procedural services. Quality prescribing Payments to practices to encourage them to keep up to date with information on the quality use of medicine by participation in a range of activities recognised or provided by the National Prescribing Service. Rural loading A rural loading is applied to the PIP payments of practices where the main location is outside a capital city or other major metropolitan area. Teaching Incentive payments to practices to encourage them to provide teaching sessions to undergraduate medical students, to ensure the practitioners of tomorrow are appropriately trained and have actual experience of general practice. Table 24—Practice Incentives Program services 2008-09 2009-10 % change 4804 4881 + 1.6% 4595 4643 +1.0% Practices with a SWPE value of more than 2000 must provide at least 15 hours of afterhours care for regular practice patients 2943 2936 -0.2% Tier 3—Provide all after-hours care for regular practice patients, 24 hours a day, seven days a week 1298 1301 +0.2% 178 231 +29.8% Sign-on1 178 240 +34.8% Outcomes4 3324 3306 -0.5% Sign-on1 180 237 +31.7% Outcomes4 2185 2129 -2.6% 3346 3830 + 14.5% Sign-on1 853 N/A Outcomes4 110 N/A 2451 +4.9% Number of practices participating at the time of the May quarterly payment calculation After hours Tier 1—Ensuring all regular practice patients have access to care from a doctor, 24 hours a day, seven days a week Tier 2—Practices with a SWPE value of 2000 or less must provide at least 10 hours of afterhours care for regular practice patients Asthma Sign-on1 Cervical screening Diabetes eHealth Indigenous health Practice nurse 2337 Procedural GP 333 656 +97.0% Quality prescribing 839 959 + 14.3% Teaching 891 989 + 11.0% 101 255 130 124 +28.5% 157 217 +38.2% 14 177 48 9513 +245.3% $298.2 million $229.2 million -23.1% Number of teaching sessions Domestic violence Service Incentive Payments2 Asthma Cervical Diabetes Aged Care Access Incentive Total amount paid (at 30 June) 1 Sign-on figures show the number of new practices that signed on for the incentive in 2009-10. 2 Service Incentive Payments include unique providers who have received a payment for the Aged Care Access Incentive, the Asthma Incentive, Cervical Screening Incentive and Diabetes Incentive. 3 This is the total number of payments for Service Incentive Payments which includes Asthma, Diabetes, Cervical and also includes the SIP Aged Care Incentive Payment. 4 Outcome payments are made to practices who have reached the specified target level required to receive the incentive under the program. Note: Key business results include additional information relating to the following: After hours—amendments to the 10 and 15 hour categories. Cervical screening—addition of sign-on and outcomes payments Diabetes—addition of sign-on and outcomes payments Services Incentive Payments—additional reporting categories Table 25—Rural Procedural Grants Program 2008-09 2009-10 % change Number of providers paid 1658 1552 -6.4% Number of payments made 3726 3635 -2.4% Total amount paid $14.3 million $16.1 million +12.6% RURAL PROCEDURAL GRANTS PROGRAM The Rural Procedural Grants Program, formerly known as the Training for Rural and Remote Procedural General Practitioner’s Program, provides financial assistance to general practitioners who provide procedural or emergency medicine services in rural and remote areas to attend training courses on maintaining and improving skills. For procedural GPs in Rural, Remote and Metropolitan Areas (RRMA) 2-7, the program provides a grant for the cost of up to 10 days of training, to a total of $20 000 per GP per financial year. For emergency medicine GPs in RRMA 3-7, the program provides a grant for the cost of up to three days of training, to a total of $6000 per GP per financial year. Eligibility for the Rural Procedural Grants Program is determined by the Australian College of Rural and Remote Medicine and the Royal Australian College of General Practitioners. From 1 July 2010 the RRMA classification system will be replaced with the Australian Standard Geographical Classification— Remoteness Area system. Analysis/trends The Rural Procedural Grants Programs is a demand-driven program. In 2009-10 the value of payments increased due in part to providers taking full advantage of the maximum 10 days of training available to GPs under this program. RURAL LOCUM EDUCATION ASSISTANCE PROGRAM The Rural Locum Education Assistance Program was established under the 2009-10 Budget initiative as a new component to the Rural Procedural Grants Program. The Rural Locum Education Assistance Program provides payments to urban GPs who undertake emergency medicine training and commit to undertake a four-week rural locum placement within two years of the first payment. A maximum of 30 providers could participate in 2009-10 with first payments for this initiative made in March 2010. Table 26—Rural Locum Education Assistance Program 2009-10 Number of general practitioners paid 15 Number of payments made 24 Total amount paid $76 000 Analysis/trends The pilot Rural Locum Education Assistance Program was launched in January 2010 and payments in 2009-10 reflect the number of GPs that completed emergency medicine training and received payments before 30 June 2010. RURAL RETENTION PROGRAM The Rural Retention Program (RRP) provides incentive payments to increase recruitment and retention of general practitioners in rural and remote Australia. The RRP recognises and rewards the contribution of GPs who practice in rural and remote areas. These communities benefit through improved access to general practice services and continuity of health care. The program consists of two components: a Central Payments System administered by Medicare Australia which assesses eligibility using doctors’ Medicare and DVA service data. Payments are based on Medicare Australia records of eligible services provided in eligible rural locations a Flexible Payments System administered by Medicare Australia and Rural Workforce Agencies based in the states and the Northern Territory. This component caters for doctors who are not billing Medicare and those working in Aboriginal Medical Services, Royal Flying Doctor Services or as statesalaried doctors. Payment amounts are provided by Rural Workforce Agencies and paid by Medicare Australia. From 1 July 2010 a new General Practice Rural Incentive Program system will replace the RRP Payments to GPs will be made according to the Australian Standard Geographical Classification— Remoteness Area system. Analysis/trends In 2009-10 the value of payments increased, reflecting a higher number of payments made under the program. Table 27—Rural Retention Program 2008-09 2009-10 % change Number of payments made 2293 2362 +3.0% Total amount paid $22.3 million $24.6 million +10.3% 2008-09 2009-10 % change Number of memberships registered 5.5 million 5.7 million +3.6% Total paid in cash claims $2.3 million $2.2 million -4.3% Total paid to health funds $4.0 billion $4.3 billion +7.5% Table 28—30% Rebate on Private Health Insurance 30% REBATE ON PRIVATE HEALTH INSURANCE The 30% Rebate on Private Health Insurance was introduced on 1 January 1999. The rebate provides reimbursement or a discount of 30 per cent of the cost of private health insurance cover. It is available to all Australians who are eligible for Medicare and have a complying health insurance policy. On 1 April 2005 the rebate was increased to 35 per cent for people aged 65 to 69 years and to 40 per cent for people aged 70 years and over. The rebates can be claimed in one of three ways: an up-front reduction in the cost of the premium—the Premium Reduction Scheme a direct cash payment at a Medicare Australia office—the Incentive Payments Scheme a tax offset in annual income tax returns. The first two methods of claiming the rebates are administered by Medicare Australia, and the Australian Taxation Office administers the third method. The authority for the rebates and Medicare Australia’s responsibilities for them are contained in the Private Health Insurance Act 2007. During 2009-10 a total of $4.3 billion was paid by Medicare Australia. The number of registered health fund memberships increased by 3.6 per cent. Cash claims paid directly by Medicare Australia to individuals decreased by 4.3 per cent to $2.2 million. This reflects a decrease in the number of policyholders opting to claim the rebate over the counter at a Medicare office rather than through a reduction in their premiums or through their tax return. Total health fund payments increased to $4.3 billion, an increase of 7.5 per cent. Analysis/trends The total amount paid for the private health insurance rebate increased during 2009-10. This variance is due to a larger volume of memberships being registered and an increase in premium costs. MEDICAL AND PHARMACEUTICAL ADVISERS Medicare Australia employs over 50 doctors and pharmacists to provide professional advice both within Medicare Australia and to external stakeholders. These advisers meet regularly with health provider organisations and registration authorities across Australia to facilitate the flow of information and feedback, and provide extensive knowledge and expertise in support of a range of activities including: enhancing the quality and national consistency of the information Medicare Australia provides to its stakeholders responding to requests for advice assisting with the interpretation and assessment of complex claims assisting with the development of education products delivering education to various forums, including events run by provider organisations including Australian General Practice Accreditation Limited (AGPAL), Royal Australian College of General Practitioners (RACGP) GP’09, Rural Medicine Australia and the Australasian College of Dermatologists. Chapter 3 Delivery of pharmaceutical benefits and services Program 1.2 Case Study Closing the Gap (CTG)—PBS Co-payment Measure ‘Collaboration was the winner of the day. ’ Medicare Australia and the Department of Health and Ageing worked collaboratively to overcome barriers to improving access to medicine for Indigenous and Torres Strait Islander people. The PBS Co-payment Measure enables eligible Indigenous and Torres Strait Islander patients to receive their PBS medicines at a lower cost. The PBS Co-payment Measure is one of the 14 elements of the National Partnership Agreement of Closing the Gap in Indigenous Health Outcomes that aims to close the life expectancy gap between Indigenous and non Indigenous Australians within a generation. Medicare Australia and the Department of Health and Ageing worked closely together to ensure that a streamlined, user-friendly solution could be implemented. A seamless online payments arrangement was implemented and has facilitated greater pharmacy engagement in the measure. The work Medicare Australia has done allows payments to pharmacies to be streamlined and timely, enabling pharmacies to supply patients with their medicines at their convenience. Eligible Indigenous and Torres Strait Islander patients who have a Medicare card can now present their CTG prescription at any pharmacy, and receive their medicines at a reduced rate of $5.40 instead of paying $33.30. Eligible Indigenous and Torres Strait Islander patients with a concessional card can, on presentation of their CTG prescription to their pharmacy, receive their medicines for free. Through collaboration with stakeholders, Medicare Australia and the Department of Health and Ageing devised a solution that has ensured positive outcomes for Indigenous and Torres Strait Islander patients. PERFORMANCE HIGHLIGHTS 197.7 million services were processed under the Pharmaceutical Benefits Scheme and Repatriation Pharmaceutical Benefits Scheme. The PBS Safety Net thresholds were adjusted from 1 January 2010: the general threshold is $1281.30 and the concession threshold is $324. The number of approved suppliers grew by 0.85 per cent from 5356 in 2008-09 to 5402 this year. The Fifth Community Pharmacy Agreement will come into effect on 1 July 2010. Medicare Australia is involved with 12 initiatives under the agreement. Under the National Health Care Agreement, the Australian Government, states and territories have reformed the supply of pharmaceutical benefits to eligible patients in public hospitals. PHARMACEUTICAL BENEFITS SCHEME The Pharmaceutical Benefits Scheme (PBS) subsidises the cost of listed prescription medicine, making them more affordable for all Australians and eligible overseas visitors. Around 80 per cent of prescriptions dispensed in Australia are subsidised under the PBS. Under the Repatriation Pharmaceutical Benefits Scheme (RPBS), eligible veterans and war widows and widowers can access some additional medicines and dressings at concession rates and, if clinically justified, items not listed in either the PBS or RPBS schedule. The Department of Health and Ageing develops program policy for the PBS and manages the scheme, including the Schedule of Pharmaceutical Benefits. The Department of Veterans’ Affairs develops policy for the RPBS. Medicare Australia administers the PBS and the RPBS—processing pharmacists’ claims, approving authority prescriptions, approving pharmacists and certain doctors to supply PBS medicine, and approving private hospitals and participating public hospitals to supply PBS medicine to eligible patients. Medicare Australia makes payments under section 100 of the National Health Act 1953 to pharmaceutical companies for supplying in-vitro fertilisation hormones, fertility drugs and botulinum toxin as well as colostomy and ileostomy associations for related surgical supplies. Table 29—PBS expenditure and services 1 2008-09 2009-10 % change PBS benefits paid1 $7.2 billion $7.8 billion +8.3% RPBS benefits paid $475.3 million $485.3 million +2.1% Total benefits paid $7.7 billion $8.3 billion +7.8% PBS services processed1 181.7 million 183.9 million + 1.2% RPBS services processed 14.3 million 13.8 million -3.5% Total services processed 196.0 million 197.7 million +0.9% Including stoma. Medicare Australia also makes payments under the Special Authority Program (a non- PBS program) for the use of trastuzumab (Herceptin®) to treat patients with late stage metastatic breast cancer. In 2009-10 there were approximately 198 million services processed under the PBS and RPBS, representing more than $8.3 billion in benefits. Analysis/trends All PBS benefits paid and services processed have increased by 7.8 per cent and 0.9 per cent respectively. These annual growths are comparable with those of the previous two financial years, which averaged around 8.8 per cent for benefits paid and 3.5 per cent for services processed. PBS ELIGIBILITY The two levels of eligibility for the PBS are the general rate and the concession rate. At the general rate, a person pays a co-payment of up to $33.30 for their prescription medicine and at the concession rate they pay $5.40. These figures are adjusted annually on 1 January, in line with the consumer price index, and do not cover costs for more expensive brands of medicine. To receive subsidised medicine through the PBS, a person must show their current Medicare card each time they get a prescription filled. To receive prescriptions at the concession rate through the PBS or RPBS, a person must show their concession card issued by Centrelink or the Department of Veterans’ Affairs when the medicine is dispensed. This ensures that only eligible people receive subsidised medicine and that they pay the correct amount. PBS SAFETY NET Medicare Australia also administers the PBS Safety Net which is adjusted annually. The Safety Net subsidises people who spend a large amount on prescription medicine in a calendar year. The PBS Safety Net thresholds were adjusted from 1 January 2010. The 2010 general threshold is $1281.30 and the concession threshold (for people holding a concession card from Centrelink or from the Department of Veterans’ Affairs) is $324. After reaching the relevant threshold, a person can apply for a Safety Net card. Once a card is issued: general patients will then pay the concession co-payment rate for their PBS prescriptions concession cardholders will receive their PBS prescriptions for free for the remainder of the calendar year. The patient must pay extra for more expensive brands of medicine. To qualify for the Safety Net, people need to keep a record of all PBS medicines supplied to them or their families. They can either get a prescription record form from their pharmacist to present whenever they have a PBS prescription filled or, if they have a preferred pharmacist, they can ask their pharmacist to keep an electronic record. PBS PROCESSING At 30 June 2010 there were 5402 approved suppliers. This includes community pharmacies, approved doctors and participating public and private hospitals. Community pharmacies make up 94.2 per cent of this total. Table 30—Program deliverables 1 Deliverables and key performance indicators 2009-10 Revised targets 2009-10 Actuals Accuracy of processing >=98% 98.4% Prompt processing 100% 94.8% % of prescriptions claimed online1 - 98.8% Average appropriated expense per billable service1 $0.74 $0.73 Pharmacist satisfaction >=90% 92% Refers to prescription process within 17 days of receipt Analysis/trends In comparison to the previous financial year the accuracy of processing improved by 0.1 per cent. Prompt processing increased by 13.7 per cent during 2009-10. APPROVING SUPPLIERS OF PBS MEDICINE Under sections 90, 92 and 94 of the National Health Act 1953, Medicare Australia can grant approvals to pharmacies, medical practitioners and hospital authorities to supply PBS medicine. An application made under section 90 must be referred to the Australian Community Pharmacy Authority (ACPA) to determine whether it satisfies the requirements of the Pharmacy Location Rules. Analysis/trends The number of section 90 applications increased from 388 in 2008-09 to 436 in 2009-10. 99 per cent of applications were referred to the ACPA seven to nine working days after registration. 100 per cent of applications recommended by the ACPA were advised within three to five working days of the decision and action required. Table 31—Approvals Section 90 applications 2009-10 Applications (new or relocated community pharmacies) referred to the Australian Community Pharmacy Authority (ACPA) 436 281 applications recommended for approval 119 applications not recommended for approval 36 applications withdrawn by the applicant Approvals granted during 2009-10 Section 90 new or relocated community pharmacies 262 Section 90 change of pharmacy ownership 453 Section 92 medical practitioners 14 Section 94 hospitals 14 7 private hospitals 7 public hospitals participating in the pharmaceutical reforms Approved suppliers of PBS medicine as at 30 June 2010 Section 90 community pharmacies 5088 Section 92 approved medical practitioners 53 Section 94 approved hospitals 261 84 private hospitals 177 public hospitals participating in the pharmaceutical reforms 1 Of the 281 applications recommended for approval by the ACPA, 19 applicants were not ready to supply PBS medicine as at 30 June 2010 and therefore were not approved under section 90. AUTHORITY PRESCRIPTIONS Authority medications can only be used for specific conditions and are subject to criteria set by the Pharmaceutical Benefits Advisory Committee. This committee recommends to the Minister for Health and Ageing which medicine should be made available as pharmaceutical benefits. An authority prescription also gives prescribers a mechanism to prescribe an increased supply of PBS/RPBS medicine to treat an individual patient. Table 32—Items listed on the PBS 2009-10 Restricted to use for a particular condition or purpose 1903 Listed as authority required 1092 INDIGENOUS PEOPLE’S ACCESS TO THE PBS Medicare Australia continued to administer the PBS arrangements in remote Indigenous communities, via the Aboriginal and Torres Strait Islander Health Service and some state-funded health services. These arrangements under section 100 of the National Health Act currently make prescription medicine accessible at more than 165 remote area health services across the Northern Territory, Queensland, South Australia, Western Australia and Tasmania. The PBS Co-payment Measure, a key element of the Australian Government’s Indigenous Chronic Disease Package, helps Aboriginal and Torres Strait Islander patients living with chronic disease or at risk of it with the cost of PBS medicine. From 1 July 2010 eligible patients will pay less for each PBS medicine. COMMUNITY PHARMACY AGREEMENT The Community Pharmacy Agreement is an agreement between the Australian Government and the Pharmacy Guild of Australia. The Fourth Community Pharmacy Agreement ran from 1 December 2005 to 30 June 2010. The Fifth Community Pharmacy Agreement started on 1 July 2010. The Community Pharmacy Agreement provides payments to improve the use of medicine and access to community pharmacy services in rural and remote areas. Medicare Australia administers these payments, listed in Table 33. Under the agreement, Medicare Australia made payments totalling $64.1 million in 2009-10. Table 33—Payment types covered by the Fourth Community Pharmacy Agreement Payment type Description Aboriginal Health Services—Pharmacy Support Payment For pharmacy owners to provide services to Aboriginal health services in rural and remote locations in Australia. Home Medicine Review—Rural Loading Payment For pharmacies in rural and remote areas of Australia to assist with travel costs incurred when conducting Home Medicine Reviews. Home Medicine Review For accredited pharmacists to review patients’ medication regimes on the request of the patient, medical practitioner or carer. Online Incentive Payment To support the take-up of online claiming for PBS. Payment type Description Medication Review Accreditation Incentives For pharmacists to achieve and/or maintain accreditation so they can conduct medication reviews. Pharmacy Connectivity Incentive To encourage the use of business grade broadband internet in pharmacies. Quality Care Pharmacy For pharmacists to achieve and maintain Quality Care Pharmacy Program Program accreditation that will enhance professional business practices. Residential Medication Management Reviews For accredited pharmacists to review the medication of eligible patients who are residents of Australian Government-funded aged care homes. Rural Pharmacy Maintenance Allowance To encourage pharmacy owners to remain in designated rural and remote locations in Australia. Software Vendor Assistance payments For software vendors to support the roll-out of PBS Online. Start-up Allowance To encourage the establishment of new pharmacies in designated rural or remote locations. Succession Allowance To assist pharmacists to purchase an existing pharmacy in eligible rural or remote locations. PHARMACEUTICAL REFORMS IN PUBLIC HOSPITALS Under the National Health Care Agreement, the Australian Government, states and territories have reformed the supply of pharmaceutical benefits to eligible patients in public hospitals. Eligible patients include: admitted patients on discharge outpatients day patients accessing chemotherapy drugs. Participating hospitals are required to adopt the Australian Pharmaceutical Advisory Council guidelines on the continuum of pharmaceutical care between the hospital and the community. The pharmaceutical reforms have been widely adopted across the Northern Territory, Queensland, Victoria and Western Australia. The Australian Government will continue to liaise with New South Wales, Tasmania and the Australian Capital Territory about their participation in the reforms. At 30 June 2010 Medicare Australia had approved a total of 107 public hospitals under these arrangements (35 in Queensland, 56 in Victoria, 8 in Western Australia, 7 in South Australia and 1 in the Northern Territory) and paid benefits of more than $205 million. Chapter 4 Delivery of other benefits and services Program 1.3 Case Study Lyndoch Warrnambool—an online success story Staff member Leanne Dalton from the Lyndoch Residential and Community Care in Warrnambool Lyndoch provides residential and community-based care to aged and disabled people across the Barwon South West region. It was established in 1952 and is located in East Warrnambool in South West Victoria. Helen Bacon, Director of Business Services at Lyndoch Warrnambool Inc., has been lodging aged care forms online for the past 12 months. She says the web-based Care Recipient Profile—which was introduced in March 2009 to help aged care services manage their information about the people in their care— has made it even easier. ‘We have been using this all-in-one feature to submit our web forms for admission, departure and leave for our 198 residential bed licences. ‘Our staff members find web forms extremely simple to use—the information is processed quickly and we can fix any processing errors immediately. ‘ Aged Care Online Claiming has made the administration for Lyndoch Warrnambool Inc. much more efficient, including: saving time at the end of the month because resident movements are processed progressively throughout the month no longer having to complete a manual Resident Entry Record, sign it, prepare a cover letter and post it improved accuracy in data and payments, which means spending less time in reconciling payment advices generating statistical reports quickly and easily, and being able to reconcile the claim during less busy times. Staff members who use the Aged Care Online Claiming website summed it up by saying: ‘We would never revert to the old way of doing things. ‘ PERFORMANCE HIGHLIGHTS Medicare Australia processed over 55 000 claims for aged care services in 2009-10. Medicare Australia in partnership with Centrelink, successfully implemented the secure and sustainable pension initiative that contained special arrangements for part pensioners and selffunded retirees who did not benefit from the full pension rise. Medicare Australia has made online claiming more straight-forward for aged care services with 2384 residential aged care services and 230 community aged care services transmitted online in 2009-10. Medicare Australia has worked closely with the National eHealth Transition Authority (NEHTA) to ensure the 1 July 2010 start date of the Healthcare Identifiers Service. Medicare Australia successfully implemented the Small Business Superannuation Clearing House, with employer registrations accepted from May 2010, and the full service becoming operational on 1 July 2010. AGED CARE The Department of Health and Ageing administers policy under the Aged Care Act 1997, while Medicare Australia manages the payment of subsidies and supplements to approved aged care providers. It does this on behalf of the Department of Health and Ageing and the Department of Veterans’ Affairs to help aged care providers deliver cost-effective, quality care for frail, older people and support for their carers. Medicare Australia’s role is to provide timely and accurate payments, with a focus on service and administrative efficiency. Medicare Australia processes and pays: residential aged care subsidies and associated supplements for high level to low level residential care residential respite care subsidies and associated supplements for short-term high level and low level residential care to give carers relief from their caring role Community Aged Care Package subsidies to support people with low level complex health needs and their carers, to enable them to remain at home flexible aged care subsidies, including: extended aged care at home subsidies to support people with high level complex health needs and their carers, to enable them to remain at home extended aged care at home dementia subsidies for dementia-specific support to people with high level complex health needs and their carers, to enable them to remain at home subsidies for short-term rehabilitation care after care in hospital, pending access to longer term care if required. In 2009-10 Medicare Australia processed 33 876 residential claims, 13 654 Community Aged Care Package claims and 7900 flexible care claims. These made up more than $8 billion in aged care benefits. Table 34—Aged care 2008-09 2009-10 % change Number of residential claims processed 33 629 33 876 +0.7% Number of CACP1 claims processed 13 125 13 654 +4.0% EACH2 (including dementia-specific EACH) 5557 6907 +24.3% Transition care 937 993 +6.0% Total flexible care claims processed 6494 7900 +21.7% Flexible care claims: 2008-09 2009-10 % change Total claims processed 53 248 55 430 +4.1% Total amount paid $7.3 billion $8.1 billion +11.0% Number of residential aged care services (aged care homes)3 2791 2782 -0.3% Number of CACP services (facilities providing CACPs) 1092 1147 +5.0% 547 674 +23.2% 2034 2614 +28.5% Number of flexible care services (facilities