My belly hurts.
advertisement

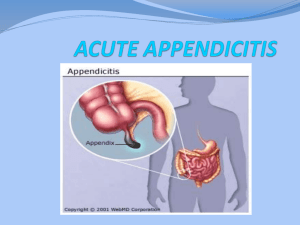
CC: ABDOMINAL PAIN HPI 23 year old female comes in to the Emergency Department with abdominal pain that started 4 hours ago and continues to worsen. Now it is most severe in the right lower quadrant. She decided to come to the hospital when she could no longer tolerate bouncing on the new pogo stick she got for her birthday yesterday. She has also been nauseated and anorexic for the past day. Denies fever, rash, diarrhea, vomiting, hematochezia or melena. HPI Past Medical Hx: Hx of right