providing EACH and transition care) Number of active services transmitting (online claiming) 1 CACP = Community Aged Care Package 2 EACH = extend aged care at home 3 Number of residential aged care services decreased in 2009-10 due to consolidation of multiple services on the one site. Analysis/trends Overall the total number of claims processed increased in comparison to last year’s results. There were noticeable increases across the range of flexible care claims, which is consistent with the government providing more care options for older Australians. Medicare Australia’s strong focus on promoting online claiming is shown in the significant upward trend in the number of services now transmitting. Note: Flexible care covers a number of different types of Commonwealth-funded aged care programs. Medicare Australia makes payments to approved providers of Extend Aged Care at Home including dementia-specific Extend Aged Care at Home and Transition Care. Other types of flexible care include Multi-Purposes Services and Consumer Directed Care Packages. Flexible care claims are made by the providers not the care recipients. Aged care online claiming Medicare Australia offers full online claiming for the aged care sector, allowing aged care providers to lodge, view and finalise residential and community care claims online. This streamlines business practices, making them more efficient and producing better outcomes for the aged care sector. Medicare Australia introduced further strategies in 2009-10 to encourage more providers to claim online. The aged care sector is very diverse with different business models, levels of IT capability and needs. The strategies therefore needed to offer choice—that is, both web forms and integrated software products—for aged care residential and community care providers. Using the web form, services can enter selected information for care recipients directly into an online form and submit it electronically via the internet to Medicare Australia, without the need for an integrated software package. Medicare Australia is also working closely with software vendors to assist aged care providers that choose to use integrated software products to come online. The strategy was developed in close consultation with Medicare Australia’s key stakeholders through the Industry Working Group. This group consists of representatives from the peak bodies and organisations associated with the aged care sector and has been established as a forum to raise issues, share information and provide guidance. Medicare Australia has been actively promoting the take-up of online claiming through dedicated Business Development Officers (BDOs), who visit aged care providers to give them relevant promotional material and support. Since the strategy began, online claiming for the aged care sector has risen dramatically. At 30 June 2010, 2653 residential aged care services had registered for online claiming. This represents 95.6 per cent of the total number of residential aged care services. Of these, 2384 aged care services were transmitting online via the online claiming or web form channels. Take-up by community aged care providers also improved in the year with 230 community aged care services commencing online claiming. Electronic Aged Care Client Record project Medicare Australia continued to work closely with the Department of Health and Ageing, participating state Aged Care Assessment Teams and evaluation units on the national rollout of the electronic Aged Care Client Record project. The project gives the Aged Care Assessment Teams the capability to electronically capture and lodge aged care client records information with Medicare Australia for processing within the aged care payment systems. It also allows aged care services to view aged care client records online to verify a client’s approval status. At 30 June 2010 there were 78 Aged Care Assessment Teams from New South Wales, Victoria, Queensland, Western Australia, Tasmania and the Australian Capital Territory electronically transmitting Aged Care Client Records. This is 66.7 per cent of teams nationally. A total of 85 848 electronic records have been received in 2009-10. Medicare Australia will continue to assist the remaining teams to come online. Aged care initiatives During 2009-10 Medicare Australia delivered on a number of key government initiatives for aged care. Medicare Australia implemented process and system changes to support the implementation of these new initiatives as they affected payments, care recipients’ fees and the claiming process. These initiatives were: Secure and sustainable pension —residential aged care To coincide with pension increases the government reset the basic daily fee from 85 per cent to 84 per cent of the single age pension base rate with special arrangements for part pensioners and self-funded retirees who did not benefit from the full pension rise. Aged care viability supplements There have been increases to the viability supplements the government pays to eligible residential aged care providers in regional, rural and remote areas. The viability supplement helps small residential aged care services in rural and remote areas with the extra costs of delivering services in those areas. The amount paid is determined by the location of the service, the number of occupied places, and the proportion of care recipients with special needs. Fairer income testing in residential aged care—ending the 28-day income test exemption Residents who have the means to pay an income-tested fee will be asked to pay this fee from the first day that they receive care in a government-subsidised residential aged care facility. Before the change, people were exempt from paying income tested fees for the first 28 days (inclusive of pre-entry leave). Changes to the Aged Care Funding Instrument high care definition The introduction of the Aged Care Funding Instrument (ACFI) has unintentionally classified some residents as high care when they are not. This is being rectified so that only people needing a higher level of care are assessed as such. 2-year variation limit If providers want to amend a claim for payment two years after the original claim they must provide Medicare Australia with appropriate supporting documentation. HEALTHCARE IDENTIFIERS SERVICE The modern healthcare environment demands greater sharing of health information so that quality health care can be provided seamlessly and efficiently. In February 2006 the National eHealth Transition Authority (NEHTA) obtained funding from the Council of Australian Governments for the Healthcare Identifiers (HI) Service. Funding was provided on the basis that in developing the service it would leverage Medicare Australia’s infrastructure, systems, data, policies and reputation. The HI Service will provide unique healthcare identifiers to all individuals, healthcare providers and healthcare provider organisations. The service and the subsequent use of healthcare identifiers by healthcare professionals are the first essential steps in developing a National eHealth System. Under contract to NEHTA, work to design, build and test the HI Service began in January 2008. By December 2009 Medicare Australia had delivered Release 1 of the HI Service through the ‘Model Healthcare Community’, an exhibition hosted by NEHTA and Medicare Australia in the atrium at the Medicare Australia National Office. The exhibition showed how the service could operate and support eHealth services in the community in the future, and the systems and processes built by Medicare Australia for the first system release. More than 600 people including ministers, agency and department heads, representatives from other jurisdictions and health professionals visited the exhibition. The new Model Healthcare Community is now located in Victoria and hosted by the Royal Australian College of General Practitioners. Medicare Australia’s Melbourne-based Business Development Officers continue to provide support to this exhibition. HOME INSULATION PROGRAM The Home Insulation Program and Low Emission Assistance Plan for Renters were set up as part of the Energy Efficient Homes Package to improve energy efficiency of Australian homes and stimulate the economy. In June 2009 Medicare Australia entered into a service arrangement with the Department of Environment, Water, Heritage and the Arts (DEWHA) to provide online registration, claims and payment services to eligible companies and installers for the installation of roofing insulation in Australian homes under the two programs. Registration for installers began in June 2009 with access to the rebate program from 1 July 2009. Under the service agreement DEWHA administered the scheme and was responsible for policy, approvals and compliance. Medicare Australia’s role was to: manage online registrations, claims and payments for registered installers establish a dedicated phone line for enquiries from installers relating to the use of the online registration, claims processing and payments make payments in accordance with the business rules and approvals provided by DEWHA. The program was discontinued on 19 February 2010, however, installers were entitled to be paid for installations made before that date. Medicare Australia made the payments progressively as the Department of Climate Change and Energy Efficiency approved individual claims. Table 35—Home Insulation Program 2009-10 Number of registered installers under the program 7386 Number of claims paid to installers by Medicare Australia 1 133 876 Value of rebate payments made to installers by Medicare Australia $1.6 billion SMALL BUSINESS SUPERANNUATION CLEARING HOUSE In the 2008-09 Federal Budget the government announced it would implement a Superannuation Clearing House facility. The Superannuation Clearing House will reduce administrative effort and compliance costs that small businesses experience in meeting their superannuation obligations. It allows employers to make one payment to the Superannuation Clearing House, which then distributes the funds to superannuation funds registered by the employer. Government funding of $16.1 million was granted over three years for the clearing house beginning in 2009-10. Use of the Superannuation Clearing House service is optional and free of charge to small businesses with less than 20 employees. The Superannuation Clearing House began taking registrations on 24 May 2010 and was fully operational on 1 July 2010. ADDITIONAL GOVERNMENT SERVICES DELIVERED THROUGH MEDICARE OFFICES Medicare offices continue to provide an important role for an increasing number of Australian Government programs, including Family Assistance, citizenship testing services and the LPG (liquid petroleum gas) Vehicle Scheme. Family Assistance services are available in all Medicare offices and flexible service delivery branches across Australia. Department of Immigration and Citizenship officers administer citizenship tests at selected Medicare offices in regional Australia. Medicare Australia also receives claims and provides information on the LPG Vehicle Scheme. Seventyfour per cent of all grant applications in 2009-10 were lodged with Medicare Australia. Family Assistance Medicare Australia provides Family Assistance services through the Medicare branch office network on behalf of the Department of Families, Housing, Community Services and Indigenous Affairs, and the Department of Education, Employment and Workplace Relations. The Family Assistance Office was established to make it easier for families to obtain family- related benefits. Instead of going to different agencies to get various family benefits, they can get them from one place—the Family Assistance Office (FAO). All Medicare offices around Australia are Family Assistance Offices. Members of the public can lodge their Family Assistance claims, income estimates, method of payment and contact details, and also obtain advice and information about Family Assistance benefits from their local Medicare office. Medicare Australia’s functions include: delivering services as part of the Family Assistance Office (under the provisions of the A New Tax System (Family Assistance) Act 1999 and A New Tax System (Family Assistance) (Administration) Act 1999 and undertaken through service arrangements with Australian Government agencies, in accordance with section 7 of the Medicare Australia Act 1973). Family Assistance payments include: Family Tax Benefit Part A, which provides help with the cost of raising children Family Tax Benefit Part B, which provides extra help for families with one main income, including sole parents Child Care Benefit, which offsets the cost of long and part-day child care Child Care Rebate, which provides additional help with the cost of child care Baby Bonus, which helps with the costs of caring for a new baby Maternity Immunisation Allowance, which is a separate payment for children who have been fully immunised. Table 36—Family Assistance Services 2009-10 Number of FAO inquiries 345 769 Number of FAO claims granted 187 633 Note: Services provided by Medicare Australia Decision-making powers A New Tax System (Family Assistance) Act 1999 A New Tax System (Family Assistance) (Administration) Act 1999 Citizenship testing The Citizenship testing scheme requires most applicants to successfully complete a test before applying for Australian citizenship. Medicare Australia and Centrelink in regional and rural areas conduct citizenship testing, providing easier access, improved customer service and to assist in cost efficiencies. Citizenship testing is administered by the Department of Immigration and Citizenship staff at 30 Medicare offices. LPG Vehicle Scheme The LPG (liquefied petroleum gas) Vehicle Scheme was established in October 2006 to help private motorists buy a new LPG vehicle or convert a new or used petrol or diesel vehicle to LPG. The Department of Innovation, Industry, Science and Research administers the scheme with Medicare Australia and Centrelink being the public contact points for enquiries and applications for grants. Centrelink is responsible for paying approved grants. During 2009-10 Medicare Australia received more than 32 000 applications, representing 74 per cent of the total applications received under the scheme. The Department of Innovation, Industry, Science and Research advised that the decline in program demand was most likely due to lower stable petrol prices, and the impact of the global financial crisis. Table 37—LPG Vehicle Scheme 1 2008-09 2009-10 % change Number of applications received by Medicare Australia 64 2821 32 162 -50.0% Percentage of total applications received +75.6%’ +74.0% -1.6% This information includes an average for two months, as only 10 months of information is available. Chapter 5 Medicare rebates —electronic claiming Program 1.4 Case Study Electronic claiming is the way to go Some of the members of the Medicare electronic claiming team In the past few years electronic Medicare claiming has revolutionised how Medicare does its business. So much so that today more than 79 per cent of all claims are submitted electronically. A team leader, Kaveri Chakrabarty, in the eClaiming and eHealth Branch, explained the system. ‘There are three channels available for electronic Medicare claiming: Medicare Online, Medicare Easyclaim and ECLIPSE. Medicare Online is where in and out-of-hospital claims are submitted over the internet from a doctor’s practice for payment of a Medicare benefit. Medicare Easyclaim uses the EFTPOS facility in a doctor’s practice to submit out- of-hospital claims for payment of a Medicare benefit. ECLIPSE is where in-hospital claims are submitted over the internet. The claim may also be sent to the private health fund or Department of Veterans’ Affairs for processing of either the private health fund or Department of Veterans’ Affairs benefit, ‘ she said. The take-up of electronic Medicare claiming has been increasing in recent years because of the concerted effort Medicare Australia has put into educating doctors and patients about the benefits. The government has also provided financial incentives for healthcare providers and software vendors that create and use the products through which claims are made. ‘The benefits are huge, ‘ Kaveri said, ‘particularly for the elderly and parents with young children, who do not have to fill in and post forms or go to a Medicare office. ‘After claiming electronically, they can receive their benefit directly into their bank account or by cheque if they prefer (for Medicare Online and ECLIPSE). ‘ Medicare Australia has been strongly promoting the direct payment option as the preferred method by offering a number of ways for members of the public to provide/ register their bank account details with Medicare Australia. As well as patients being able to claim benefits electronically, doctors too are able to lodge their bulkbilled claims electronically, making the process simpler with faster payments into their bank account. ‘The administrative overhead is much less for everyone’. PERFORMANCE HIGHLIGHTS At 30 June 2010 all 36 health funds were using the ECLIPSE electronic system for in-patient hospital claims. Medicare developed and rolled out a campaign to raise awareness among practitioners and the public about electronic Medicare claiming. The collection of patients’ bank account details for easy electronic payment increased to more than three million consumers. The Transitional Support Package helped GPs and specialists, as well as software vendors, with start-up costs for electronic claiming. A subsidy to develop systems that integrate Medicare Easyclaim was available to software developers. The combined take-up of both Medicare Online and Medicare Easyclaim increased by 6.5 per cent from June 2009 to June 2010. Electronic Medicare claiming makes bulk bill claiming much more convenient for medical practices, as well as allowing patients to claim their Medicare rebate at the practice. This is done through three electronic claiming channels: Medicare Online Medicare Easyclaim Electronic Claim Lodgement Information Processing Service Environment (ECLIPSE). Over 90 per cent of bulk bill services are submitted electronically, i.e. via Medicare Online and Medicare Easyclaim. These claiming channels are explained further on. This chapter in part reports against program 1.4—Medicare rebates—electronic claiming. For information about Medicare rebates see Chapter 2: Delivery of medical benefits and services. MEDICARE ONLINE Introduced in 2002, Medicare Online is an internet-based claiming channel that is integrated into providers’ practice management software. Using Medicare Online, providers can make claims such as in and out-of-hospital, bulk-bill and patient claims, as well as claims for Department of Veterans’ Affairs services and the Australian Childhood Immunisation Register. Most healthcare practitioners, including eligible health professionals and dentists, can use Medicare Online. Offered over secure connection using Public Key Infrastructure, Medicare Online enjoys strong support from provider communities. In 2009-10 more than 11 000 practices used Medicare Online. Payments for patient claims are made directly into their bank account if account details have been recorded. MEDICARE EASYCLAIM Medicare Easyclaim, a more recent channel than Medicare Online, enables medical practices to lodge claims with Medicare Australia. Medicare Easyclaim differs from Medicare Online as it uses a secure Electronic Funds Transfer Point of Sale (EFTPOS) network operated by financial institutions specifically accredited by Medicare Australia. For payment of the Medicare benefit for fully paid patient claims, the claimant simply swipes their bank debit card and receives their benefit almost immediately into their bank account. Medicare Easyclaim was introduced in 2007 as a standalone facility separate to practice management software. However, recent developments have resulted in Medicare Easyclaim solutions now offering an option that integrates the practice management software with the EFTPOS terminal. Medicare Easyclaim can transmit out-of hospital bulk bill and patient claims, but unlike Medicare Online does not facilitate Department of Veterans’ Affairs claiming, reporting for the Australian Childhood Immunisation Register, or support some of the more complex Medicare item numbers. A practice can use either or both Medicare Online and Medicare Easyclaim. ECLIPSE The Electronic Claim Lodgement and Information Processing Service Environment (ECLIPSE) is an electronic system that can be used for in-patient hospital claims. ECLIPSE is an extension of Medicare Online and provides a secure connection using Public Key Infrastructure between practices, public and private hospitals, billing agents, Medicare, private health funds and the Department of Veterans’ Affairs. Benefits for users of ECLIPSE include fewer claim rejections, better quality of data, reduced administrative effort, and faster claims processing and payment. Out of a total 37 health funds, 36 were using ECLIPSE at 30 June 2010. ECLIPSE also facilitates informed financial consent for private patients seeking an estimate for hospital treatment by providing their out-of-pocket costs. ECLIPSE claims fall into two broad categories: in-hospital medical claims in-hospital claims. In-hospital medical claims are for medical items arising from an in-hospital episode of care and benefits may be payable by Medicare Australia as well as the patient’s private health fund. An in-hospital claim involves non-medical aspects of a patient’s hospital stay—such as accommodation, theatre, transfers, prosthetics—where benefits may only be payable by a private health fund or the Department of Veterans’ Affairs. ECLIPSE was developed in collaboration with the broader health sector, and improves public-private coordination in the delivery of healthcare services. TAKE-UP AND USAGE OF ELECTRONIC MEDICARE CLAIMING Medicare Australia has been working with medical providers, software vendors and members of the public to increase the availability and adoption of electronic Medicare claiming. Specifically, Medicare Australia has implemented a series of targeted promotional activities to practitioners and the public to raise awareness and understanding of electronic Medicare claiming. This year, the focus has been on electronic patient claiming and how easy it is for patients to now claim their Medicare benefits. More recently, information about ECLIPSE has been included in some of these activities. Medicare has used a range of strategies to increase the collection of patients’ bank account details so that electronic payments can be easily made. Bank account details are recorded for more than three million consumers. FINANCIAL SUPPORT Financial support was given to medical practices and software vendors to assist with the introduction of electronic Medicare claiming through the Transitional Support Package, which ceased at 31 December 2009. General practitioners and specialists (excluding pathologists) who began using electronic claiming between 1 September 2007 and 31 December 2009 were eligible for a one-off lump sum payment of $750 (for metropolitan areas) or $1000 (for rural and remote areas) for start-up costs. At 30 June 2010 more than 1200 general practitioner and specialist practices received their one-off lump sum payment. Practices and providers also received an incentive payment of 18 cents for each electronic bulk bill and patient claim transaction successfully assessed by Medicare Australia between 1 September 2007 and 31 December 2009. These payments were made quarterly to about 5000 practices and 25 000 providers. Software vendors were also eligible for incentive payments within the Transitional Support Package. These payments, which recognised that vendors play an important role in assisting practices to move to electronic claiming, had two components: a roll-out payment and a support payment. Software vendors may have been eligible to receive the roll-out payment for any general practice or specialist site using their software which started using Medicare Online claiming between 1 September 2007 and 31 December 2009. The roll-out payments varied from $750 to $2250 depending on the site’s claiming channel. Software vendors may have been eligible for a support payment between February 2009 and January 2010. Each support payment was 25 per cent of the total amount of the roll-out payment already paid. At 30 June 2010 more than 50 software vendors had received roll-out payments for more than 1790 sites. In addition, the Medicare Easyclaim Practice Management System Integration Solution Subsidy funded the development of practice management systems that integrate Medicare Easyclaim. Figure 7—Milestones in take-up initiative of electronic patient claiming Figure 8—Medicare service by claim type—electronic and manual Figure 9—Number of practices transmitting electronically Table 38—Volumes of services transmitted electronically 2007-08 2008-09 2009-10 bulk bill 80.3 million 181.8 million 198.0 million patient claim 5.7 million 8.2 million 11.7 million bulk bill 786 483 4.7 million 11.2 million patient claim 346 424 1.3 million 3.7 million ECLIPSE 464 439 1.2 million 3.0 million Total 87.6 million 197.2 million 227.6 million Medicare Online Medicare Easyclaim Note: Extrapolated to 12 months from July 2009-June 2010 data. Through the subsidy, a total of $6 million was available to software developers to design, develop and roll out solutions that support the integration of practice management software with Medicare Easyclaim solutions. The benefits of the subsidy, which was paid in June 2009, have started to be felt in the past year. Figure 7 shows the key milestones in the take-up initiative of electronic patient claiming. There has been a major increase in the use and take-up of electronic Medicare claiming channels. As shown in Figure 8, of all Medicare claims 79 per cent were made electronically in 2009-10. As shown in Figure 9, the number of practices using Medicare Online increased from 8453* in 2007-08 to 11 244 in 2009-10. Medicare Easyclaim grew even more—from 1 578* to 6830 over the same period. * The methodology of calculating the number of transmitting sites has changed to be consistent across all channels. Figure 10—Examples of growth in monthly volumes claimed electronically Analysis/trends As shown in Table 38, the volume of services transmitted electronically substantially increased. Although claims transmitted through Medicare Easyclaim more than doubled this year, most services are transmitted through Medicare Online. Electronic patient claiming at general practitioners’ surgeries has been a significant contributor to the increase. At June 2010, 47.5 per cent of all patient claims at GPs’ surgeries are now made electronically. Specialists have been slower to adopt this, making only 15.1 per cent of patient claims electronically. Further to the above profile on annual growths, Figure 10 below shows examples of growth in monthly traffic for Medicare Easyclaim bulk bill and patient claims, and ECLIPSE claims, over the past two years. Further information Further details on the electronic Medicare claiming channels and related processes are published on Medicare Australia’s website: www.medicareaustralia.gov.au. Chapter 6 Customer service and partnerships Case Study What are customers telling us? ‘So in the future we will be holding more forums and doing more research so we can better understand what our customers are seeking and ask them to help shape our services.’ Early in 2010 the Human Services portfolio conducted a series of forums with customers to explore their experiences and views of government service delivery. About 20 forums were held across Australia, with up to 20 people being invited to each one. The ideas they rated as most important included: personalised service delivery linked-up services help with everyday issues easy and appropriate access options. Mary, who was involved in running the forums, said the people attending were positive about the idea of agencies sharing their information, with one customer noting: ‘It would be good if they could work together. They don’t share information and we really want each provider to have access to as much of our information as possible so there’s no duplication. We could do things once and have it over and done with. ‘ Mary said from the portfolio’s point of view the forums provided some really useful information. ‘We discovered which groups we needed to contact for more feedback—for example, families caring for a family member with a disability and older people not accessing Centrelink payments. ‘So in the future we will be holding more forums and doing more research so we can better understand what our customers are seeking and ask them to help shape our services. ‘ PERFORMANCE HIGHLIGHTS Medicare Australia is developing ‘co-design practice’ as part of service delivery reform within the Human Services portfolio to ensure real community partnerships are built to shape and deliver better services. Several international organisations visited Medicare Australia, including the World Health Organisation, the Chinese Ministry of Health and the Japan Federation of National Health Insurance Organisations. More than 1000 new registrations every day for Medicare Australia’s online services. A range of new services were added to the Health Professional Online Services, including staff logon, and the ability to view a patient’s care plan history, with their consent. A new intranet began, with more tools and information for the benefit of staff and stakeholders. A new program began, giving an incentive to general practices to provide better care of Indigenous patients with chronic disease. A new PBS measure ensures that medicine are more affordable for Indigenous patients with chronic disease. CO-DESIGN PRACTICE As part of service delivery reform within the Human Services portfolio, Medicare Australia is leading the development and implementation of ‘co-design’. Co-design refers to the methods used to involve the community, staff and stakeholders to shape the reform activities. A people-first focus is paramount to ensure that community needs are identified and met in the reform. Internationally, the practice of co-design is being recognised as a way of improving government services. A co-design capability is being established to enable this to happen as part of Australia’s service delivery reform agenda. Co-design is more than asking for feedback or undertaking consultation or satisfaction surveys. It means engaging with individuals and groups from the beginning to the end of a design process. The co-design approach will ensure: genuine partnerships are built with the community the community has a real and ongoing voice at the table change delivers a balance of what the Australian Government, the Human Services portfolio and the community want to achieve the end user is involved in the planning, development and implementation of solutions outputs are user friendly and meet the end user’s needs change and new products integrate smoothly with existing systems. MEDICARE AUSTRALIA’S RELATIONSHIP WITH GOVERNMENT Medicare Australia’s strong partnership with government departments and agencies helps us deliver efficient and convenient services to all Australians on behalf of the Australian Government. In 2009-10 Medicare Australia delivered services on behalf of: the Department of Health and Ageing (DoHA) the Department of Veterans’ Affairs (DVA) the Department of Families, Housing, Community Services and Indigenous Affairs (FaHCSIA) the Department of Innovation, Industry, Science and Research (DIISR) the Department of Environment, Water, Heritage and the Arts (DEWHA) the Department of Climate Change and Energy Efficiency the Treasury. MEDICARE AUSTRALIA’S STAKEHOLDERS Effective collaboration and consultation with key stakeholders is integral to ensure that Medicare Australia’s programs provide efficient and convenient service delivery. Medicare Australia’s Stakeholder Engagement Strategy provides the framework and direction for how groups or individuals in the organisation engage with external stakeholders. It ensures benefits are maximised in engagement with stakeholders. Many individual areas within Medicare Australia recognise the value of stakeholder engagement and actively seek opportunities to engage with key stakeholders in a collaborative manner. To achieve desired outcomes from stakeholder engagement, Medicare Australia developed and implemented a twoyear Stakeholder Engagement Strategy in 2009. This provides a clear strategic direction for stakeholder engagement and articulates the organisation’s principles and approach to stakeholder engagement. STAKEHOLDER CONSULTATION Medicare Australia undertakes formal and informal stakeholder engagements and forums as part of its business processes nationally and at state level. Its peak stakeholder consultation forums are the Stakeholder Consultative Group (SCG) and the Consumer Consultative Group (CCG). Members of these groups include representatives of peak bodies and organisations that are affected by the programs Medicare Australia administers. Medicare Australia has clear and agreed governance for how to engage with key stakeholder groups to obtain their feedback about the delivery of quality information and services. Stakeholder Consultative Group Through the Stakeholder Consultative Group key groups in the health sector engage with Medicare Australia on its business priorities and programs at a strategic level. The group meets three times a year and provides a valuable opportunity to build collaborative working relationships. This group is not a decision-making forum but plays an important role in identifying potential issues and opportunities so that the best results can be achieved for stakeholders. It comprises representatives from peak bodies and other government departments: Australian Association of Practice Managers Aged Care Association of Australia Australian General Practice Network Australian Health Insurance Association Australian Medical Association Australian Pharmacy Council Australian Private Hospitals Association Committee of Presidents of Medical Colleges Consumers’ Health Forum of Australia Medical Software Industry Association Pharmaceutical Society of Australia Rural Doctors Association of Australia Royal Australian College of General Practitioners Society of Hospital Pharmacists of Australia The Pharmacy Guild of Australia Department of Health and Ageing Department of Veterans’ Affairs. Consumer Consultative Group Medicare Australia has an established consumer stakeholder group, the Consumer Consultative Group, which meets three times a year. Members provide input on issues which impact our customers, discuss their potential effect on services and products, and advise Medicare Australia on how to add further value in delivering services to the Australian public. This committee consists of representatives from agency departments and consumer groups: Australian Federation of Disability Organisation Carers Australia Chronic Illness Alliance Consumers’ Health Forum of Australia Council on the Ageing (COTA) National Seniors Families Australia Federation of Ethnic Communities Councils of Australia Health Consumers Rural and Remote Australia Health Issues Centre Winnunga Nimmityjah Aboriginal Health Department of Health and Ageing. Table 39—Overall stakeholder satisfaction levels 2006-07 to 2009-10 2006-07 2007-08 2008-09 2009-10 Public 90% 89% 93% 96% Practitioners 89% 86% 74% 85% Practice managers 95% 89% 87% 91% Pharmacists 87% 91% 86% 92% Aged care providers 96% 92% 95% 94% Figure 11—Stakeholder satisfaction 2002-03 to 2009-10 Satisfaction research findings Medicare Australia has undertaken annual satisfaction research with the community since 1984 and with medical professionals since 1991. The results and recommendations of these surveys provide Medicare Australia with a better understanding of the needs and expectations of providers and the Australian public. Colmar Brunton conducted the annual satisfaction research on behalf of Medicare Australia. The research findings feed into strategic planning processes to ensure continued development of Medicare Australia services. In 2009-10 research was conducted with the Australian public, practitioners (general practitioners, pathologists, imaging and other specialists, optometrists, dental practitioners, Aboriginal health service providers and other allied health providers), practice managers, pharmacists and aged care providers. Medicare Australia has developed a research framework to ensure it gains full benefit from its research expenditure. A three-year research contract was established with Colmar Brunton in 2009 to maintain continuity in the annual public and provider satisfaction research. The research results guide Medicare Australia’s business planning activities and identify any issues for future research to enhance its service delivery to providers and the public. It includes measuring satisfaction with any changes in customer service delivery resulting from the portfolio’s service delivery reform program. CUSTOMER SERVICE CHARTER Medicare Australia has a commitment to improve service delivery to the Australian community and stakeholders. Our Service Charter is a public expression of our commitment to excellence in service delivery. It tells our customers: what standard of service we will provide their rights as a customer their responsibilities as a customer what they can do if they are unhappy with the service they receive. Medicare Australia’s Service Charter is available as a brochure in Medicare offices and electronically at: www.medicareaustralia.gov.au. Information on Medicare Australia’s performance against the delivery of these measures is published quarterly. Commonwealth Ombudsman During the year, the Commonwealth Ombudsman received 171 approaches about Medicare Australia, covering 173 separate issues. Of the approaches finalised, 36 of these (21 per cent) covering 38 issues were forwarded to Medicare Australia to provide background information to assist with their investigations. Medicare Australia responded to all of these approaches. In four of them, the Commonwealth Ombudsman made a finding of administrative deficiency. In accordance with Medicare Australia’s commitment to continuous improvement, all complaints are reviewed to identify systemic issues, and establish appropriate business improvement strategies. The 171 approaches represented a 6.2 per cent increase on the 161 approaches made in the previous year. BUILDING INTERNATIONAL RELATIONSHIPS Medicare Australia continued to build and maintain relationships with other countries to exchange information on policy development, service delivery and compliance systems. This helps Medicare Australia administer the Medicare and Pharmaceutical Benefits schemes. For information about international visits to Medicare Australia, see Table 40. Table 40—International visits to Medicare Australia Date Delegation Areas of interest August 2009 World Health Organisation Parramatta NSW Overview of Medicare program October 2009 Israeli Ministry of Health Canberra Overview of Medicare program November 2009 Japanese Federation of National Health Insurance Organisations Parramatta NSW—Overview of Medicare program November 2009 Japanese Mutual Aide association of public school teachers Parramatta NSW—Overview of Medicare program November 2009 National Health Insurance Department of Health—Taiwan Canberra Medicare, PBS, Fraud and Compliance framework Date Delegation Areas of interest November 2009 Chinese Ministry of Health Canberra Medicare program November 2009 Vietnamese Ministry for Health Canberra Overview of PBS, Australian Organ Donor Register, Australian Childhood Immunisation Register November 2009 Vietnamese Ministry for Health Brisbane Overview of Medicare program and operations December 2009 Ministry of Health Kazakhstan Canberra Overview of Medicare policy, program and operations January 2010 Vietnamese Ministry for Health Parramatta NSW Overview of Medicare policy, program and operations February 2010 Control Yuan of the Republic of China Canberra Overview of Medicare policy, program and operations March 2010 April 2010 May 2010 May 2010 49th Parliament Health Select Committee, New Zealand Canberra First Affiliated Hospital of Anhui Medical university Perth Mutual Aid Association of Prefectural Government Sydney The university of Queensland and The Human Resources and Social Security Bureau of Dalian City Government Brisbane Overview of Medicare program and operations, Australian Childhood Immunisation Register Overview of Medicare program and operations Overview of Medicare policy, program and operations Overview of Medicare program and operations ACCESS AND EQUITY During 2009-10 Medicare Australia continued to respond to the Commonwealth Disability Strategy with a range of activities guided by the principles of equity, inclusion, participation, access and accountability. Information kits about its programs are available in braille, large print and audio formats on request from Medicare offices and Medicare Australia contact centres. Large print information is also available from the Medicare Australia website. Medicare Australia provides access to the Telephone Typewriter Service and the National Relay Service for people with hearing or speech impairments. Assisted listening devices are available in selected Medicare offices to provide better access to services for people with hearing disabilities. The provision of adequate physical access to Medicare offices is a mandatory component of all lease negotiations and will remain the case through the roll-out of co-located Medicare offices as part of service delivery reform. Medicare offices are subject to a continual improvement program relative to fitout design and occupational health and safety. Recent initiatives include the installation of automatic doors, sit-down service counters and writing slopes. Seated waiting areas and electronic queue ticket systems in Medicare Australia’s busiest offices make arrangements efficient and comfortable for the public. Cultural diversity Australia has people from more than 180 countries who speak some 200 different languages. Medicare Australia is always looking at ways to make it easier for people from culturally and linguistically diverse backgrounds to access information about the services and programs it delivers. Medicare Australia has an information kit available in 19 community languages. The information kits are available from the Medicare Australia website and all Medicare offices. In addition, the kits are promoted to migrant resource centres as an important resource for people arriving in Australia. Medicare Australia includes a contact number for the Translating and Interpreting Service (TIS), provided by the Department of Immigration and Citizenship, on all communication brochures. The public can contact TIS to speak to a qualified interpreter in more than 170 languages, either by phone or at a face-to-face interview if required. Medicare Australia also has a number of bilingual employees who use their language skills to make communication with the Australian public easier and more effective. ONLINE SERVICES Online services provides an additional channel for the Australian public to securely view, update and request some information held by Medicare Australia. More than 1.5 million Australians have registered for Medicare Australia’s online services, with an average of more than 1000 new registrations every day. The most popular services accessed through online services are the: Medicare claims history statement Medicare benefit tax statement Australian Childhood Immunisation Register history statement Medicare Safety Net balance. Pre-filling of tax returns From July 2006 taxpayers have been able to retrieve their Medicare benefit tax statement automatically through the e-tax lodgment process. For those who lodge their personal tax return electronically and complete the medical expenses section of the return, this service removed the need to phone or visit a Medicare office to request a Medicare benefit tax statement. Tax payers have also been given more choice in the entry of Medicare Australia information in their tax returns. The delivery of the Medicare benefit tax statement has been expanded to allow tax agents to retrieve the information on behalf of their clients. The expansion of this service was made possible through close collaboration between Medicare Australia and the Australian Taxation Office. From 1 July 2009 to 30 June 2010, 1 320 172 million customers have pre-filled their Medicare claims data into the Australian Tax Office e-tax application and 101 258 customers have pre-filled their Medicare claims data via the Tax Agent Portal. Health Professional Online Services Health Professional Online Services (HPOS) offer better access for health professionals to Medicare Australia’s online services through a single entry point. Since it began in March 2009 there have been more than 600 000 logons to HPOS and more than 870 000 services have been accessed it, the most popular being patient verification, which accounts for 67 per cent of services accessed. The following key services were added to HPOS in 2009-10: a staff logon which allows nominated practice staff to access HPOS on behalf of a health professional using their own authentication certificate the ability for health professionals to view a patient’s care plan history with consent of the patient the ability to reopen a Medicare practice location the ability to manage existing bank account details expansion of the email subscription to allow health professionals to subscribe to: National Bowel Cancer Screening Program Australian Childhood Immunisation Register Australian Defence Force Family Healthcare Program 90 day Pay Doctor Via Cheque statements the ability for insurance companies to submit claims, register midwives and change midwives’ details. Web services About 7.7 million visits were made to Medicare Australia’s website in 2009-10. Of around 21 000 visits per day to Medicare Australia web pages, an average of 3971 were made to the online services index page, and 9749 to the Medicare Australia homepage. Medicare Australia began a new intranet in 2009-10. The intranet is now an intuitive resource of tools and information, which enables our people to access quality advice, guidance, communication and services. Staff and stakeholders were widely consulted, resulting in new information architecture, a refreshed design and a full review of content. The new intranet has cut costs for Medicare Australia through less content having to be maintained, better user experience and improved quality of information. INDIGENOUS AUSTRALIANS Stakeholder engagement Medicare Australia works with other agencies in the Human Services portfolio and wider government, including Centrelink, the Child Support Program, the Department of Veterans’ Affairs, the Department of Families, Housing, Community Services and Indigenous Affairs, and the Department of Health and Ageing, particularly with the Office of Aboriginal and Torres Strait Islander Health. Initiatives include: shared field trips to Indigenous communities with the Department of Human Services and other agencies. Field trips increase the breadth of community access and foster strong networking between agencies and communities ongoing promotion of the Voluntary Indigenous Identifier, which encourages all Indigenous Australians to identify as Indigenous. The identifier is part of a broader government initiative that provides valuable information for planning, policy development and service improvements. Indigenous Access Strategy The Indigenous Access Strategy was developed in response to major studies that recommended how Medicare Australia could contribute to improving the health of Indigenous Australians. Research on average revealed that despite their poorer levels of health, Indigenous Australians on average accessed the Medical Benefits Scheme and the Pharmaceutical Benefits Scheme less than other Australians. The major focus of the Indigenous Access Strategy is to ensure that Indigenous Australians register for Medicare, as well as voluntarily identifying themselves to Medicare Australia as Indigenous Australians. The number of people who have voluntarily identified themselves as Indigenous Australians continues to grow steadily. The number of Indigenous-specific services claimed through Medicare has also steadily increased. Medicare Australia is implementing the Council of Australian Governments’ Closing the Gap measures. In particular, Medicare Australia has been involved in two new measures: the Practice Incentives Program Indigenous Health Incentive, which gives an incentive to general practices to provide better care of Indigenous patients over the age of 15 with chronic disease the PBS measure, which ensures that medicines are more affordable for Indigenous patients with chronic disease, or at risk of it. Medicare Liaison Officers for Indigenous Access (MLOs) work closely with Aboriginal and Torres Strait Islander medical and other health service providers to promote and support the use of Medicare Australia programs. The MLOs operate in each state and territory and have culturally appropriate skills and expertise. MLOs provide dedicated support and outreach services to Indigenous people and communities, undertaking field trips and visits to health services, local communities, prison, schools and relevant stakeholders. They: provide support and training for Aboriginal and Torres Strait Islander health service staff to ensure correct Medicare benefits are claimed, resulting in increased Medicare revenue for health services promote the importance of increasing enrolments and access to Medicare Australia services provide support and expert advice to health service staff and providers about new Medicare initiatives represent and promote Medicare Australia programs and services at local Indigenous forums and events provide support and advice through the dedicated Aboriginal and Torres Strait Islander Access and Employment line on 1800 556 955. Monthly reports help identify health service needs and direct resources. This ensures that Medicare Australia continues to develop its policies and practices and the services it offers to Indigenous Australians based on areas of need and in a culturally appropriate manner. Reconciliation Action Plan Medicare Australia has a Reconciliation Action Plan which commits it to deliver on key initiatives set out by Reconciliation Australia. A Statement of Commitment to Reconciliation, the Indigenous Access Strategy and the Indigenous Employment and Retention Strategy underpin the Reconciliation Action Plan. Chapter 7 Management and accountability Case Study Better distribution of your medicine The Prescription Shopping Information Service is available on 1800 631 181 The Prescription Shopping Program is an information service to help doctors make informed prescribing decisions about patients, and to inform patients who have been identified under the program. There are two elements to the Prescription Shopping Program: a Prescription Shopping Information Service (PSIS): 1800 631 181—available 24 hours, 7 days a week to doctors who are registered with the service a patient and provider alert service conducted by Medicare Australia. Medicare Australia administers the program on behalf of the Australian Government within strict privacy and legal constraints. These constraints are important because obtaining high levels of medicine subsidised under the Pharmaceutical Benefits Scheme may be medically necessary for many people, for example, people with a chronic illness. Doctors can ring the Prescription Shopping Information Service if they suspect a patient is getting more medicine than they need. Or Medicare Australia can contact the prescriber if their patient has been identified under the program. Between February and April last year, the top 10 people identified through the Prescription Shopping Program each saw more than 17 doctors, and each received more than 61 Pharmaceutical Benefits Scheme medicines. In New South Wales, one patient alone saw 40 doctors and obtained 118 Pharmaceutical Benefits Scheme medicines. PERFORMANCE HIGHLIGHTS The Travelling with PBS medicine enquiry line and website received a total of 4147 calls and 30 930 hits. Medicare Australia completed 3594 cases during 2009-10. More than $10.2 million was identified for recovery from compliance activities undertaken during 2009-10. Payment accuracy reviews revealed the level of payment accuracy for Medicare rebates was 99.86 per cent and for the Pharmaceutical Benefits Scheme was 99.7 per cent. This compares with 99.53 per cent and 99.79 per cent in 2008-09. Medicare Australia is accountable for its actions within the framework of ministerial responsibility to the government, the parliament and the Australian public under section 10(1)(e) of the Public Service Act 1999. The Minister for Human Services has chosen not to continue with the Statement of Expectations and Statement of Intent arrangement used in previous financial years. Instead, in 2009-10 the Minister wrote a letter to the Chief Executive Officer outlining Medicare Australia’s directions for the financial year. To support this letter a strategic directions document was developed. EXTERNAL AND INTERNAL SCRUTINY External audits In 2009-10 the ANAO issued several audit reports that involved Medicare Australia. For detailed information, see Appendix H: Australian National Audit Office activity on page 204. Medicare Australia actively responds to all ANAO recommendations, and the Medicare Australia Audit Committee monitors progress. ANAO representatives are invited to attend all audit committee meetings as observers. In many cases ANAO recommendations directly involve the responsibilities of policy departments. As the service delivery agency, Medicare Australia works with policy departments to help them effectively respond to the recommendations. The Joint Committee of Public Accounts and Audit is required by the Public Accounts and Audit Committee Act 1951 to examine all Auditor-General reports that are tabled in the parliament. The joint committee’s review procedures are built around a series of public hearings, at which evidence is provided by agencies who have been the subject of recent ‘significant’ audit findings. Medicare Australia did not attend any hearings in 2009-10. Internal audits Medicare Australia has an active and effective audit function which carries out internal audits to identify risks and opportunities for improvement. The audit program is developed through consultation with business areas within Medicare Australia and addresses corporate strategic risks to correctly target audit and assurance activities. The audits provide independent assurance on management performance in maintaining Medicare Australia’s strategic priorities, achieving operational objectives in line with organisational and legislative requirements, and ensuring that high standards of probity and accountability are met. Additionally, Medicare Australia: works closely with the ANAO and provides advice to the Joint Committee of Public Accounts and Audit undertakes periodic external benchmarking to ensure that it continues to conform to best practices ensures its employees undertake professional development activities fosters external relationships with private and public sector audit organisations maintains external networks within the Human Services portfolio and other audit areas within public sector departments and agencies and the broader audit community. Action on audit recommendations is monitored and reported to the Medicare Australia executive, the Audit Committee and the ANAO. The Medicare Australia 2009-10 internal audit program was aimed at addressing possible weaknesses in the control framework in areas of: governance program performance human resources finance information and communications technology. Fraud control In compliance with the Commonwealth Fraud Control Guidelines 2002, in 2009-10 the Chief Executive Officer of Medicare Australia certified that Medicare Australia complies with the guidelines, conducts risk assessments and prepares payment risk management plans (see Appendix I: Commonwealth Fraud Control Guidelines certification on page 206 for a copy of the CEO’s signed certificate). These assessments and plans include Medicare Australia’s fraud prevention, detection, investigation, reporting and data collection procedures and processes. The requirements are that Medicare Australia: assesses fraud risk and prepares fraud control plans puts in place fraud prevention, detection, investigation and reporting procedures and processes collects and reports annual fraud data, complying with the Commonwealth Fraud Control Guidelines. Medicare Australia also has other avenues available for reporting allegations of unauthorised staff access to customer information on Medicare Australia systems and employee involvement in fraudulent behaviour. Medicare Australia assesses and investigates all allegations of internal fraud and unauthorised access. If necessary, these are then referred to the Commonwealth Director of Public Prosecution for criminal proceedings. Risk management Medicare Australia’s risk management framework is reviewed regularly and revised as needed to achieve best practice. We participate in the annual Comcover Risk Management Benchmarking Survey to gauge the effectiveness and maturity of risk management across the agency; achieving a score of 5.2 in June 2010. The framework is supported by a Chief Executive Instruction, policy, guidelines and reporting templates. The Executive and Governance Branch is responsible for preparing the highest level of risk management plan—the Corporate Risk Management Plan—and ensuring it is monitored by the executive. The Business Planning, Corporate Project Office and Risk Management teams work together to ensure a high level of risk awareness at all levels of business planning, and program and project management. Risk management advisers are available to facilitate workshops and provide advice and assistance with report preparation and reviews. Medicare Australia is transitioning to Risk Management framework which is integrated with the Department of Human Services framework and in line with AS/NZS ISO 31, 000: 2009 (Standard for Risk Management). PROGRAM INTEGRITY As part of the Human Services portfolio, Medicare Australia is responsible for ensuring that public funds are used appropriately by maintaining the integrity of the programs it administers. A key focus of program integrity is ensuring that Medicare Benefits Schedule rebates, subsidies under the Pharmaceutical Benefits Scheme and health-related incentives are claimed correctly and that the right person receives the right payment at the right time. National Compliance Program Medicare Australia’s National Compliance Program describes how Medicare Australia encourages and supports its key stakeholder groups to voluntarily comply with the requirements of the programs it administers. The program is risk-based and identifies a mix of activities to support and manage compliance. In 2009-10 Medicare Australia identified five factors influencing compliance with the programs it administers: increasing complexity growth of services and health professionals changing practice the impact of eBusiness community demand. These can generate a range of non-compliant behaviour including incorrect claiming, noncompliant activity and inappropriate practice. In 2009-10 Medicare Australia’s key areas of focus were: further refining and extending support services enhancing the audit program. In 2010-11 Medicare Australia’s focus areas will be: education—continuing to develop resources to help providers, including new doctors and international medical graduates, to voluntarily meet their compliance obligations stakeholder engagement—the co-design of our compliance initiatives completion of our published work program working closely with other Human Services Portfolio agencies to improve compliance and fraud management. Learning and support Learning and support projects Medicare Australia has developed a suite of resources to help health professionals understand the requirements for billing and claiming benefits. Stakeholder engagement has been a pivotal component in ensuring these resources are appropriately targeted to meet the needs of health professionals. New resources developed over the past 12 months include: eLearning PBS and You—dispensing and claiming for pharmacists (3 modules) PBS and You—for new health professionals (3 modules) PBS and You—prescribing in public hospitals (1 module) PBS and You—prescribing in private practice (1 module) PBS and You—prescribing for optometrists (1 module) Medicare and You—chronic disease management for GPs (3 modules) Medicare and You—treatment for skin lesions (3 modules). Quick reference guides Quick reference guides for Restricted, Authority Required and Authority Required (streamlined) benefits were developed to provide support for prescribers. Medicare Australia worked with public hospitals throughout 2009-10 to develop learning tools for the introduction of new funding arrangements for highly specialised drugs. These learning tools were released in July 2010. Resources The hard copy resources developed in 2009-10 included: ‘PBS and You claiming checklist for community pharmacists’ ‘PBS and You dispensing checklist for community pharmacists’ ‘Dispensing and claiming checklist— for pharmacists and pharmacy staff in participating public hospitals’ ‘PBS and You—Manual for pharmacists and pharmacy staff in participating public hospitals’ ‘Writing a PBS prescription—participating public hospitals’ writing guide. A public hospital PBS kit was mailed to 141 public hospitals participating in the pharmaceutical reforms. This kit included the manual, dispensing and claiming checklists and the writing guide. Additionally, Medicare Australia developed learning tools to support the introduction of new arrangements for funding highly specialised drugs in public hospitals and released them in July. Teletutorial pilot From September to December 2009 Medicare Australia tested a series of teletutorials for new health professionals. Feedback is being used to develop the future strategy for delivery of learning and support for new health professionals. In addition, Regional Training Providers and GP registrars were surveyed in November and December 2009 to seek their input on possible approaches to GP registrar reinforcement learning. Allied health professionals Medicare Australia surveyed 400 allied health professionals in October and November 2009. The findings from this survey will inform our education and support strategy for this provider segment and will be used in the design of future compliance activity. Nurse practitioners and midwives With nurse practitioners and midwives becoming eligible to provide MBS services and prescribe PBS medicine from November 2010, Medicare Australia began working with these groups to understand their work environment as a precursor to developing specific support resources in 2010 and 2011. Face-toface workshops were held with nurse practitioners nationally in June 2010. Learning and support activities Online support From July 2009 to June 2010 there were 34 070 visits to the education pages on the Medicare Australia website, with an average duration of 11 minutes and 17 seconds spent accessing our eLearning programs and other online support. Face-to-face presentations Medicare Australia delivered face-to-face presentations and workshops on a wide range of Medicare and PBS topics to support new and experienced health professionals. These topics included: health assessments chronic disease management mental health treatment items prescribing PBS prescriptions in private practice and public hospitals supplying PBS medicine in community pharmacy. Sessions were delivered to almost 3000 medical practitioners (including GPs, medical interns and specialists), around 3300 pharmacy students and pharmacy interns, 100 medical students and almost 1000 others in the health care industry. Medicare Australia also sponsored exhibit booths at local and national stakeholder events to distribute learning and support materials, or delivered workshops or seminars. These were: General Practice Education and Training (GPET) conference Australian Society of Anaesthetists conference Royal Australian College of General Practitioners conference 8th Annual Allied Health conference Australian College of Rural and Remote Medicine / Rural Doctors Association General Practice Conference and Exhibition (GPCE) Australian General Practice Accreditation Limited (AGPAL). In early 2010 Medicare Australia undertook market research on communications activities relating to its online education services. The findings will be used to improve communications about online education services, and to develop information and education strategies for health professionals. Information services Medicare Australia provides information services and targeted information which help health professionals and members of the public meet their obligations. These are described further on. Travelling with PBS medicine enquiry line The Travelling with Pharmaceutical Benefits Scheme medicine enquiry line (1800 500 147) and related website are initiatives of the Overseas Drug Diversion Program. The program targets individuals who may be illegally sending or carrying Pharmaceutical Benefits Scheme medicine overseas. The enquiry line and website provide information on the rights and responsibilities of Australians when travelling. In 2009-10 the enquiry line received a total of 4147 calls. There were also 30 930 hits on the website. Prescription Shopping Program The aim of the Prescription Shopping Program is to protect the integrity of the Pharmaceutical Benefits Scheme by identifying and reducing the number of patients obtaining medicine subsidised under the scheme in excess of medical need. The Prescription Shopping Program provides information to help prescribers make informed prescribing decisions and thereby assist them to better manage the health outcomes of their patients. Practitioner alert service Medicare Australia contacts prescribers to give them information about their patients who may be obtaining Pharmaceutical Benefits Scheme medicine beyond their medical need. Medicare Australia also writes to patients, notifying them of these concerns and advising them that their prescribers have also been advised. In 2009-10 Medicare Australia wrote to 1180 patients and to 10 060 prescribers about those patients. Prescription Shopping Information Service Medicare Australia’s Prescription Shopping Information Service (1800 631 181) provides eligible prescribers with information on patients whom they suspect may be prescription shopping. This information is provided only when the patient has been identified as a potential prescription shopper according to the criteria set for the Prescription Shopping Program. In 2009-10 the service received over 26 900 calls compared to 24 739 in 2008-09 and sent 5100 patient reports compared to 4709 in 2008-09. This is an 8 per cent increase in the number of calls and an 8 per cent increase in the number of reports sent to prescribers. Compliance management Analysis and research Medicare Australia has a risk-based compliance program to ensure that claiming under the Medicare Australia program meets requirements set out in legislation. Potential non-compliance is identified through internal assessments and analysis of claiming data, information supplied to the Medicare fraud tip-off line, inter-agency intelligence and targeted detection techniques. Fraud tip-off line Members of the public can report suspected fraud by phoning the Australian Government Services Fraud tip-off line (131 524) or online through the Medicare Australia website. Medicare Australia also receives tip-offs about potential fraud cases via fax, mail and email. All tip-offs are assessed to determine whether there are compliance concerns. In 2009-10 Medicare Australia received more than 1864 tip-offs through the Australian Government Fraud Services tip-off line and 1011 tip-offs through other avenues. Risk and data analysis In 2009-10 Medicare Australia began using a new product to identify and accurately analyse compliance risk. The risk work-up is the first step in the risk analysis process and involves identifying risk by conducting a thorough examination of relevant issues. This includes examining the nature of the risk, relevant legislation, any factors that cause the risk to occur and any other issues that could affect how Medicare Australia responds to it. Findings from risk and data analysis have assisted compliance operations by identifying areas where analysis of claiming data will identify incorrect claiming and inappropriate servicing. Artificial intelligence analysis Medicare Australia also monitors claiming using artificial intelligence analysis to identify anomalous patterns of claiming. In 2009-10 the artificial intelligence analysis provided data for compliance audits. Cross-agency compliance operations The Overseas Drug Diversion Program focuses on individuals who may be illegally sending or taking Pharmaceutical Benefits Scheme medicine overseas. Medicare Australia also works with the Australian Customs and Border Protection Service and Australia Post to detect and prevent the illegal export of Pharmaceutical Benefits Scheme medicine through international airports and mail exchanges. In June 2010 Medicare Australia conducted joint operations with the Australian Customs and Border Protection Service at Melbourne and Sydney international airports and mail exchanges. Compliance cases—audits and reviews In 2009-10 Medicare Australia continued to build on the co-design approach adopted in recent years. Medicare Australia engaged with key stakeholders in understanding and identifying the risks to compliance, determining appropriate treatments and in delivering those treatments. If non-compliance (excluding fraud) is suspected, Medicare Australia may do one or more of the following: Compliance audit—to verify that individuals or organisations are entitled to the payments received. Audits are conducted by telephone, letter or face-to-face. If non-compliance is accidental, Medicare Australia will counsel and provide educational material where appropriate. Review of Practitioner claiming profiles—the Practitioner Review Program (PRP) deals with practitioners whose provision of services under Medicare or the Pharmaceutical Benefits Scheme prescribing data suggests that there may be inappropriate practice. If fraud or criminal behaviour is suspected, Medicare Australia will undertake an investigation and if appropriate will refer cases to the Commonwealth Director of Public Prosecutions. In 2009-10 Medicare Australia finalised 3594 compliance cases. Table 41—Completed audit and review cases 2009-10 Population Number Medical practitioner 2365 Pharmacies/pharmacists 273 Members of the public 468 PIP payment recipients 414 PHIR funds 74 Total 3594 Medicare Benefits Schedule and Pharmaceutical Benefits Scheme data matching Budget measure In 2009-10 the government announced a Budget measure to enable the matching of Medicare Benefits Schedule and Pharmaceutical Benefits Scheme data to help improve compliance outcomes. The measure will allow the identification and analysis of claiming patterns for health service activity, such as unusually high claiming of prescriptions or overuse of medical services. This measure will cost $4.2 million over four years to implement and is expected to result in a reduction in incorrect Medicare Benefits Schedule and Pharmaceutical Benefits Scheme payments of $15.4 million over four years, resulting in net savings of $11.3 million over four years. Increased Medicare compliance audits During 2008-09 Medicare Australia implemented the Increased Medicare Benefits Schedule Compliance Initiative which was announced in the 2008-09 Budget. Under this initiative, Medicare Australia’s Medicare audit coverage was increased from less than 1 per cent to about 4 per cent of health professionals. Increased audits began in January 2009, with about 1000 additional Medicare audits conducted in 2008-09. As part of the Budget measure, the government also announced introducing changes to the legislation to: require providers to produce documents to substantiate their Medicare claiming when audited introduce a financial penalty for Medicare providers whose incorrect claims are above a certain amount give providers an opportunity to seek an independent, internal review if they are unhappy with an audit outcome. In September 2009 the government introduced the Health Insurance Amendment (Compliance) Bill 2009 in parliament—the Bill has now lapsed. This means that the Bill must be reintroduced to parliament for further debate prior to it potentially being passed. Professionalism Survey In January 2010 Medicare Australia launched the Professionalism Survey. The survey asks health professionals to assess both Medicare Australia’s audit process and the professionalism of Medicare Australia’s compliance staff. Feedback will be used to inform the training and development of Medicare Australia compliance officers and for the continual improvement of the audit process. In 2009-10 results from the survey revealed that 80 per cent of survey respondents either agreed or strongly agreed that: the reasons for the compliance activities were fully explained their privacy was respected they were treated in a professional manner they had an opportunity to respond to Medicare Australia’s concerns. The Professionalism Survey was developed and implemented after an exit survey of medical practitioners in 2008 revealed that 86 per cent of respondents agreed that Medicare Australia’s compliance officers had acted professionally during the audit process. Medicare Australia will continue to seek feedback from health professionals through its survey program. Compliance Officer Development program The Compliance Officer Development program, a Medicare Australia strategic priority in 2009-10, provides a compliance-focused training framework for affected Medicare Australia and Centrelink staff. The program has been tailored to: meet the current and future business needs of staff within the Customer Service Design and Compliance program provide career and development pathways across the DHS portfolio. Implementation of the technical and leadership qualification elements of this framework is scheduled to begin in November 2010. External referrals Commonwealth Director of Public Prosecutions In 2009-10 Medicare Australia referred eight individuals to the Commonwealth Director of Public Prosecutions for criminal prosecution. The Commonwealth Director of Public Prosecutions successfully prosecuted 12 individuals referred by Medicare Australia. The following table summarises those prosecutions. Table 42—Summary of successful prosecutions 2009-10 Number Repayment orders Medical practitioner 4 $43 708 Pharmacies/pharmacists 1 $16 000 Members of the public 12 $359 234 Total 17 $418 942 Director of Professional Services Review The Professional Services Review is a peer review process established in 1994 to examine suspected cases of inappropriate practice. In 2009-10 Medicare Australia forwarded 36 requests to the Director of Professional Services Review. In 2009-10 the Director of Professional Services Review issued 68 final determinations resulting in: 56 determinations under section 92 of the Health Insurance Act 1973 12 determinations under section 93 of the Health Insurance Act 1973 requests for review of 17 practitioners being dismissed under section 91 of the Health Insurance Act 1973 repayment orders totalling close to $5.07 million. Suspension or revocation of approval to supply under the Pharmaceutical Benefits Scheme Under section 133 of the National Health Act, the approval for pharmacists to supply Pharmaceutical Benefits Scheme medicine and claim Pharmaceutical Benefits Scheme benefits can be revoked by the Minister for Health and Ageing or suspended by the Secretary of the Department of Health and Ageing. In 2009-10 Medicare Australia considered the suspension of one pharmacist under section 133. Before finalisation of this process, the pharmacist surrendered the pharmacy approval number. Medicare Participation Review Committees Medicare Participation Review Committees (MPRCs) are independent statutory committees established on a case-by-case basis under Part VB of the Health Insurance Act 1973. The role of the MPRC is to make independent determinations on whether a practitioner should maintain the right to participate in Medicare. A case can be referred to the MPRC when: a practitioner has been convicted of a relevant offence or civil contravention a practitioner has been found under the Professional Services Review Scheme to have engaged in inappropriate practice on two separate occasions a practitioner or pathology company is reasonably believed to have breached a pathology undertaking. Table 43—Medicare Participation Review Committee determinations Case Reasons for referrals Determination 1 Professional Services Review referral Full disqualification from Medicare for two weeks 2 Criminal referral Full disqualification from Medicare for four weeks 3 Professional Services Review referral No further action 4 Professional Services Review referral Full disqualification from Medicare for three weeks 5 Criminal referral No further action 6 Professional Services Review referral Partial disqualification from Medicare for two weeks 7 Professional Services Review referral Full disqualification from Medicare for two weeks 8 Professional Services Review referral Partial disqualification from Medicare for two weeks 9 Professional Services Review referral Full disqualification from Medicare for two weeks 10 Professional Services Review referral No further action 11 Professional Services Review referral Partial disqualification from Medicare for seven weeks 12 Professional Services Review referral Partial disqualification from Medicare for two years 13 Professional Services Review referral No further action 14 Professional Services Review referral Full disqualification from Medicare for five weeks 15 Professional Services Review referral No further action 16 Professional Services Review referral No further action 17 Professional Services Review referral Partial disqualification from Medicare for five weeks The MPRC can determine different things depending on the type of case. Generally it can determine that no further action be taken, the practitioner be reprimanded, the practitioner be counselled and/or the practitioner be partially or fully disqualified from participating in the Medicare program for up to five years and this can be specific to services, class of persons or location. In 2009-10, 13 practitioners were referred to the MPRC. During the year, the committee made 17 determinations. Details are in Table 43. Debts raised for recovery of benefits incorrectly paid In 2009-10 Medicare Australia initiated action to recover more than $10 million in incorrect payments from more than 600 individuals or entities. This was through: voluntary agreements as a result of audits, investigations or practitioner reviews payment orders resulting from civil litigation payment orders resulting from successful prosecutions payment orders resulting from the Director of Professional Services Review’s determinations payment orders resulting from Medicare Participation Review Committee determinations. Table 44—Debts raised for recovery of benefits incorrectly paid Groups Number Amount Medical practitioners 477 $7 879 181 Pharmacies/pharmacists 100 $1 842 051 Patients/members of public 25 $196 811 Practice Incentive Program recipients 15 $212 587 Other 2 $162 358 Total 619 $10 292 988 Payment accuracy reviews As part of the assurance process, Medicare Australia conducts payment accuracy reviews to estimate the overall level of payment accuracy in the administration of the Medicare and Pharmaceutical Benefits Scheme programs. The reviews measure the level of accuracy by regularly verifying a random sample of services or supplies for which Medicare or Pharmaceutical Benefits Scheme benefits were paid through contact with the health professional and patient. In 2009-10 the level of payment accuracy for Medicare rebates was calculated to be 99.86 per cent and 99.7 per cent for the Pharmaceutical Benefits Scheme. This compares with 99.53 per cent and 99.79 per cent, respectively, in 2008-09. CORPORATE BUSINESS CONTINUITY A severe business disruption could damage Medicare Australia’s reputation and ability to deliver services to the Australian public if the speed or scale of the event is allowed to overwhelm operations and management systems. Medicare Australia has emergency management and business continuity procedures in place to ensure it is prepared to manage such events as they occur. All Medicare Australia divisions maintain a business continuity plan to ensure that effective interim operating arrangements can quickly be put in place to support critical business functions and resources. For each critical function, a maximum allowable outage is nominated to indicate sensitivity to disruption as measured in hours and/or days. Emergency management and business continuity plans were reviewed and several tested by real scenarios in 2009-10. Business continuity communication protocols as well as new after-hours escalation procedures were developed, implemented and tested during 2009-10 to ensure 24/7 availability and accessibility in the event of a service interruption. CORPORATE RECORDS MANAGEMENT A new Corporate Records Management branch in Centrelink is now responsible for ensuring the Department of Human Services, Centrelink and Medicare Australia all comply with recordkeeping requirements and responsibilities as Australian Government agencies. This includes ongoing monitoring of practices and ICT systems while preparing for e-records and records-keeping in the context of connected service delivery across government agencies. CONSULTANCIES Medicare Australia complies with the information published in the Department of Finance and Deregulation’s Financial Management Guidance No 15: Guidance on Procurement Publishing Obligations (July 2007) in distinguishing between consultancy and non-consultancy contracts for annual reporting purposes. During 2009-10, 18 new consultancy contracts were entered into, involving total actual expenditure of $824 637. In addition, 11 ongoing consultancy contracts were active during 2009-10, involving total actual expenditure of $641 651 (all prices include GST). Appendix J: Consultancy contracts on page 207 lists 16 new consultancy contracts let by Medicare Australia during 2009-10 with a value of $10 000 or more. Note that two new consultancy contracts are not listed as they were under $10 000. Table 45 shows total expenditure on consultancy contracts for the current and previous two financial years. Table 45—Expenditure on consultancy services 2007-08 to 2009-10 (incl. GST) Financial year Total consultancy services expenditure 2007-08 $573 253 2008-09 $1 167 482 2009-10 $1 466 288 Annual reports contain information about actual expenditure on contracts and consultancies. Information on the value of contracts and consultancies is available in Appendix J: Consultancy contracts and on the AusTender website: www.tenders.gov.au. Australian National Audit Office access clauses All of Medicare Australia’s templates for contracts of $100 000 or more include standard clauses providing the Auditor-General with appropriate access to a contractor’s premises. Exempt contracts During the year, Medicare Australia had no contracts or standing offers that were exempted from publication on AusTender. Grants Information on grants awarded by Medicare Australia since 1 January 2009 is available on the website at: www. medicareaustralia.gov.au. NATIONAL PROCUREMENT Purchasing activity and contract management Medicare Australia’s procurement activities are carried out in accordance with the Commonwealth Procurement Guidelines (December 2008). Medicare Australia’s Chief Executive’s Instructions and related policy and procedural publications support the guidelines and are regularly reviewed for consistency with the Commonwealth procurement framework. Since January 2006 Medicare Australia has worked jointly with all Human Services portfolio agencies to cooperate in procurement activity. This has taken the form of either a joint approach to the market (clustering) or through contractual arrangements containing provisions allowing access by other Human Services Portfolio agencies (often referred to as piggybacking). Clustering and piggybacking have led to reduced tendering costs and savings through economies of scale. Similarly, Medicare Australia has established clustering and piggybacking arrangements with other Australian Public Service agencies wherever it has been practical to do so. Medicare Australia has also been involved in contributing to a number of whole-of-government coordinated procurement initiatives led by the Department of Finance and Deregulation, such as accounting services, travel services and stationery and office supplies. See page 110 for ICT procurement Key achievements 2009-10. Property management Medicare Australia maintains a leased portfolio of 257 sites occupying 105 529 m 2. The property portfolio comprises nine sites in the ACT, with the rest located in the other Australian capital cities and regional areas. Following an open market tender process, a new property services contract began in July 2009 with Centrelink’s incumbent provider, Jones Lang LaSalle. This new contract also includes Medicare Australia and the Department of Human Services/Child Support Agency with Centrelink as the lead agency. In 2009-10 office lease and associated costs for Medicare Australia were $63.2 million. The Property and Environment branches of Centrelink, Medicare Australia and the Department of Human Services have been integrated into two branches to support the property elements of the portfolio’s service delivery reform program. In an ongoing program to improve service delivery, customer and staff amenity, and enhance the image and presentation of Medicare Australia, seven Medicare Australia sites were partially refurbished or relocated to new premises. A further three sites were also established; Belmont WA, Belmont NSW and Warrawong NSW, as part of the government’s election promises. In total, $35.07 million was spent on capital improvements to Medicare Australia sites. FREEDOM OF INFORMATION, INFORMATION RELEASE AND PRIVACY Freedom of information reforms The new Freedom of information (FOI) reforms were passed in parliament on 13 May 2010 with the principal objective of promoting a pro-disclosure culture across the Australian Public Service to build a stronger foundation for more openness in government. The Department of Human Services (DHS) agencies will proactively ‘push’ information into the public arena, to supplement the current ‘pull’ approach when customers and journalists extract that information from Commonwealth agencies through FOI requests. Some of the reform changes include: no fees for FOI applications no charges for FOI requests for personal information the ability for FOI applications to be submitted online a database for non-personal FOI decisions available online an Information Publication Scheme (IPS) plan to be available on 1 May 2011. The IPS requires DHS agencies to publish a range of information on the internet, or advertise how the information can be obtained. The information includes operational information held by the agency to assist in exercising powers and functions when making decisions or recommendations affecting customers, as well as any other information that the agency may wish to publish. Freedom of information report The following table sets out the reportable freedom of information matters for Medicare Australia in 2009-10. Table 46—Freedom of information requests Requests Number or $ amount On hand at 30 June 2009 3 Received 6 Resolved by being: Withdrawn (following consultation) 1 Granted in full 6 Granted in part 1 Refused in full N/A Requests Number or $ amount Transferred 1 Outstanding at 30 June 2010 N/A Finalised in: 0-30 days 2 31-60 days 6 61-90 days N/A 91 days or more N/A Fees and levies charged: Application fees received $60 Charges notified $110 Charges collected $110 Internal reviews N/A Received N/A Finalised N/A Administrative Appeals Tribunal appeals N/A Received N/A The table below shows Medicare Australia’s performance against freedom of information standards in 2009-10. Table 47—Freedom of information standards Standard 2008-09 Performance 2008-09 Performance 2009-10 We will acknowledge your request under the Freedom of Information Act 1982 within 14 days of receipt and respond within 30 days of receiving your request. If other parties need to be consulted, the law provides for another 30 days for a decision to be made. Thirty-one requests were received. Of these, eight were withdrawn, six were transferred internally, 14 decisions were made and three were carried over to 2009-10. All were acknowledged within 14 days. Six new FOI requests were received. Of these, one was withdrawn, one was transferred and four decisions were made. All were acknowledged within 14 days and responded to within the required time frame. Of the 14 decisions, all but one was responded to within the legislative time frame. There were two requests for internal review of which one was finalised in 2009-10. Privacy of personal information Medicare Australia maintains an extensive range of measures to ensure privacy protection. These enable it to uphold its current high standard of privacy and to ensure that community standards for privacy continue to be met. Chief Executive Instruction 9.5 provides the framework for managing privacy in Medicare Australia. Under this instruction, the Chief Executive Officer issues twice yearly reminders to all staff about their privacy obligations. Privacy training Medicare Australia raises awareness of privacy issues through training, participation in various privacy forums and providing expert advice to internal and external stakeholders. Medicare Australia’s training responsibilities are outlined in Chief Executive Instruction 9.5 and it meets these by ensuring that all ongoing and non-ongoing employees complete privacy training. During 200910 more than 4650 staff completed the privacy training. Privacy impact assessments Medicare Australia maintains an uncompromising commitment to best privacy practice, ensuring new projects and program improvements are developed within a robust privacy framework. Medicare Australia also continues to use the privacy impact assessment process, as required under Chief Executive Instruction 9.5, to mitigate privacy risks and impacts, ensure compliance with legal obligations and build best privacy practice into projects. In 2009-10 Medicare Australia completed privacy impact assessments on a range of significant projects. Comprehensive privacy analysis continues to be done as part of the privacy impact assessment process for projects such as the Superannuation Clearing House project and the Healthcare Identifiers project. Access to personal information Protecting the privacy and confidentiality of personal information is of critical importance. Medicare Australia has high standards of privacy protection and an extensive range of activities which support the relevant legislation and best privacy practice. These activities include: induction training for new staff and follow-up training on identified privacy issues relevant to staff in different business areas privacy impact assessments of new Medicare Australia initiatives involving the collection, use or disclosure of personal information proactive audits of access to personal information to identify any unauthorised access by Medicare Australia staff high-quality and timely privacy advice to all business units to encourage the identification and resolution of any privacy issues as they arise investigating customer complaints and staff reports of possible privacy breaches to ensure action is taken to address any ongoing risks specific processes for releasing personal information to any other agency or person twice yearly messages from the Chief Executive Officer to all staff about privacy standards. Secrecy provisions contained in Commonwealth legislation, specifically the Health Insurance Act 1973 and the National Health Act 1953, make it an offence for Medicare Australia staff to disclose information about a person obtained under those Acts, unless that disclosure is in the performance of their duties, or unless one of the disclosure-enabling sections contained in the secrecy provisions applies. All requests for personal Medicare and/or PBS information are considered case by case according to the secrecy provisions and in many cases require approval or certification by an officer exercising a delegation made by the CEO. Information may be disclosed in response to requests, for example, from state or territory medical boards, other specified Australian Government agencies or in response to requests when a delegate establishes that the disclosure of personal information is necessary in the public interest. Personal information related to other programs administered by Medicare Australia is protected by the Privacy Act 1988 and requests for personal information about those programs are considered under the information privacy principles. Requests for other types of information or documents are, depending on the circumstances, processed under either the Privacy Act or the Freedom of Information Act. Statistics relating to Freedom of information requests are on pages 106-107 of this report. Medicare Australia also complies with the Privacy Commissioner’s guidelines under the National Health Act which deal with personal Medicare and PBS claims information, including its storage and destruction, as well as data- matching restrictions. COMMUNICATIONS ACTIVITIES Integrated communication functions To support service delivery reforms Centrelink took lead responsibility for integrated communication functions across the Human Services portfolio on 1 March 2010. A high priority is placed on effective communication with customers, potential customers, providers and the Australian community. Effective communication provides people with the information they need to make informed choices about Human Services portfolio payments and services, and to understand their rights and obligations when they receive these. In 2009-10 Medicare Australia continued to provide customers and the community with information about its payments and services through a range of accessible channels, including media, print, advertising and, increasingly, online. Communicating with staff From 1 March 2010 corporate communications based in Centrelink began providing integrated solutions to keep staff up to date with the latest corporate information and to ensure staff understand the services and programs offered by their individual agency and the Human Services portfolio more broadly. Medicare Australia CEO Lynelle Briggs shared and received information through a monthly column published in In the loop—the staff newsletter—and through all staff emails. As well, each fortnight Medicare Australia produced Pulse for people managers in the organisation and SES Insight for SES staff. Communicating with health care providers and the public Medicare Australia uses a range of communication tools to support and inform the public, health care providers and its stakeholders about the programs and services it delivers. This includes our website, brochures, mail-outs, newsletters, quick reference guides and fact sheets. We ensure that we are responsive, open and transparent, and produce high- quality information communication products through a range of print, media and other information services. eclaiming communication strategy Medicare electronic claiming—claiming from the doctor’s surgery—has been a major communication activity. Since it began in May 2009 more than three million people have registered their bank account details with Medicare Australia. The post-implementation review undertaken this financial year revealed: awareness of Medicare electronic claiming has doubled Medicare cardholders are now much more likely to have asked their doctor about Medicare electronic claiming medical practices were much more willing to offer the system to their patients—increasing the amount of patient claims processed using this method there was a significant change in attitudes after the campaign compared to before. Community participation Medicare Australia is active within the Australian community. Communication activities have successfully helped raise approximately $74 000 for the Leukaemia Foundation and $80 000 for the Starlight Foundation— helping to grant approximately 15 wishes to sick children. Medicare Australia has received a number of awards for its community support including the Jenny Deck ACT Chief Minister’s award for Community Support for our efforts promoting organ donations in the ACT, and one national and two state awards from the Leukaemia Foundation: seventh place nationally—the highest amount collected by any government agency and an increase on last year’s effort of $59 000 National Office came twelfth in the state awards and NSW state headquarters came nineteenth. Media During the year Medicare Australia engaged with local, national, state and territory media to promote public understanding of Medicare Australia services. Initiatives that attracted significant media coverage included compliance activities, the Small Business Superannuation Clearing House, the Organ Donor Register and online self-help tools. Medicare Australia also maintains close contact with medical industry media outlets, including Australian Doctor and Medical Observer. Medicare Australia works with these publications to proactively promote key education and compliance messages, and to respond to any media enquiries or issues which arise. Media monitoring and analysis has allowed Medicare Australia to critically evaluate the effectiveness of its media activity. This has helped identify emerging service delivery issues so that effective remediation strategies to respond to community enquiries or increases in customer demand can be implemented quickly and effectively. In February 2010, following integration of the communications function across the Human Services portfolio, a centralised portfolio-wide media monitoring process was introduced to achieve a more efficient distribution service. INFORMATION AND COMMUNICATION TECHNOLOGY ICT infrastructure integration As part of service delivery reform, the Department of Human Services is implementing an ICT infrastructure integration program. This will merge the portfolio’s ICT infrastructure, which will deliver a platform to enable customer services integration across the department, Centrelink and Medicare Australia. Medicare Australia’s capability in ICT uniquely places it in the Australian health sector as a key enabler and provider of information and payment services. Increasingly, Medicare Australia is being asked by government to leverage this capability through the electronic delivery of new programs. In 2009-10 new and improved services were delivered for the Australian Defence Family Healthcare program, the Energy Efficient Home Packages program and the Aged Care program, while development and implementation work progressed on the Healthcare Identifiers Service, the Superannuation Clearing House and the Provider Incentives initiatives. Medicare Australia’s ICT capability is based on its: ability to deliver and manage major payment and information systems for several government agencies high availability of ICT systems and infrastructure supporting large-scale real-time eBusiness processing 24 hours a day, seven days a week, all year round secure processing over the internet using Public Key Infrastructure (PKI) substantial business and transaction connections with the Australian health sector, major banks, superannuation funds, small business, federal, state and local government facilitation of online access to information for Australian citizens, health professionals and Medicare Australia service officers major directory systems supporting Australian citizens and health professionals proven disaster recovery capability ICT architecture that enables the re-use of information and technology assets. Key achievements 2009-10 The following outlines Medicare Australia’s key achievements in ICT in 2009-10: Supporting the National E-Health Transition Authority by delivering the ICT components to enable the eHealth foundation services and commencing the roll-out of the Healthcare Identifiers Services to healthcare individuals and providers. Working with the Australian Health Practitioner Regulation Agency on implementing a centralised registration process, and incorporating the necessary changes both in the Healthcare Identifiers Services systems, and business-as-usual systems. Working with the Treasury and the Australian Taxation Office on the Superannuation Clearing House facility, which will reduce red tape and compliance costs for small business associated with meeting their superannuation obligations. Completing the second phase of the new Australian Defence Force Family Healthcare program as part of a trial established by the government to provide free basic medical and dental care to families of Australian Defence Force personnel living in remote and regional locations. Supporting the Department of Environment, Water, Heritage and the Arts by providing electronic registration and payment services for the Energy Efficiency Home Packages project and the Home Insulation Program. Implementing the Indigenous Health Incentive, which involves three types of incentive payments to practices. Implementing full Voice Over Internet Protocol (VOIP) telephony infrastructure across all national, state and regional sites, delivering significant operational and ICT infrastructure savings, and dramatically improving business flexibility by creating a single virtual call centre encompassing more than 2 50 sites across the country. Working collaboratively with the Department of Human Services on all aspects of infrastructure integration to ensure that business as usual is maintained through integration. Completing enhancement releases including Health Professional Online Services, National Bowel Cancer Screening, Aged Care Webforms, Medicare and Veterans’ program, Mental Health Nurse Incentive Payment, Practice Incentive Program eHealth incentive, Australian Childhood Immunisation Register and completion of Phases 1 and 2 of the Online Claiming for Highly Specialised Drugs project for the PBS System. Starting to redevelop the Practice Incentive Program Online, Rural Relocation Incentive Grant, General Practice Registrars Rural Incentive Payments Scheme, Rural Higher Education Contribution Scheme, Midwives Professional Indemnity Scheme and Rural Procedural Grants program. Completing the IT Optimisation project which improves the operational efficiency of Medicare Australia’s ICT systems, people and processes and to achieve Medicare Australia’s Gershon ICT cost-reduction commitments to government. The IT Optimisation project incorporated two major contract extensions which helped achieve the Gershon ICT cost- reduction commitments. During 2009-10 Medicare Australia extended the following contracts: IBM contract Medicare Australia formalised arrangements with IBM Australia to provide ICT infrastructure services for another year. Optus contract Medicare Australia formalised arrangements with Optus to provide telecommunications services for another year. Managed imaging services contract Medicare Australia formalised arrangements with Salmat BusinessForce for its managed imaging services until 30 March 2011. The imaging services Medicare Australia requires include the supply, implementation, support and maintenance of scanner and server hardware, recognition software, data correction software, options for image storage and retrieval software and support services to extract bulk bill claim data from paper form into an electronic format suitable for assessing purposes. Public Key Infrastructure services contract Medicare Australia formalised arrangements with Verizon Australia Pty Ltd for its Public Key Infrastructure (PKI) certificate issuance and ancillary services until 30 June 2010. Following a successful tender evaluation and contract Negotiation, Verizon was awarded a new three- year contract that began on 1 July 2010 and guarantees Medicare Australia with PKI services until 30 June 2013. Card production contract Medicare Australia has formalised arrangements with Giesecke and Devrient Australia Pty Ltd for its card production services until 20 November 2010. As the contract has exhausted its extension options a new request for tender was undertaken. The tender evaluation outcome resulted in a new contract with Placard Pty Ltd. This contract provides the services to produce various cards for Medicare Australia including Medicare and Australian Organ Donor cards. In addition, a number of cards are produced on behalf of the Department of Veterans’ Affairs under a memorandum of understanding. The contract is open to any Australian Government agency which requires similar services. Essential print contract Medicare Australia has formalised arrangements with Salmat BusinessForce for its printing, personalisation and mailing services until 30 September 2010. A new request for tender to provide these services past 30 September 2010 began in January 2010 and will seek responses from members of the Centrelink Personalisation and Mailing Panel using a request for quotation. This will occur early in the new financial year. Key challenges 2010-11 Medicare Australia’s key challenges in ICT in 2010-11 include: supporting the National E-Health Transition Authority after the roll-out of the Healthcare Identifiers Services to healthcare individuals and providers in July 2010 continuing to work with the Treasury and the Australian Taxation Office on implementing the Superannuation Clearing House facility continuing to work with the Department of Health and Ageing on modernising the Aged Care Payment System providing ICT support for activities relating to the take-up of electronic Medicare claiming to reflect the growing interest and demand in the community for speed, efficiency and convenience when accessing government services continuing to work with the Department of Health and Ageing on the package of work that will form part of the Fifth Community Pharmacy Agreement developing and implementing the ICT components of various critical legislative and policy initiatives, including the Practice Incentive Program Online redevelopment, Rural Relocation Incentive Grant, General Practice Registrars’ Rural Incentive Payments Scheme, Rural Higher Education Contribution Scheme, Midwives Professional Indemnity Scheme and Rural Procedural Grants Program ICT Business As Usual Reinvestment fund— as a result of implementing the Gershon Review recommendations, some of the savings have been put back into technical projects to improve service delivery. Medicare Australia successfully bid for funding as part of this process for the following ICT tasks: Medicare ICT System—Remove Hard Coding from Medicare Assessing Medicare ICT System—Enhancement for Pathology Claims. Case Study – To be the ‘best of the best’ Some of the staff from the people services area It’s been a very busy time in the Human Services portfolio since the Minister for Human Services, Chris Bowen MP, announced a series of service delivery reforms in December 2009 aimed at simplifying people’s dealings with government. Responsible for uniting the people services functions from Medicare Australia, Centrelink and the Department of Human Services, Lynelle Briggs—Medicare Australia’s Chief Executive Officer—has a vision for the portfolio to become the high-quality benchmark for people services across the public sector. Each agency had a human resources area, including recruitment, occupational health and safety, workforce security and conditions of service. Under the new integrated structure there will be one area providing people services to all staff across the portfolio—cutting back on duplication and increasing efficiency. Staff enthusiasm for co-location is high. Eventually, all Canberra-based staff in the people team will be co-located at the Tuggeranong (ACT) precinct, providing a complete range of services to staff from one central location. ‘The portfolio is taking the lead in cutting-edge thinking: finding out what other organisations are doing,’ Lynelle says. ‘For instance, the Commonwealth Bank is fairly similar in people numbers to us—40 000— and it’s further advanced in automation and self-help activities. ‘We are very lucky that Katharine McLennan, a people leader from the Commonwealth Bank, has agreed to serve as a member of the portfolio People and Leadership Committee. ‘We’re looking at working smarter. Bigger teams mean service levels will improve because of simple things, such as more people to answer the phone. Self-help services also mean people will be able to enter their own leave through the system and get answers online. ‘We’re bringing together the best of the three agencies, the best of the best—that’s our aim. ‘ OUR PEOPLE Integration of human resources functions The people services functions of the Department of Human Services, Medicare Australia and Centrelink came together on 1 March 2010. There are now two people divisions for the portfolio: People Services and People Capability. Both divisions report to the Deputy CEO, People and Operations, who in turn reports directly to the CEO of Medicare Australia, as the leader of the portfolio’s people services functions. The combined people divisions are responsible for a broad range of portfolio issues, including: diversity and strategic recruitment people development leadership employee relations performance improvement and awards change management ethics and values payroll workforce planning workplace health and safety. Staff profile At 30 June 2010 Medicare Australia employed 5705 people, of which 5419 (95 per cent) were ongoing and 286 (5 per cent) were non-ongoing. Appendix K: Staffing statistics on page 209 presents statistics on staff by classification, employment status, gender and location, and sets out salary ranges under the various employment agreements. Collective agreement Consistent with the Australian Government Employment Bargaining Framework, Medicare Australia is committed to setting employment conditions for staff by a collective agreement. The Medicare Australia Collective Agreement 2008-2011 covers all non-Senior Executive Service (nonSES) employees, apart from employees occupying Medical Officer positions and employees on individual agreements. The collective agreement came into effect on 25 December 2008 and nominally expires on 5 December 2011. Medicare Australia has a separate collective agreement for Medical Officer employees, which came into effect on 31 December 2008 and also nominally expires on 5 December 2011. By agreement, 324 non-SES employees terminated their individual agreements during the year and reverted to coverage under the collective agreement. Managing performance Medicare Australia is committed to being a high-performing organisation by linking individual performance agreements to the organisation’s business goals and strategic directions. Effective management of the individual performance of employees is a key contributor to Medicare Australia’s organisational success. To this end, Medicare Australia requires all employees to participate in its performance management program. The main objectives of Medicare Australia’s performance management program are to: develop a high-performing culture ensure employees are aware of the standards of performance expected of them provide employees with an understanding of what they are expected to achieve during the performance year ensure employees uphold the Australian Public Service values in the course of their duties recognise achievement identify and address capability development needs. Medicare Australia encourages regular ongoing discussions between employees and their managers regarding performance, with formal reviews conducted in November/December and June/July of each year. Senior executive remuneration Senior executive remuneration is determined by the Chief Executive Officer and reflects work value, individual capability, contribution and performance. Relevant market factors and the organisational performance of Medicare Australia are also taken into account. Remuneration is reviewed at the end of the annual performance cycle in June each year (see Appendix L: Employee remuneration overview on page 213). Conditions of employment for all senior executives are contained in determinations made under section 24 of the Public Service Act 1999. These arrangements typically provide for salary, superannuation, access to a motor vehicle or equivalent cash out and other applicable allowances and benefits. Workforce planning Strong workforce planning progress was made during 2009, including: the formulation of a working group to critically examine Medicare Australia’s workforce capacity, capability and workload demand with a particular focus on the operational workforce to provide flexibility in managing Medicare Australia’s workforce in the context of the service delivery reform agenda the establishment of a cross-portfolio workforce planning team. A portfolio-wide human capital planning framework will be designed in 2010-11. Recruitment Medicare Australia continues to promote its focus on serving the Australian community while recognising and aligning with recruitment approaches across the Australian Public Service. Key achievements include: updated intranet content based on best practice recruitment processes recruitment policy review and redevelopment the launch of the workforce Mobility Register to promote internal movement and capability development and the Job Placement Register to facilitate redeployment the design and implementation of a new DHS National Graduate Program a nationally consistent approach to benchmark recruitment activities in line with an integrated approach to recruitment across the Human Services portfolio, the implementation of standard advertising templates nationally from 1 July 2010. Medicare Australia has also collaborated across the Human Services portfolio agencies to provide crossagency recruitment activity and will continue to develop these relationships to provide quality recruitment services. Workplace diversity Medicare Australia is committed to providing an inclusive, diversity-friendly workplace, while ensuring equal opportunity for all of its employees. The new Workplace Diversity Plan 2010-11 (published in March 2010) reflects Medicare Australia’s leadership commitment, embraces responsibility and strengthens workplace values and culture, while improving measures to address employment-related disadvantages (see Appendix F: Commonwealth Disability Strategy on page 199). The new plan will continue to foster a culture which recognises and supports diverse employee strengths so that all can achieve their full potential. The new plan supports: employment and retention for Indigenous Australians people with disability mature aged workers intranet support tools and information about diversity practices development of cross-cultural awareness training mandatory e-learning package for workplace diversity improved organisational workplace diversity statistical data. During 2009-10 Medicare Australia continued its well established workplace diversity programs, including: support, awareness and education for the Workplace Diversity Contact Officer and Coordinator networks education and awareness for all employees stakeholder engagement and attendance at relevant conferences working with other government agencies and disability organisations. Nearly 2 per cent of Medicare Australia’s total workforce identify as having a disability. Indigenous Employment and Retention Strategy At 30 June 2010 Medicare Australia’s Indigenous employees (ongoing and non-ongoing) made up 2 per cent of its total workforce. Medicare Australia continues to work towards becoming an APS employer of choice for Indigenous Australians. The Indigenous Employment and Retention Strategy is continually reviewed and has the following elements: welcome to country and acknowledgment of country protocols have been implemented staff training using an Indigenous e-learning cross-cultural awareness package development of an employment website, assistance line and database, which lets Indigenous Australians know about employment opportunities and employee support in Medicare Australia annual recruitment of Indigenous Australians for the graduate and cadetships programs Indigenous school-based Work Ready Traineeship program in Western Australia— at completion the students receive a Certificate II in Business an Indigenous mentoring program an Indigenous Employees’ Network that promotes staff development, input into policies and practices affecting Indigenous Australians, information sharing, networking and peer support of Indigenous employees an Indigenous identification policy that encourages Indigenous staff members to identify as such celebration and commemoration in Medicare Australia of events such as NAIDOC week, Sorry Day and Reconciliation Week intranet support tools and information about Indigenous policies and practices. Learning and development As part of the national review of the human resources function within Medicare Australia, the learning and development staff located within the states became part of the National Business Capability team. This allowed for consolidation of consistency in national learning products offered. In 2009-10 the Learning and Development team started a targeted process to ensure that corporate mandatory refresher training was undertaken by all staff. This refresher training started with privacy refresher training for all staff, with more than 4650 staff completing this training by 30 June 2010. The mandatory refresher training includes the following topics: APS Values and Code of Conduct records management workplace diversity cultural awareness occupational health and safety security fraud awareness and program integrity. Learning and Development continue to support the front line of the business by developing blended training products to meet the changing needs of the business, through the delivery of varying services. Some of the training packages designed and delivered in-house include: Continence Aids Package Indigenous Health Identifier Health Professional Online Services Medical Indemnity Australian Defence Force Family Healthcare Program. Additionally, the Learning and Development team facilitates planning days and training requirements inhouse to meet business priorities. One such program is the development and delivery of a pilot of a manager development program to support front-line managers in their duties. Corporate governance for staff Medicare Australia has corporate governance information on its intranet to guide the day-to-day work of staff. This information includes the Chief Executive Instructions and a range of policy and procedural documentation, including Medicare Australia Practice Statements. Medicare Australia has a suite of e-learning modules, including one on governance. This module provides an overview of governance, systems and processes, principals of good governance, and defines the employee’s responsibilities in practising good governance. All new employees are encouraged to explore the full range of e-learning modules. Human Services Leadership Forum On 18 June 2010 the inaugural Human Services Leadership Forum was held in Canberra. The forum brought together 45 EL1s and EL2s from across the portfolio to build relationships, share ideas, discuss key issues, identify priorities and engage in two-way dialogue with the executive. The event explored issues around future directions, organisational change, information and communication technology, workloads, staff identity and communication. Overall, participant feedback was positive, with 84 per cent of staff rating the event 7 out of 10 or higher. Ethics and Code of Conduct Medicare Australia is committed to supporting employees to meet their obligations to adhere to APS Values and comply with the Code of Conduct. On commencement with Medicare Australia, all employees are provided with a copy of the Ethics Framework and Ethics and Conduct Handbook. Additionally, the APS Values and Code of Conduct are discussed. Staff survey Medicare Australia’s staff survey was conducted online in late 2009. Results indicated strong levels of employee commitment and engagement with the organisation. Key features of the 2009 staff survey included a focus on the future and business change, and the shift from measuring satisfaction to measuring employee engagement (a composite of satisfaction, pride, commitment, brand advocacy and employer advocacy). The results show that the majority of Medicare Australia employees: believe that the organisation is well placed to deliver the government’s agenda believe that their immediate managers and senior leaders demonstrate the APS Values and Code of Conduct believe that managers value the contribution that employees make and support them to do their jobs believe that Medicare Australia values team work and the privacy of personal information, encourages continuous improvement and allows employees to balance work and home life demands. Employee engagement scores were benchmarked and are well above the Australian public sector average, providing a strong platform for the delivery of current and future services. Medicare Australia awards and recognition The Medicare Australia employee recognition framework has formal and informal acknowledgment at various organisational levels. Recognising outstanding contributions from employees is conducted in a manner consistent with Australian Public Service Values and the Financial Management and Accountability Act 1997, Medicare Australia also has a length of service program acknowledging 5, 10, 1 5, 20, 25, 30 and 35-year employment milestones for employees. The internal formal acknowledgment is structured around annual Regional Excellence Awards across seven regions. Following the regional awards, two recipients (one individual and one team) are selected as winners for the National Excellence Awards each year. Medicare Australia also participates in the following external award programs to support exceptional employee performance: Public Service Medal National Youth Awards Minister for Human Services Award for Excellence in Customer Service to Customers and Stakeholders Australia Day Achievement Awards NAIDOC Awards. Occupational health and safety Medicare Australia is committed to providing a safe and healthy workplace for all employees as required by the Occupational Health and Safety Act 1991. Medicare Australia’s Health and Safety Management Arrangements demonstrate Medicare Australia’s commitment to supporting workplace safety and wellbeing through 11 key elements: the OHS policy OHS structure roles and responsibilities for OHS consultation OHS planning OHS risk management OHS policies and guidelines OHS training OHS reporting emergency preparedness injury management. Medicare Australia has regional OHS consultants located in each capital city and the Workplace Health team in National Office. The regional consultants are responsible for the day-to-day operations of occupational health and safety, rehabilitation and workers’ compensation. The Workplace Health team develops preventative strategies to reduce the number and severity of workplace injuries. Our consultants work closely with the Workplace Health team to implement national strategies in a coordinated way. Achievements in 2009-10 The Workplace Health team educates employees about health, safety and wellbeing. Throughout 200910 the team refreshed the delivery of OHS within Medicare Australia. This included a complete review of the OHS intranet pages, providing an easy reference to OHS in the workplace. Coinciding with the intranet refreshment, our OHS policies and procedures have been transformed into the Medicare Australia Practice Statement framework, delivering a comprehensive OHS framework. In November 2009 a two-day conference for regional OHS consultants was held. The conference focused on ‘Supporting Workplace Safety and Wellbeing’. Agenda items included better management practices for complex return-to-work cases, best-practice rehabilitation case management for complex return-to-work cases and the development of a framework for the prevention of body- stressing injuries. A national OHS induction program has been implemented across Medicare Australia’s geographically diverse network, as well as two mandatory elearning modules consisting of: the legislative guidelines, OHS procedure statement framework and employer and employee responsibilities recommended workstation practices and a guide to good workstation set-up, to support Medicare Australia’s focus on preventing body-stressing injuries. Medicare Australia has also developed keyboard shortcut cards for Microsoft-based programs and for Medicare-specific program users. Employees using keyboard shortcuts will be able to minimise mouse use, and help prevent bodystressing injuries. Workplace security The protective security functions within the Human Services portfolio were consolidated on 1 March 2010. The new team comprising all existing DHS, Centrelink and Medicare Australia physical and personnel security employees is managed by the Human Services Agency Security Adviser (ASA), a new role that rationalises the roles previously performed by the Centrelink, DHS and Medicare Australia ASAs. The team reports to the Branch Manager, People Support Branch. The new Human Services Workplace Security team is managed from National Support Office and has nine outposted security advisers deployed across the Human Services network. It has a portfolio-wide responsibility for the following strategic and operational security elements: the physical security of all Human Services portfolio employees and customers the physical security of all buildings and office space the physical security of Human Services portfolio assets and hard copy information personnel security for all current and prospective Human Services portfolio employees and contractors. Associated with those responsibilities are the following tasks: physical security incident management physical security reviews policy advice and development employee awareness and training personnel security. Chapter 8 – Financial statements for the period ending 30 June 2010 Appendices Appendix A: Commonwealth legislation relevant to Medicare Australia The Medicare Australia Act 1973 provides for the Chief Executive Officer to authorise the exercising of powers requiring a person to give information or to produce a document that is in the person’s custody, or under the person’s control; and the power to obtain a search warrant to search and seize evidential material, in respect of a relevant offence, where warranted. Section 42 of the Medicare Australia Act 1973 specifies that the use of these powers must be reported annually. Table 48—Statutory report under section 42 1 Section 42(1) subsections: a to h 2009-10 (a) The number of signed instruments made under section 8M 0 (b) The number of notices in writing given under section 8P 25 (c) The number of notices in writing given to individual patients under section 8P Note: this is a subset of (b) above. 0 (d) The number of premises entered under section 8u 0 (e) The number of occasions when powers were used under section 8V 1 (f) The number of search warrants issued under section 8Y 3 (g) The number of search warrants issued by telephone or other electronic means 0 under section 8Z (h) The number of patients advised in writing under section 8ZN1 0 Where powers are exercised in relation to a record containing clinical records, the Chief Executive Officer must advise the patient in writing, except under specific circumstances, for example: after reasonable inquiries, the patient could not be located or contacting the patient would jeopardise the investigation. Appendix B: Occupational health and safety Medicare Australia is required under section 74 of the Occupational Health and Safety Act 1991 to provide a report on occupational health and safety activities and statistics on notifiable accidents, dangerous occurrences, investigations and notices under section 68 during the year. Table 49—Occupational health and safety report Action Number Deaths that required notice under section 68 0 Accidents that required notice under section 68 4 Dangerous occurrences that required notice under section 68 6 Investigations conducted under Part 4 0 Tests on plant, substance, or thing in the course of investigations considered 0 Directions given to Medicare Australia under section 45 (that the workplace etc. not be disturbed) 0 Notices given to Medicare Australia under section 29 (provisional improvement notice) 0 Notices given to Medicare Australia under section 46 (prohibition notice) 0 Notices given to Medicare Australia under section 47 (improvement notice) 0 Appendix C: Freedom of information As a part of its obligations under the Freedom of Information Act 1982 Medicare Australia publishes information about freedom of information in terms of its organisation structure, how it functions and the legislative powers it exercises. Medicare Australia also details the types of documents held and how access can be provided to the public to obtain documents. Documents held by Medicare Australia Medicare Australia produces a range of brochures to help explain the various programs it administers on behalf of the Australian Government. These include the Medicare program, the Pharmaceutical Benefits Scheme, the Australian Childhood Immunisation Register, the Compensation Recovery program, the Australian Organ Donor Register, External Breast Prostheses program and Family Assistance. All of these brochures are available, free of charge, from Medicare offices. Medicare Australia’s website provides publications and forms that are publicly available for people to view or download. Medicare Australia’s statement under section 9 of the Freedom of Information Act was updated in May 2008 and is available on the National Archives of Australia website. In accordance with section 8 of the Freedom of Information Act, the following types of documents are held by Medicare Australia and are available subject to the exemption provisions of the Act: administration and policy files agendas, minutes and records of meetings of various internal and external committees and tribunals agendas, minutes and submissions for commission meetings applications for approval as an accredited orthodontist applications for approval as a dentist or dental practitioner applications for recognition as a specialist or consultation physician applications for recognition as a vocationally registered general practitioner brochures relating to Medicare Australia operations committee and tribunal files created as a result of a specific inquiry or hearing committee and tribunal member papers computer records relating to all Medicare Australia operations financial budgetary documents internal audit terms of reference, reports and files legal advice and opinions legislative documents in the form of Acts, regulations and interruptions listings of approved Medicare practitioners and laboratories listings of certified patients for the cleft lip and palate scheme listings of participating Medicare medical practitioners, dentists and optometrists listings of pathology licensed collection centres and accredited pathology laboratories listings of Pharmaceutical Benefits Scheme approved persons as defined under sections 90 and 92 of the National Health Act and pharmaceutical prescribers Medicare Benefits Schedule item rulings and interpretations ministerial, Commonwealth Ombudsman and general correspondence ministerial submissions operational instructions, circulars and directives relating to Medicare, the Pharmaceutical Benefits Scheme, the Australian Childhood Immunisation Register, the Practice Incentives Program, the Compensation Management System, the 30% Rebate on Private Health Insurance, Veterans’ Treatment Accounts, the Australian Organ Donor Register, the Hearing Service Payment, the External Breast Prostheses program, National Bowel Cancer Screening program and the Health Research and Coordinated Care Trials personnel records processed enrolment, registration and withdrawal forms and claims documentation relating to Medicare Australia operations property documents, including leases, tenders and maintenance agreements records created as a result of a specific complaint, inquiry or review records in relation to the regulatory functions of pathology licensed collection centres and accredited pathology laboratories records of contact between medical advisers and medical practitioners statistical reports and analyses undertakings for participating optometrists other records and documents including but not limited to: photographs, maps or diagrams, staff diaries, DVDs and mobile phone SMS messages on Medicare Australia issued phones. Procedure and initial contact points Members of the public or organisations wanting to formally request documents under the Freedom of Information Act should write to: Freedom of Information Officer Medicare Australia PO Box 1001 Tuggeranong DC ACT 2901 Telephone: 02 6124 7914 Fax: 02 6124 6935 Requests should be made in writing, specifying the documents requested, and include a cheque or money order for $30 made payable to Medicare Australia. Remission of the application fee may be sought. Applicants may be liable to pay charges for costs associated with processing a request and providing access to documents. Appendix D: Advertising and market research Section 311A of the Commonwealth Electoral Act 1918 requires Australian Government agencies to report all payments of $10 300 or more made to advertising agencies or to organisations carrying out market research, polling, direct mailing or media advertising. The following table outlines the use of such agencies by Medicare Australia in 2009-10. Table 50—Advertising and market research Payee Purpose Amount Annual customer satisfaction research $150 767 Healthcare Identifiers Communication testing research $80 030 Market research Colmar Brunton Social Research Payee Purpose Amount Online Education Services research $19 800 To conduct recruitment advertising and standard non-campaign Medicare Australia advertising $31 361 To conduct recruitment advertising and standard non-campaign Medicare Australia advertising $135 111 Includes advertising and listing of all Medicare branch offices $362 975 Polling No polling was undertaken during 2009-10 Media advertising HMA Blaze Adcorp White Pages Direct mail No direct mail was undertaken during 2009-10 Total $780 044 Appendix E: Ecologically sustainable development and environmental performance Following the December 2009 announcement of major reform to Australian Government service delivery, environmental management teams from Centrelink, Medicare Australia and the Department of Human Services have integrated to ensure portfolio agencies continue to conduct their business in environmentally responsible ways. Section 516A of the Environment Protection and Biodiversity Conservation Act 1999 (EPBC Act) requires Australian Government organisations to report annually on their environmental performance and contribution to the principles of ecologically sustainable development (ESD). All agencies of the Human Services portfolio are committed to: complying with all relevant environmental legislation and regulations conducting their operations in a manner that minimises environmental impacts and prevents pollution setting environmental objectives and targets to enable continuous improvement. How activities of Medicare Australia accord with the principles of ecologically sustainable development—section 516a(6)(a) During 2009-10 Medicare Australia continued to operate in an environmentally responsible manner. Potential impacts associated with its operations were mitigated through efficient use of resources, effective waste management and pollution prevention. Medicare Australia continued to implement its environmental management system that is aligned to the International Standard ISO 14001: 2004. Environmental policies, plans and procedures influence the decision-making processes of the agency. Programs administered by Medicare Australia during 2009-10 that accord with the principles of ecologically sustainable development — section 516A(6)(a) Medicare Australia has procurement guidelines, motor vehicle policies and sustainable office practices that accord with ESD principles. Details of these policies and practices are reported under ‘Measures taken to minimise the effect of our activities on the environment’. Examples of programs administered by Medicare Australia that were relevant to and met ecologically sustainable development principles included: Drought assistance Drought buses have travelled to rural areas of New South Wales, Victoria, South Australia and Queensland as part of the Australian Government’s drought assistance package. The buses visit the worst affected areas to provide a whole-of-government mobile service. Staff provided Medicare services such as enrolment and card replacement and assisted with Family Assistance services. Natural disaster response Medicare Australia staff have joined crisis response units to deliver Australian Government assistance to communities and individuals adversely affected by natural disasters. Medicare Australia has helped the public, providers, hospitals, pharmacists and community-help groups to access its services and related information. Liquefied Petroleum Gas Scheme Medicare Australia has assisted with the Liquefied Petroleum Gas (LPG) Vehicle Scheme which encourages the use of liquefied petroleum gas as a transport fuel. LPG is the most popular alternative fuel used in Australia. The lower carbon-to-hydrogen ratio and higher octane rating of LPG offers the potential for LPG-fuelled vehicles to deliver reduced carbon dioxide emissions. How Medicare Australia’s outcomes contribute to the principles of ecologically sustainable development— section 516A(6)(b) A key organisational outcome for Medicare Australia in 2009-10 was improving Australia’s health through payments and information. One of Medicare Australia’s priorities during 2009-10 was to deliver great service to all Australians and make it easy for them to conduct business. There is a growing demand from the community for efficient, fast and convenient service from government agencies. To meet this need Medicare has encouraged electronic business through electronic claiming. A consequence of supporting electronic claims and online services is a reduction in paper- based claiming. Medicare’s clients can choose to access its services online or claim rebates at medical practices, reducing or eliminating the need to travel to Medicare offices. Effect of the activities of Medicare Australia on the environment— section 516A(6)(c) Medicare Australia’s daily operations have an impact on the environment. While carrying out our business, resources such as electricity, paper and water are consumed and waste is generated. Medicare Australia is committed to managing the impacts of its business activities on the environment and improving its environmental performance. Measures Medicare Australia is taking to minimise the impact of its activities on the environment— section 516(6)(d) Environmental management system The Environmental Management System is a tool to manage the impact of the portfolio’s business activities on the environment. The system contributes to Medicare Australia’s program outcomes and accords with the principles of ecologically sustainable development. Implementation of its Environmental Management System has generated significant environmental benefits for Medicare Australia. It has also facilitated better resource allocation and cost savings, and contributed to overall staff satisfaction. Environmental impact assessments Medicare Australia conducts assessments of the potential environmental impact of proposed changes to operations such as the implementation of new programs and the introduction of new technologies. The primary aim of these assessments is a precautionary management approach to prevent unintended environmental consequences from the introduction of new projects. The assessment, which considers the potential environmental impact against government benchmarks, is taken into account in final decision making and has the added benefit of achieving better business and resource management outcomes. Environmental policies, procedures and guidelines Medicare Australia’s policies, procedures and guidelines inform the public and its staff of the way it manages its environmental performance. These policies, procedures and guidelines ensure the environment is considered during business planning and decision-making processes. 2009-10 environmental management targets under Medicare Australia’s Environmental Management System, objectives and targets are regularly reviewed to respond to changes in government environmental policies or changing business parameters. These targets allow us to measure the effectiveness of the environmental management plans that we have implemented. Table 51 outlines Medicare Australia’s environmental targets for 2009-10. Table 51—Medicare Australia’s environmental targets 2009-10 Measure Target Energy Office—Tenant light and power < 7, 500 MJ per person Office—Central services < 400 MJ per m2 Other buildings < 130 MJ per m2 Greenhouse Total greenhouse emissions < 17, 000 CO2-e tonnes Total greenhouse offsets > 1, 500 CO2-e tonnes Ethanol blended fuel utilisation E10 utilisation > 35% Paper use External paper use (tonnes) <3000 tonnes Internal A4 copy paper use (tonnes) <150 tonnes Waste General office landfill waste of total < 6.0% Percentage of refurbishment waste diverted from landfill > 80.0% Procurement and the environment Medicare Australia has ensured that environmental considerations are part of normal procurement practice, consistent with traditional factors such as product safety, price, performance and availability. Procurement decisions are no longer confined to considerations of price and functionality but include considerations of environmental performance as well. Environmental performance provisions are now being included in Medicare Australia procurement tenders and associated contracts. Environmentally aware business culture Medicare Australia adopts a continuous education program to train staff on environmental policies and procedures, raising environmental awareness and improving environmental performance. Internal environment program A network of state-based Econet members has been established. Econet members have a local or regional role of communicating and promoting green office awareness practices, and overseeing the implementation of environmental recommendations within the business generally. In practice, this arrangement generates local environmental networks within the various business units of Medicare Australia’s organisational structure. The program is supported by training and awareness activities included in the Medicare Australia’s National Induction Program. All new Medicare Australia employees participate in this training. External—government sector Medicare Australia continues its role as a key member of the Government Agencies Environment Network. The network was established by Centrelink, the Department of Defence and the Australian Taxation Office to drive environmental performance improvements within public agencies. It aims to: share best-practice ideas on environmental management initiate best-practice activities for public agencies facilitate uptake of ideas within agencies. The Government Agencies Environment Network now has more than 30 participating agencies. Energy Overall performance Energy use is considered to be Medicare Australia’s most significant environmental aspect. During 200910 Medicare Australia continued to perform substantially better than Energy Efficiency in Government Operations (EEGO) targets set for 2011-12. Medicare Australia continued to focus on reducing energy consumption by: improving the energy efficiency of its property portfolio promoting good energy management practices to its employees. Energy conservation Since May 2007 Medicare Australia has conducted environmental assessments at national, capital city and Medicare branch offices. Audit findings and recommendations are presented to the site manager for planning and budget consideration. Medicare Australia has commissioned independent energy audits at larger sites. These assessments have identified areas for improvement. Table 52—Transport energy use 1 Measure Metric 2007-08 2008-09 2009-10 Transport energy use GJ 8379 6169 59101 Cars GVG 10.5 and above % 45 74 731 Ethanol blend fuel use (year end) % 30 36 581 Data has not been independently verified and may be subject to change. Supply Medicare Australia continued to support the growth of the renewable energy sector during 2009-10 by incorporating a component of green and/or renewable energy in energy- related procurement arrangements. Transport Medicare Australia has made changes to its various administrative policies associated with motor vehicles to ensure vehicle numbers nationally are kept to the minimum necessary to meet business needs. During 2009-10 Medicare Australia focused on reducing and improving fleet vehicle fuel consumption, improving usage rates of bio-fuels and reducing air travel. Seventy-three per cent of the Medicare Australia vehicle fleet is comprised of vehicles with a Green Vehicle rating of 10.5 or better. The number of hybrid vehicles in the Medicare Australia fleet increased by 10 per cent and ethanol (E10) fuel usage increased by 22 per cent. These results contributed to reduced photochemical smog and greenhouse gas emissions. Medicare Australia continued to offset 100 per cent of its vehicle fleet emissions through Greenfleet. The greenhouse gases generated by the fleet’s operations were offset by the planting of native trees. The trees improved water quality, reduced soil degradation and provided an essential habitat for native animals. Medicare Australia continued to work on reducing air travel by improving Medicare Australia’s capacity to conduct business via video and teleconferencing arrangements. Paper All copy paper purchased by Medicare Australia contains 50 per cent recycled content. Awareness campaigns encouraging duplex printing, on-screen editing and electronic filing continued to be conducted during 2009-10. Table 53—Materials use Measure Metric 2007-08 2008-09 2009-10 Green office consumables % 45 51 48 Paper use (internal copy) tonnes 169 123 143 Paper use (forms, letters, envelopes) tonnes 2946 3229 3188 Recycled content (copy paper) % 50 50 50 Materials Table 54—Water use for Medicare Australia National Office Measure Metric 2007-08 2008-09 2009-10 Water use (National Office only) kL/m2 0.77 0.64 0.66 Water Medicare Australia focused on methods that could be used to accurately determine its total water use. However, a lack of comprehensive metering within the property leased generally and the nature of many property leasing arrangements required water usage to be estimated. Staff education within the organisation continued to encourage the conservation of water. The installation of water conservation solutions were included during accommodation refurbishment activity. Waste Medicare Australia aims to reduce the amount of waste sent to landfill. New recycling streams were introduced to divert hazardous waste from landfill. Medicare Australia sought more information on waste going to landfill from cleaners, builders carrying out accommodation refurbishment and related fit-out activity. Recommendations from audits and trials were implemented to increase the percentage of recycling. Greening information and communications technology strategy In response to the 2008 Gershon Review of Information, Communications and Technology (ICT) in Government, Medicare Australia developed an ICT Energy Management Plan. To improve the environmental performance of its ICT estate the Australian Government initiated the development of a whole-of- government ICT Sustainability Plan. This requires large government agencies to develop an ICT energy management plan. Medicare Australia has identified areas for improvement, considered how ICT can enable sustainability and estimated its ICT energy consumption. Medicare Australia is committed to working towards ICT energy consumption targets and reviewing the plan annually. Medicare Australia mechanisms for reviewing and increasing the effectiveness of its environmental management strategies—section 516A(6)(d) During 2009-10 Medicare Australia continued to implement its environmental management system. Objectives, targets and performance indicators were determined and reviewed on a regular basis. An annual management review is conducted to assess the suitability and effectiveness of the environmental management system. The process provides the opportunity to improve the system and in turn reduce exposure to risk whilst improving overall environmental performance. Table 55—Waste Measure Metric 2007-08 2008-09 2009-10 Landfill waste (of total) % 6 6 6 Fluorescent tube recycling % 30 75 75 Appendix F: Commonwealth Disability Strategy Under the Commonwealth Disability Strategy, during the year Medicare Australia continued work on the Workplace Diversity Plan 2010-11. The Commonwealth Disability Strategy provides a framework to assist Australian Government departments and agencies to meet their obligations under the Disability Discrimination Act 1992. Under the strategy, Australian Government agencies are obliged to remove barriers which prevent people with disability from having access to policies, programs and services. Medicare Australia’s Workplace Diversity Plan 2010-11 incorporates objectives for attracting, employing and retaining people with disability. The Workplace Diversity Plan is a principles- based document that closely aligns to the Australian Public Service Values. The objectives of the plan: 1. To build on our organisation’s previous equity and diversity achievements. 2. To pursue, develop and maintain strategies aimed at attracting, employing and retaining people with disability in our organisation, so that we are seen by people with disability as an employer of choice. This will be achieved through; a. supporting the employment of people with disability in our organisation and removing barriers to that employment b. providing reasonable adjustment and support to our people with disability in the workplace c. educating our people regarding what a disability is, the facilities available to assist those with disabilities, and encouraging employees to identify as having disability where appropriate d. educating and supporting the managers and colleagues of our people with disability e. promoting our organisation as an employer of choice for people with disability. Communicating with people with disability Information affecting customers with a disability, illness or injury is available in alternative formats. These formats include audio cassette/CD, large print, braille and e-text. Medicare Australia can also provide these products on request. Usability of Medicare Australia’s website Medicare Australia is committed to improving the accessibility and usability of website information for all Australians, including those with a disability or with technical limitations. Contacting Medicare Australia Medicare Australia’s TTY numbers and the National Relay Service allow people with disability to contact Medicare Australia by phone. Purchasing and procurement Purchasing specifications reflect requirements of the Disability Discrimination Act 1992 and make particular reference to people with disability when required. Medicare Australia’s standard contracts contain a clause that requires contractors to comply with the requirements of the Disability Discrimination Act 1992. Policy development In working with its partner departments and agencies—for example, the Department of Health and Ageing and the Department of Veterans’ Affairs—Medicare Australia assists in developing and implementing policies that take account of the needs of people with disability. Accessibility in Medicare offices Assistive listening devices are available in selected Medicare offices to provide better access to services for people with hearing impairments. The provision of adequate physical access to Medicare offices is a mandatory component of all lease negotiations. For more information refer to Access and equity on page 86. Appendix G: Services delivered on behalf of our partners—200910 year in summary Note: Financial and other data in this annual report have been rounded to the nearest decimal point. This may lead to some discrepancies in the total figures. Medicare 1 Persons enrolled in Medicare1 at 30 June 2010 22.1 million Active Medicare cards at 30 June 2010 12.4 million Bulk billed services 229.3 million Patient claimed services 79.1 million Total services processed 308.4 million Percentage of services bulk billed 74.3% Total benefits paid $15.4 billion includes some people who are not Australian residents (such as long-term visitors for more than 6 months and eligible short term visitors). Pharmaceutical Benefits Scheme and Repatriation Pharmaceutical Benefits Scheme PBS services processed1 183.9 million RPBS services processed2 13.8 million Total services processed 197.7 million PBS benefits paid1 $7.8 billion RPBS benefits paid2 $485.3 million Total benefits paid $8.3 billion Authority prescriptions authorised 6.5 million 1 including stoma 2 payments to veterans processed on behalf of the Department of Veterans’ Affairs Aged Care 1 Residential claims processed 33 876 Community Aged Care Package claims processed 13 654 Total flexible care claims processed 7900 Total claims processed 55 430 Total amount paid1 $8.1 billion $1.1 billion paid on behalf of the Department of Veterans’ Affairs Australian Childhood Immunisation Register Valid immunisation episodes recorded 4.7 million Children (under 7) registered 2.1 million Total amount paid to immunisation providers $8.9 million Children registered with appropriate immunisation coverage at 30 June 2010 aged 12-15 months 91.5% aged 24-27 months 92.4% aged 60-63 months 89.6% Australian Organ Donor Register Number of consent registrations (including registrations of intent by 16-17 year olds) 1 395 792 National Bowel Cancer Screening Register Invitations distributed 515 593 Practice Incentives Program Participating practices at 30 June 2010 4881 Total amount paid $229.2 million Mental Health Nurse Incentive Program Total amount paid $21.6 million Number of participating practices at 30 June 2010 629 Rural Retention Program Number of providers paid 2298 Number of payments made 2362 Total amount paid $24.6 million General Practice Immunisation Incentive Scheme Number of practices registered at 30 June 2010 5555 Total amount paid $20.2 million General Practice Registrars’ Rural Incentive Payments Scheme Medical practitioners paid 664 Number of payments made 1248 Total amount paid $17.3 million Rural Procedural Grants Program Number of providers paid 1552 Number of payments made 3635 Total amount paid $16.1 million Compensation Recovery Program Number of cases finalised 47 876 Total amount of benefits recovered $37.9 million HECS Reimbursement Scheme Number of medical graduates paid 462 Number of payments made 826 Total amount paid $5.4 million Hearing Services Program Services processed1 1 099 690 Total amount paid2 $294.0 million 1 Services provided to individuals. 2 Payments made to hearing contractors. 30% Rebate on Private Health Insurance Memberships registered 5.7 million Total paid in cash claims $2.2 million Total paid to health funds $4.3 billion Medicare Australia online claiming Number of registered sites transmitting via online claiming 11 244 Bulk billed services transmitted via online claiming 198.0 million Patient claimed services transmitted via online claiming 11.7 million Medicare Easyclaim Number of transmitting sites 6830 Bulk billed services transmitted via Easyclaim 11.2 million Patient claimed services transmitted via Easyclaim 3.7 million Electronic Claim Lodgement and Information Processing Service Environment (ECLIPSE) Number of transmitting sites 1225 Number of simplified billing services transmitted via ECLIPSE 3.0 million Online patient verifications transmitted 69.8 million On behalf of the Department of Veterans’ Affairs Veterans’ treatment accounts 1 Cards produced1 61 329 Total services processed 21.7 million Total benefits paid $2.1 billion Personal Treatment Entitlement cards, Repatriation Pharmaceutical Benefits cards, Specific Treatment Entitlement cards and Totally Permanently Incapacitated Gold cards. Before 2004-05 Medicare Australia’s funding for the processing of DVA services was allocated based on the number of lines processed. The output pricing agreement has since changed and Medicare Australia’s funding is now allocated based on the number of DVA services processed. Care should be taken when comparing the statistics in this table with those of earlier years, which used lines instead of services. Service and benefit figures include incentive items. On behalf of the Department of Innovation, Industry, Science and Research LPG Vehicle Scheme Number of applications received by Medicare Australia 32 162 Percentage of total applications received 74.0% On behalf of the Department of Families, Housing, Community Services and Indigenous Affairs Family Assistance Number of claims granted 187 633 Number of FAO inquiries 345 769 On behalf of the Department of Climate Change and Energy Efficiency, and the Department of the Environment, Water, Heritage and the Arts Home Insulation Program Number of claims paid to installers by Medicare Australia 1 133 876 Value of rebate payments made to installers by Medicare Australia $1.6 billion Appendix H: Australian National Audit Office activity ANAO liaison The Portfolio Audit and Assurance Division continues to work closely with the Australian National Audit Office (ANAO) on developing and coordinating the contribution of Medicare Australia’s divisions and branches to the ANAO’s audit activities and monitors the implementation of recommendations from ANAO audit reports. Medicare Australia has a collaborative and productive relationship with the ANAO and welcomes the audit and assurance activities it undertakes. Additionally, the ANAO Better Practice guides are considered useful resources for Medicare Australia to assist with improving business practices. ANAO audit reports that have been tabled can be found on the website: www.anao.gov.au. Full reports are published, including the recommendations. Australian National Audit Office audits tabled 2009-10 Report 2 of 2009-10, tabled 7 September 2009 Campaign advertising review 2009 The objective of the report was to provide the ANAO’s perspective on the operation of the government advertising framework over the first 12 months of operation. The report provides an overview of the current framework for government advertising, identifies the roles of the various agencies, including the ANAO, and provides information on the assurance review activity for government campaigns conducted by the ANAO. Medicare Australia conducted one advertising activity in 2008-09 aimed at non-English speaking audiences following guidelines which require documented justification of campaigns on cost, need and relevance to government responsibilities. Report 17 of 2009-10, tabled 17 December 2009 Audits of the financial statements of Australian Government entities for the period ended 30 June 2009 The preparation of audited financial statements in compliance with the Finance Minister’s Orders is a key element of the financial management and accountability regime applicable to Australian Government entities. The ANAO audit found no significant or moderate issues for Medicare Australia. Report 18 of 2009-10, tabled 18 December 2009 LPG Vehicle Scheme The objective of the audit was to assess the effectiveness of the administration of the LPG Vehicle Scheme. To address the objective, the ANAO considered whether: there was a sound framework for the operation of the scheme grants were promoted, assessed and approved in accordance with relevant guidance and regulations the scheme’s performance was monitored and reported. The audit was a cross-portfolio review and included an examination of the administration of the scheme and the roles and responsibilities of the Department of Innovation, Industry, Science and Research (DIISR) (including AusIndustry), Centrelink and Medicare Australia. One of the three recommendations related to Medicare Australia. As a service delivery partner for the scheme, Medicare Australia supported the recommendation that a formal evaluation be undertaken to assess the impact of the scheme. There is no action for Medicare Australia to take in relation to this recommendation until a formal evaluation by DIISR has commenced. Report 39 of 2009-10, tabled 24 May 2010 Medicare Australia’s administration of the Pharmaceutical Benefits Scheme The objective of the audit was to examine the effectiveness of Medicare Australia’s administration of the Pharmaceutical Benefits Scheme (PBS). In assessing the objective, the ANAO considered: Medicare Australia’s relationship with the PBS policy agency, the Department of Health and Ageing (DoHA) and the service delivery policy agency, the Department of Human Services (DHS) the management arrangements and processes underpinning Medicare Australia’s delivery of the PBS (including the means by which Medicare Australia gains assurance over the integrity of the PBS) how Medicare Australia undertakes its three main responsibilities relating to the delivery of the PBS, namely: approving pharmacies, approving authority prescriptions, and processing PBS claims. The Repatriation PBS and the processes supporting the formulation of the PBS Schedule did not form part of the audit scope. The integrity of individual payment transactions between Medicare Australia and pharmacists was not tested as part of the audit. The audit resulted in five recommendations. Medicare Australia agreed with recommendations one to four. Regarding recommendation five, Medicare Australia had previously advised that changes to the administration of the PBS Safety Net would be a policy matter for DoHA to consider. Medicare Australia has used the audit process to pursue opportunities for improvement and has already implemented recommendation number one. It is actively taking steps to implement recommendations two to four. Medicare Australia is committed to continually seeking to improve its business processes, including the operational arrangements and processes supporting its delivery of the PBS, and the monitoring and reporting of our performance. Report 50 of 2009-10, tabled 24 June 2010 Interim phase of the audit of financial statements of general government sector agencies for the year ending 30 June 2010 This report presents the results of the interim phase of the 2009-10 financial statement audits of all portfolio departments and other major general government sector (GGS) agencies that collectively represent some 95 per cent of the GGS revenues and expenses. The ANAO found that key elements of internal control were operating effectively to provide reasonable assurance that Medicare Australia can prepare financial statements that are free of material misstatement. Continuing ANAO audits As well as the ANAO audits tabled in 2009-10, Medicare Australia contributed to a number of audits that will continue after 30 June 2010. These are: Medicare Australia’s Administration of General Practitioners—Practice Incentives Program Home Insulation Program. Appendix I: Commonwealth Fraud Control Guidelines certification Appendix J: Consultancy contracts Table 56—Consultancy contracts let during 2009-10 valued at $10 000 or greater Reference Consultant Name Description Contract Price (incl GST) Selection Process (1) Justificatio n (2) S05/001/20/ AA APIS Group Pty Ltd ICT Consultancy Services $324 588 Panel C S06/001/64/ AA Booz Allen Hamilton Review of Business Framework $88 444 Panel C PO 3000003405 3000003406 Bull and Bear Assignments Move from Statebased structure to National Program Management Structure - APS 5 job design $51 975 DS B S09/006/02/ AA Bull and Bear Assignments Move from Statebased structure to National program Management Structure - APS 6 to EL2 job design $102 612 Panel B S10/002/01/ AC Deloitte Touche Tohmatsu Audit, Governance and Assurance Services $30 000 Panel B S06/002/07/ AS DLA Phillips Fox Privacy Impact Assessment for Superannuation Clearing House Project $20 900 Panel C C09/030 Mr D Murphy Medical Advisory Services $11 900 DS B C10/019 Price Waterhouse Coopers Review of Superannuation Clearing House processes $55 707 DS B S06/001/17/ AI Price Waterhouse Coopers Due Diligence Assessment $171 874 Panel C S07/002/07/ AI Price Waterhouse Coopers Audit of Superannuation Clearing House Project $137 500 Panel C Reference Consultant Name Description Contract Price (incl GST) Selection Process (1) Justificatio n (2) S07/002/07/ AH Price Waterhouse Coopers Infosec-Registered Assessor Program Certification Assessment $55 000 Panel C C10/008 Record Keeping Innovation Pty Ltd Review of Medicare Australia’s records management program $16 500 DS C C09/029 Dr C M Reid Medical Advisory Services $11 900 DS B C10/007 Stratsec. Net Pty Ltd Security Assessment for Healthcare Identifier Service $25 000 DS C C10/005 Terranovate Group Pty Ltd Advice regarding IT Integration Project $36 736 DS B S06/001/29/ AA Walterturnbull Advice on Medicare Australia’s proposed costing model $24 651 Panel C Total $1 165 287 (1) Explanation of selection process terms drawn from the Commonwealth Procurement Guidelines (December 2008): Open tender (OT)—a procurement procedure in which a request for tender is published inviting all suppliers that satisfy the conditions for participation to submit tenders. Open approaches to the market include requests for tender, requests for expressions of interest and requests for inclusion on a multi-use list, all of which are published on the Australian Government AusTender internet site. Select tender (ST)—a procurement procedure in which the procuring agency selects which potential suppliers are invited to submit tenders. This procurement process may only be used under certain defined circumstances. Direct sourcing (DS)—refers to a procurement process in which an agency invites a potential supplier or suppliers of its choice to make submissions. Direct sourcing may include a competitive process, for example, obtaining quotes. Panel—an arrangement under which a number of suppliers, initially selected through an open tender process, may each supply goods or services to an agency as specified in the panel arrangements. Quotes are sought from suppliers that have prequalified on the agency panels to supply to the government. This category includes standing offers and supplier panels where the supply of goods and services may be provided for a pre-determined length of time, usually at a prearranged price. (2) Justification for decision to use consultancy: A—skills currently unavailable within agency B—need for specialised or professional skills C—need for independent research or assessment. Appendix K: Staffing statistics Staffing statistics At 30 June 2010, 5705 staff were employed by Medicare Australia under the Public Service Act. This was a decrease of 182 staff or 3.09 per cent since 30 June 2009. Part-time work participation has increased to 23.24 per cent of the workforce. Women comprised 80.37 per cent of all staff. All staff figures are based on head count at 30 June 2010. In Medicare Australia more than 3700 staff provide front-line services to our customers either through our offices or through our phone centres and processing centres. The tables below record staff against the positions they normally occupy, noting that some may be working temporarily in other positions. Table 57—Staff by classification and location National Office Classification NSW QLD SA/NT TAS VIC WA Total CEO 1 0 0 0 0 0 0 1 SES Band 3 2 0 0 0 0 0 0 2 SES Band 2 8 0 0 0 0 0 0 8 SES Band 1 32 1 1 0 0 0 1 35 EL 21 243 12 10 6 3 12 6 292 EL 12 333 35 28 20 19 31 9 475 APS 6 273 41 30 16 6 33 15 414 APS 5 160 148 91 49 24 98 49 619 APS 4 144 76 60 31 20 87 34 452 APS 3 19 952 592 254 170 782 359 3128 APS 2 2 68 22 4 8 14 22 140 APS 1 3 32 14 12 61 7 10 139 Total 1220 1365 848 392 311 1064 505 5705 1 Executive level 2. 2 Executive level 1. Table 58—Performance pay 1 Employee groups Employees paid Amount paid Average Range Executive Level 2 114 $624 829 $5481 $525-$13 560 Executive Level 1 78 $315 947 $4051 $1250-$9026 APS 6 and below 100 $271 169 $2712 $662-$5236 Total 292 $1 211 9451 $4150 The performance pay relates to the 2008-09 financial year. Table 59—Ongoing and non-ongoing staff by classification Classification N O Total CEO 0 1 1 SES Band 3 0 2 2 SES Band 2 0 8 8 SES Band 1 0 35 35 EL 2 3 289 292 EL 1 13 462 475 APS 6 10 404 414 APS 5 18 601 619 APS 4 24 428 452 APS 3 71 3057 3128 APS 2 61 79 140 APS 1 84 55 139 Total 286 5419 5705 O = Ongoing; N = Non-ongoing Table 60—Full-time and part-time staff by classification Classification FT PT Total CEO 1 0 1 SES Band 3 2 0 2 SES Band 2 8 0 8 SES Band 1 35 0 35 EL 2 268 24 292 EL 1 418 57 475 APS 6 367 47 414 APS 5 577 42 619 APS 4 417 35 452 APS 3 2133 995 3128 APS 2 92 48 140 APS 1 61 78 139 Total 4379 1326 5705 State Female Male Total National office 734 486 1220 New South Wales 1178 187 1365 Queensland 724 124 848 South Australia / Northern Territory 337 55 392 Tasmania 262 49 311 Victoria 911 153 1064 Western Australia 439 66 505 FT = full-time; PT = part-time Table 61—Staff by gender and location State Female Male Total Total 4585 1120 5705 Table 62—Equity and diversity groups Indigenous Disability NESB* Location O N O N O N National office 11 0 21 0 256 9 New South Wales 29 2 27 2 386 20 Queensland 18 0 14 0 56 5 South Australia 14 0 5 0 44 2 Tasmania 9 3 4 3 10 1 Victoria 19 1 27 0 167 0 Western Australia 7 3 4 0 57 5 Total 107 9 102 5 976 42 O = Ongoing; N = Non-ongoing * Non English Speaking Background Appendix L: Employee remuneration overview Non-Senior Executive Service remuneration arrangements At 30 June 2010, 5658 non-Senior Executive Service employees were covered by the Medicare Australia Collective Agreement 2008-2011 and Medicare Australia (Medical Officers) Collective Agreement 2008-2011. One employee remains on an Australian Workplace Agreement. Medicare Australia Collective Agreement 2008-2011 Table 63 shows the range of job classifications, salaries and additional pay points for employees covered by the Medicare Australia Collective Agreement 2008-2011. Medicare Australia (Medical Officers) Collective Agreement 2008-2011 Table 64 shows the range of job classifications, salaries and additional pay points for employees covered by the Medicare Australia (Medical Officers) Collective Agreement 2008-2011. Table 63—Salary ranges for employees covered by the Medicare Australia Collective Agreement 20082011 Classification Annual salary range Additional pay point Maximum salary approved under flexible employment arrangements Executive Level 2 $97 101—$116 526 $120 432 $132 770 Executive Level 1 $79 837-$93 826 N/A $104 954 APS Level 6 $65 717—$74 775 $77 800 $83 100 APS Level 5 $59 596-$63 909 $65 096 $72 903 APS Level 4 $54 846-$58 672 $60 271 N/A APS Level 3 $47 692-$52 327 N/A N/A APS Level 2 $43 035-$47 203 N/A N/A APS Level 1 $38 282-$42 582 N/A N/A Note: The Medicare Australia Collective Agreement 2008-2011 provides for access to additional pay points for employees conditional upon them meeting prescribed criteria outlined in clauses 7.2, 7.3.1 and 7.6.2. Table 64—Job classifications and salaries for employees covered by the Medicare Australia (Medical Officers) Collective Agreement 2008-2011 Classification Annual salary range Restricted salary range Medical Officer Class 3 $127 513-$133 250 $133 414-$138 572 Medical Officer Class 4 $138 572-$147 664 $152 717-$153 432 Australian Workplace Agreements At 30 June 2010 only one non-SES employee in Medicare Australia was covered by an Australian Workplace Agreement. Table 65—Total amount of achievement bonuses for non-Senior Executive Service employees on Australian Workplace Agreements Classification Aggregated amount Number of employees receiving achievement bonus Average bonus paid per employee Executive Level 2 $624 829 114 $5481 Executive Level 1 $315 947 78 $4051 APS Level 6 $107 515 34 $3162 APS Level 5 $160154 65 $2464 APS Level 4 $3500 1 $3500 Total $1 211 945 292 $4151 Note: This table shows the total amount of bonuses paid during 2009-10 to those on Australian Workplace Agreements prior to reverting back to the Medicare Australia Collective Agreement 2008-2011 coverage. Senior Executive Service remuneration arrangements Table 66—Salary range for Senior Executive Service classifications Salary range for Senior Executive Service classifications 1 SES Band 2/31 $187 630-$277 378 SES Band 1 $140 474-$170 000 SES Band 3 salaries have been included with SES Band 2 salaries because of the small number of staff at that level. Table 67—Performance pay and achievement bonuses for Senior Executive Service employees Performance pay Employee groups Employees paid Amount paid Average Range Band 2/3 (incl Acting CEO)1 11 $142 046 $12 913 $5304-$33 150 Band 1 38 $258 835 $6811 $4052-$13611 Total 49 $400 8812 $8181 1 SES Band 3 and Acting CEO payments have been included with SES Band 2 payments because of the small number of staff at that level. 2 The performance pay relates to the 2008-09 financial year. Appendix M: Resource statements Agency Resource Statements were introduced to Portfolio Budget Statements in 2008-09 to provide information about the various funding sources that the agency may draw upon during the year. Table 68 advises Medicare Australia’s actual available appropriation for 2009-10. Table 68 corresponds to that contained in the Agency Resource Statement in the 2010-11 Portfolio Budget Statements. Medicare Australia operates under one single outcome. Table 69 provides an overview of the total expenses for Outcome 1 by program. Table 68—Agency resource statement—2009-10 Actual available appropriations for 2009-10 $’000 (a) Payments made 2009-10 $’000 (b) Balance remaining $’000 (a-b) Prior year departmental appropriation $131 000 $131 000 N/A Departmental appropriation $651 587 $488 587 $163 000 S.31 Relevant agency receipts $130 497 $130 497 N/A Total $913 084 $750 084 $163 000 Outcome 1 $4786 $4016 Total $4786 $4016 Total ordinary annual services $917 870 $754 100 Prior year appropriation $19 525 N/A $19 525 Equity injections $34 962 $11 866 $23 096 Previous years’ outputs $6550 $6550 N/A Total $61 037 $18 416 $42 621 Ordinary Annual Services1 Departmental appropriation Administered expenses Other services2 Departmental non-operating Actual available appropriations for 2009-10 $’000 (a) Payments made 2009-10 $’000 (b) Total other services $61 037 $18 416 Total resourcing and payments $978 907 $772 516 Balance remaining $’000 (a-b) 1 Appropriation Bill (No. 1) 2009-10, Appropriation Bill (No. 3) 2009-10, Departmental appropriations reduced (Appropriation Act section 9) and Comcover receipts (Appropriation Act section 12) 2 Appropriation Bill (No. 2) 2009-10 and Appropriation Bill (No. 4) 2009-10 Table 69—Budgeted expenses and resources for outcomes Outcome 1—Access to government health and other payment and information services to the Australian public and providers through convenient and efficient service delivery Budget 2009-10 $’000 (a) Actual expenses 200910 $’000 (b) Variation $’000 (a)-(b) Program 1.1: Delivery of medical benefits and services (D) Ordinary Annual Services (Appropriation Bill No. 1) $489 395 $461 328 $28 067 Departmental supplementation $1227 $1227 N/A Revenues from independent sources (section 31) $28175 $29 874 -$1699 Total for Program 1.1 $518 797 $492 429 $26 368 Program 1.2: Delivery of pharmaceutical benefits and services (D) Ordinary Annual Services (Appropriation Bill No. 1) $155 405 $150 643 $4762 Departmental supplementation $566 $566 N/A Revenues from independent sources (section 31) $3250 $1017 $2233 Total for Program 1.2 $159 221 $152 226 $6995 $142 $5305 Program 1.3: Delivery of other benefits and services (D) Ordinary Annual Services (Appropriation Bill No. 1) $5447 Budget 2009-10 $’000 (a) Actual expenses 200910 $’000 (b) Variation $’000 (a)-(b) Revenues from independent sources (section 31) $80 076 $79 061 $1015 Expenses not requiring Appropriation in the Budget year $887 $390 $497 Total for Program 1.3 $86 410 $79 593 $6817 Program 1.4: Medicare rebates—electronic claiming (A) Ordinary Annual Services (Appropriation Bill No. 1) $4381 $3614 $767 Total for Program 1.4 $4381 $3614 $767 $4381 $3614 $767 Ordinary Annual Services (Appropriation Bill No. 1) $650 247 $612 113 $38134 Departmental supplementation $1793 $1793 N/A Revenues from independent sources (section 31) $111 501 $109 952 $1549 Expenses not requiring Appropriation in the Budget year $887 $390 $497 Total expenses for Outcome 1 $768 809 $727 862 $40 947 (D) = Departmental $764 428 $724 248 $40 180 (A) = Administered $4381 $3614 $767 Average staffing level (number) 5251 5089 162 Outcome 1 totals by appropriation type: Administered expenses Ordinary Annual Services (Appropriation Bill No. 1) Departmental expenses Appendix N: Corrections to errors in 2008-09 annual report The following consultancy was omitted inadvertently from those reported on page 224 of Medicare Australia’s 2008-09 Annual Report. Table 70—Corrections to errors in 2008-09 Reference Consultant name Purpose of engagement Contract price (incl GST) Selection Reason process PO 3000003756 Price Waterhouse Coopers Assessment of Due Diligence exercise 79 539 Panel C Appendix O: Compliance index Table 71—Compliance index Reference in Annual Report Guidelines Description Requirement Page number(s) in this report A.4 Letter of transmittal Mandatory iii A.5 Table of contents Mandatory v A.5 Index Mandatory p. 230 A.5 Glossary Mandatory p. 226 A.5 Contact details Mandatory ii A.5 Internet home page address and Internet address for report Mandatory ii Review by departmental secretary or CEO Mandatory Chapter 1 p. 2 9.2 Summary of significant issues and developments Suggested Chapter 1 p. 2-3 9.2 Overview of department’s performance and financial results Suggested Chapter 1 p. 6-12 9.2 Outlook for following year Suggested Chapter 1 p. 2-3 9.1 Part of report Review by Secretary or CEO Reference in Annual Report Guidelines Part of report Description Requirement Page number(s) in this report Significant issues and developments—portfolio Portfolio departments— suggested Chapter 1 p. 4-6 Overview description of department Mandatory Chapter 1 p. 6-12 10.1 Role and functions Mandatory Chapter 1 p. 6-12 10.1 Organisational structure Mandatory Chapter 1 p. 13 10.1 Outcome and program structure Mandatory Chapter 1 p. 10 10.2 Where outcome and program structures differ from PB Statements/PAES or other portfolio statements accompanying any other additional appropriation bills (other portfolio statements), details of variation and reasons for change Mandatory no change 10.3 Portfolio structure Portfolio departments— mandatory Chapter 1 p. 6 Review of performance during the year in relation to programs and contribution to outcomes Mandatory Chapters 2-5 Actual performance in relation to deliverables and KPIs set out in PB Statements/PAES or other portfolio statements Mandatory Chapters 2-5 Performance of purchaser/ provider arrangements If applicable— suggested Chapter 1 p. 8-9 Where performance targets differ from the Mandatory no change 9.3 10 11.1 11.1 11.1 Departmental Overview Report on Performance Reference in Annual Report Guidelines Part of report Description Requirement Page number(s) in this report PBS/ PAES, details of both former and new targets, and reasons for the change 11.1 Narrative discussion and analysis of performance Mandatory Chapters 2-5 11.1 Trend information Mandatory Chapters 2-5 11.1 Significant changes in nature of principal functions/services Suggested Chapter 1-8 11.1 Factors, events or trends influencing departmental performance Suggested Chapters 2-5 11.1 Contribution of risk Suggested management in achieving objectives Chapter 7 p. 94 11.1 Social justice and equity impacts Suggested Chapter 6 p. 86 11.2 Performance against service charter customer service standards, complaints data, and the department’s response to complaints If applicable— mandatory Chapter 6 p. 84 11.3 Discussion and analysis of the department’s financial performance Mandatory Chapter 8 11.3 Discussion of any significant changes from the prior year or from budget. Suggested Chapters 2-5 11.4 Agency resource statement and summary resource tables by outcomes Mandatory Appendix M Reference in Annual Report Guidelines Part of report 11.5 Description Requirement Page number(s) in this report Developments since the end of the financial year that have affected or may significantly affect the department’s operations or financial results in future If applicable— mandatory Chapter 1 Management Accountabilit y 12.1 Chapters 1 and 7 Corporate Governance 12.1 Statement of the main corporate governance practices in place Mandatory Chapters 1 and 7 pp. 12-16, 93-94 12.1 Names of the senior executive and their responsibilities Suggested Chapter 1 p. 13 12.1 Senior management committees and their roles Suggested Chapter 1 p. 1416 12.1 Corporate and operational planning and associated performance reporting and review Suggested Chapter 1 p. 9-11 12.1 Approach adopted to identifying areas of significant financial or operational risk Suggested Chapter 7 p. 94 12.1 Agency heads are Mandatory required to certify that their agency comply with the Commonwealth Fraud Control Guidelines. 12.1 Policy and practices on the establishment and maintenance of Suggested Appendix I Reference in Annual Report Guidelines Part of report Requirement Page number(s) in this report How nature and amount of remuneration for SES officers is determined Suggested Chapter 7 and Appendix L Significant developments in external scrutiny Mandatory Chapter 7 p. 9394 12.2 Judicial decisions and decisions of administrative tribunals Mandatory Chapter 7 p. 9394 12.2 Reports by the AuditorGeneral, a Parliamentary Committee or the Commonwealth Ombudsman Mandatory Chapter 7 and Appendix H Assessment of effectiveness in managing and developing human resources to achieve departmental objectives Mandatory Chapter 7 p. 114119 12.3 Workforce planning, staff turnover and retention Suggested Chapter 7 p. 115116 12.3 Impact and features of enterprise or collective agreements, determinations, common law contracts and AWAs Suggested Chapter 7 p. 115 12.3 Training and development undertaken and its impact Suggested Chapter 7 p. 116117 12.3 Occupational health and safety performance Suggested Chapter 7 p. 118119 12.3 Productivity gains Suggested 12.3 Statistics on staffing Mandatory Description appropriate ethical standards 12.1 12.2 12.3 External Scrutiny Management of Human Resources Appendix K and Appendix L Reference in Annual Report Guidelines Part of report Description Requirement Page number(s) in this report 12.3 Enterprise or collective agreements, determinations, common law contracts and AWAs Mandatory Chapter 7 12.3 Performance pay Mandatory Appendix K 12.4 Assets management Assessment of effectiveness of assets management If applicable— mandatory Chapter 7 p. 105 12.5 Purchasing Assessment of purchasing against core policies and principles Mandatory Chapter 7 p. 104 12.6 Consultants A summary statement of new consultancy services contracts let during the year and their total actual expenditure; ongoing consultancy contracts and their total actual expenditure and a statement noting that information on contracts and consultancies is available through the AusTender website Mandatory Chapter 7 and Appendix J 12.7 Australian National Audit Office Access Clauses Absence of provisions in contracts allowing access by the Auditor-General Mandatory Chapter 7 p. 104 12.8 Exempt contracts Contracts exempt from the AusTender website Mandatory Chapter 7 p. 104 12.9 Commonweal th Disability Strategy Report on performance in implementing the Commonwealth Disability Strategy Mandatory Appendix F 13 Financial Statements Financial Statements Mandatory Chapter 8 Reference in Annual Report Guidelines Part of report Description Requirement Page number(s) in this report 14.1 Occupational health and safety (section 74 of the Occupational Health and Safety Act 1991) Mandatory Appendix B 14.1 Freedom of Information (subsection 8(1) of the Freedom of Information Act 1982) Mandatory Appendix C 14.1 Advertising and Market Research (section 311A of the Commonwealth Electoral Act 1918) and statement on advertising campaigns Mandatory Appendix D 14.1 Ecologically sustainable development and environmental performance (section 516A of the Environment Protection and Biodiversity Conservation Act 1999) Mandatory Appendix E Other Information 14.2 Other Grant programs Mandatory Chapter 7 p. 104 14.3 Correction of material errors in previous annual report If applicable— mandatory Appendix N F List of requirements Mandatory Appendix O References Glossary Administered items Revenues, expenses, assets and liabilities that the government controls, but which an agency or authority manages on the Commonwealth’s behalf Appropriation An amount of public moneys parliament authorises for spending for a particular purpose AusTender The Australian Government’s web-based procurement system, which provides centralised access to all publicly available approaches to market, multi-use lists, annual procurement plans and reported contracts Australian Workplace Agreement An individual written agreement between an employer and an employee about the terms and conditions of employment, made under the Workplace Relations Act 1996 Average staffing level (ASL) The average number of employees receiving salary or wages (or compensation in lieu of salary or wages) over a financial year, with adjustments for casual and part-time employees to show the full-time equivalent Collective agreement A collective agreement relating to employment conditions made directly between an employer and a group of employees Commonwealth Procurement Guidelines The Commonwealth Procurement Guidelines establish the core procurement policy framework and articulate the government’s expectations for all FMA Act agencies and their officials when performing duties related to procurement NABERS NABERS is a voluntary environmental rating system for office premises. NABERS ratings for offices include NABERS Energy (previously Australian Building Greenhouse Rating), NABERS Water, NABERS Waste and NABERS Indoor Environment. Non-ongoing staff member A person engaged as an APS employee under subsection 22(2)(b) or 22(2) (c) of the Public Service Act 1999 Ongoing staff member A person engaged as an ongoing APS employee under subsection 22(2)(a) of the Public Service Act 1999 Key performance indicators (KPIs) These are financial and non-financial measures used to help define and evaluate an organisation’s success. An indicator is usually selected on the basis of relevance as a measure of some aspect of a specific project or operation. Outcome An outcome is the intended result, consequence or impact of government actions on the Australian community. Policy departments Australian Government policy departments are responsible for developing and implementing policies and programs for the Australian community. Medicare Australia and Centrelink deliver payments and services on behalf of a number of Australian Government policy departments and agencies. Portfolio agencies Different government agencies which are accountable to the same minister. Portfolio Budget Statements Budget-related paper detailing Budget initiatives and explanations of appropriations specified by outcome and program by each agency within a portfolio. Programs Australian Government programs deliver benefits, services or transfer payments to individuals, industry/business or the community as a whole and are the primary vehicles for government agencies to achieve the intended results of their outcome statements. Shortened forms ACFI aged care funding instrument ACIRs Australian Childhood Immunisation Registrations ACPA Australian Community Pharmacy Authority ADF Australian Defence Force AGPAL Australian General Practice Accreditation Limited AHPRA Australian Health Practitioners Regulation Agency ANAO Australian National Audit Office APS Australian Public Service BDOs Business Development Officers CACP Community Aged Care Package CCG Consumer Consultative Group CEO Chief Executive Officer CODP Compliance Officer Development Program COTA Council on the Ageing DCCEE Department of Climate Change and Energy Efficiency DEEWR Department of Education, Employment and Workplace Relations DEWHA Department of Environment, Water, Heritage and the Arts DHS Department of Human Services DIAC Department of Immigration and Citizenship DIISR Department of Innovation, Industry, Science and Research DoHA Department of Health and Ageing DVA Department of Veterans’ Affairs EACH extended aged care at home ECLIPSE Electronic Claim Lodgement and Information Processing Service Environment EFT electronic funds transfer EFTPOS electronic funds transfer point of sale ESD ecologically sustainable development FaHCSIA Department of Families, Housing, Community Services and Indigenous Affairs FOI freedom of information FTB A Family Tax Benefit Part A GP general practitioner GPCE General Practice Conference and Exhibition GPET General Practice Education and Training GPRRIPS General Practice Registrars’ Rural Incentive Payment Scheme GST goods and services tax HECS Higher Education Contribution Scheme HI Healthcare Identifiers HPOS Health Professional Online Services ICT information and communication technology IDC interdepartmental committee IM information management IPS Information Publication Scheme IT information technology JLL Jones Lang LaSalle LEAP Locum Education Assistance Program LEAPR Low Emission Assistance Plan for Renters LPG liquefied petroleum gas MBS Medicare Benefits Schedule MDO Medical Defence Organisation MHNIP Mental Health Nurse Incentive Program MLOs Medicare Liaison Officers MPRCs Medicare Participation Review Committees MRCAETS Military Rehabilitation and Compensation Act Education and Training Scheme NAIDOC National Aboriginal and Islander Day Observance Committee NEHTA National eHealth Transition Authority OHS occupational health and safety PBS Pharmaceutical Benefits Scheme PHIR Private Health Insurance Rebate PIP Practice Incentives Program PKI Public Key Infrastructure PRP Practitioner Review Program PSIS Prescription Shopping Information Service RACGP Royal Australian College of General Practitioners ROCS Run-off Cover Scheme RPBS Repatriation Pharmaceutical Benefits Scheme RPGP Rural Procedural Grants Program RRMA Rural, Remote and Metropolitan Area RRP Rural Retention Program RWAs Rural Workforce Agencies SCG Stakeholder Consultative Group SDR service delivery reform SES senior executive service SIP service incentive payments SWPE Standardised Whole Patient Equivalent TIS Translating and Interpreting Service UHI unique Health Identifier (now replaced by the Healthcare Identifier) VCES Veterans’ Children Education Scheme VOIP voice over internet protocol Contact details Office locations National Office 134 Reed Street North Greenway, Australian Capital Territory 2900 Phone: 02 6124 6333 Fax: 02 6282 5025 Postal address: PO Box 1001 Tuggeranong DC, Australian Capital Territory 2901 Capital city offices New South Wales 130 George Street Parramatta, New South Wales 2150 Phone: 02 9895 3333 Fax: 02 9895 3082 Tasmania 199 Collins Street Hobart, Tasmania 7000 Phone: 03 6125 5333 Fax: 03 6125 5700 Queensland 143 Turbot Street Brisbane, Queensland 4000 Phone: 07 3004 5333 Fax: 07 3004 5410 Victoria 595 Collins Street Melbourne, Victoria 3000 Phone: 03 9605 7333 Fax: 03 9605 7980 South Australia 209 Greenhill Road Eastwood, South Australia 5063 Phone: 08 8274 9333 Fax: 08 8274 9371 Western Australia 130 Stirling Street Perth, Western Australia 6000 Phone: 08 9214 8333 Fax: 08 9214 8322 National telephone enquiry service and email contacts People can contact Medicare Australia through its national telephone service, using the numbers listed by subject area on the following page. Calls to 1800 numbers are free except for calls from public pay phones or mobile phones which may be charged at higher rates. Further information can be found on Medicare Australia’s website. People can also contact Medicare Australia about a range of matters through the internet, using the email addresses listed by subject area in Table 67. Enquiry lines open during business hours Service Hours of Operation (AEST/AEDST whichever is applicable unless otherwise indicated) Phone Number 30% Rebate Mon–Fri 7:30am–5:00pm (AWST) 1300 554 463 ACIR General (Australian Childhood Immunisation Reigster General Enquiries Mon–Fri 8:00am–7:00pm / 8:00am–8:00pm (AEDST) 1800 653 809 ACIR GPIIS (Australian Immunisation Register General Practice Immunisation Incentives Scheme) Mon–Fri 8:00am–7:00pm / 8:00am–8:00pm (AEDST) 1800 246 101 ACIR Internet (Australian Childhood Immunisation Register Internet) Mon–Fri 8:00am–7:00pm / 8:00am–8:00pm (AEDST) 1300 650 039 ADF Family Healthcare Program Mon–Fri 8:30am–5:00pm (Australian Defence Force Family Healthcare Program) 1300 3010 505 Mon–Fri 8:00am–5:00pm (Local Time) 1800 195 206 Option 1 Mon–Fri 8:00am (Local Time) 1800 195 206 Option 2 –5:00pm (AWST —Aged Care eBusiness CFL (Customer Complaints and Feedback line) Mon–Fri 8:30am–5:00pm 1800 465 717 Cleft Lip and Cleft Palate Scheme Mon–Fri 7:30am–5:00pm (AWST) 1300 652 492 Compensation Recovery Mon–Fri 8:30am–5:00pm 132 127 Aged Care —Aged Care (Local Time) (Local Time) Department of Veterans’ Affairs Mon–Fri 8:30am–5:00pm 1300 550 017 Option 1 (DVA) Processing (Local Time) —DVA Medical Mon–Fri 8:30am–5:00pm (ACST) 1300 550 017 Option 2 —DVA Allied Health Hours of Operation (AEST/AEDST whichever is applicable unless otherwise indicated) Phone Number Mon–Fri 8:30am–5:00pm 1300 550 017 Option 3 (Local Time) —DVA Hospital Pharmacy Connectivity Initiative Mon–Fri 8:00am–5:00pm 1800 818 111 eBusiness Mon–Fri 8:00am (Local Time) – 5:00pm (AWST) 1800 700 199 Option 1 Mon–Fri 8:00am–5:00pm 1800 700 199 Option 2 (Local Time) —Pharmacy Connectivity Initiative Mon–Fri 8:00am (Local Time 1800 700 199 Option 5 –5:00pm (AWST)) —Health Professional Service —Online Claiming/ Mediclaims Online Services (HPOS) Fraud Tip-off line (Local Time) Mon–Fri 9:00am–4:45pm 1800 202 011 GP Registration (General Practitioner Registration for 90 Day Doctor Scheme) Mon–Fri 9:00am–5:30pm 1800 032 259 Incentive Programs Mon–Fri 9:00am–5:00pm (ACST) 1800 222 032 Option 1 Mon–Fri 9:00am–5:00pm (ACST) 1800 222 032 Option 2 Mon–Fri 8:30am–5:00pm (Local Time) 1800 556 955 Indigenous Access —PIP (Practice Incentive Program) —MHNIP (Mental Health Nurses Incentive Program) Service Hours of Operation (AEST/AEDST whichever is applicable unless otherwise indicated) Phone Number LSPN (Location Specific Practice Number) Mon–Fri 7:30am–5:00pm (AWST) 1800 620 589 Medical Indemnity Mon–Fri 8:30am–5:00pm 1800 813 167 MAAP Hotline / Claim Inquiry NSW: 8:00am to 6:00pm (Local Time) 1300 131 102 VIC: 8:00am to 6:00pm (Local Time) 1300 131 102 QLD: 8:00am to 7:00pm (Local Time) 1300 131 102 TAS: 8:00am to 6:00pm (Local Time) 1300 131 102 SA: 8:00am to 5:30pm (Local Time) 1300 131 102 WA: 8:00am to 5:00pm (Local Time) 1300 131 102 Medicare Levy Exemption Mon–Fri 8:30am–5:00pm 1300 300 271 Medicare Provider Mon–Fri 8:30am–5:00pm (Local Time) 132 150 Option 3 Mon–Fri 8:30am–5:00pm (ACST) 132 150 Option 4 Medicare Provider —ADCCMC (Assisting Doctors Completing Centrelink Medical Certificates) —IHCI (Commonwealth Government Initiative for Northern Territories Indigenous Communities) National Bowel Cancer Screening Mon–Fri 8:30am–7:00pm 1800 118 868 Service Hours of Operation (AEST/AEDST whichever is applicable unless otherwise indicated) Phone Number Online (General Public) Services Mon–Fri 9:00am–5:00pm Enquiries 1300 850 111 Online Technical Support Mon–Fri 8:30am–5:00pm 1300 550 115 Optometrists Date of Service Check IVR Only 24 x 7 1300 652 752 (IVR) Operator intervention Mon–Fri 8:00am–7:00pm Sat 9:00am–4:30pm PBS General and IME (Pharmaceutical Benefits Scheme General and IME) Mon–Fri 8:00am (Local Time 132 290 Option 3 –5:00pm (AWST)) —PBS eBusiness Rural & Remote Program Mon–Fri 8:30am–5:00pm (ACST) 1800 010 550 Simplified Billing Mon–Fri 8:30am–5:00pm 1300 130 043 Option 1 —ASHA (Australian Health Services Alliance) Mon–Fri 8:30am–5:00pm 1300 130 043 Option 2 —BuPA Australia Mon–Fri 8:30am–5:00pm 1300 130 043 Option 3 (Local Time) —Other Billing Special Assistance Mon–Fri 7:30am–5:00pm (AWST) 1800 660 026 Complex Drugs Mon–Fri 8:00am–5:00pm 1800 700 270 Option 1 —Specialised Drugs (Biological Diseases) Mon–Fri 8:00am–5:00pm 1800 700 270 Option 2 —Specialised Drugs Service Hours of Operation (AEST/AEDST whichever is applicable unless otherwise indicated) Phone Number (Botulinum Toxin) Mon–Fri 8:00am–5:00pm 1800 700 270 Option 3 —Specialised Drugs (Herceptin) Mon–Fri 8:00am–5:00pm 1800 700 270 Option 4 —Specialised Drug (Imatinib)s Mon–Fri 8:00am–5:00pm 1800 700 270 Option 5 —Specialised Drugs (Highly Specialised) TTY Hearing Impaired Enquiry Line Mon–Fri 8:30am (AEST)– 5:00pm 1800 552 152 (AWST) VMP (Visiting Medical Practitioners WA) Mon–Fri 8:30am–5:00pm (AWST) 1300 134 113 Enquiry lines open 24 hours a day, seven days a week Service Phone Number AODR AMP (Australian Organ Donor Registe Authorised Medical Personnel)r 1800 556 455 AODR Public (Australian Organ Donor Register Public Enquiries) 1800 777 203 Customs Prescription Drug Smuggling 1800 032 258 eBusiness—HeSA/PKI 1800 700 199 Option 3—HeSA/PKI Medicare Providers 132 150 Option 1—Medicare Provider Medicare Providers 132 150 Option 2—Easyclaim Medicare Providers 132 150 Option 5—Teen Dental Medicare Public 132 011 Option 1—Public General Enquiries Medicare Public 132 011 Option 2—Easyclaim Medicare Public 132 011 Option 3—Teen Dental Medicare Teleclaiming 1300 360 460 NECC (National Emergency Call Centre) 1800 11 22 33 PBS Authority (Pharmaceutical Benefits Scheme Authorities) 1800 888 333 PBS General and IME (Pharmaceutical Benefits Scheme General and IME) 132 290 Option 1—IME PBS General and IME (Pharmaceutical Benefits General and IME) 132 290 Option 2—General Prescription Shopping Information Service 1800 631 181 Travelling with PBS Medicine 1800 500 147 Email addresses for enquiries Aged care agedcare@medicareaustralia.gov.au Australian Childhood Immunisation Register acir@medicareaustralia.gov.au Australian Organ Donor Register aodr@medicareaustralia.gov.au Compensation Recovery compensation.recovery@medicareaustralia.gov.au Customer Feedback customer.feedback@medicareaustralia.gov.au Freedom of information co.foi@medicareaustralia.gov.au GPMOu 90-day scheme 90daypay@medicareaustralia.gov.au IBNR Indemnity Claims Scheme (medical indemnity) medical.indemnity.payments@medicareaustralia.gov.au Information release (Medicare/PBS claiming histories, enrolment details, provider details) co.information.release@medicareaustralia.gov.au Location Specific Practice Number wa.providers@medicareaustralia.gov.au Medicare Australia general enquiries info@medicareaustralia.gov.au Medicare Australia online claiming onlineclaiming@medicareaustralia.gov.au Medicare Australia media communication and government relations info@medicareaustralia.gov.au Medicare public enquiries medicare@medicareaustralia.gov.au Medicare Australia service charter service.charter@medicareaustralia.gov.au Medicare Australia statistics statistics@medicareaustralia.gov.au Medicare provider enquiries medicare.prov@medicareaustralia.gov.au Online Services support olssupport@medicareaustralia.gov.au Online Technical Support Helpdesk onlineclaiming@medicareaustralia.gov.au otseasyclaim@medicareaustralia,gov.au pbsonline@medicareaustralia.gov.au agedcareonline@medicareaustralia.gov.au eclipse.enq@medicareaustralia.gov.au pki@medicareaustralia.gov.au edihelp@medicareaustralia.gov.au Online Technical Support Product Certification itest@medicareaustralia.gov.au Online Technical Support Liaison otsliaison@medicareaustralia.gov.au Medicare Online Claiming Certification itest@medicareaustralia.gov.au Aged Care Online Claiming Certification acep.itest@medicareaustralia.gov.au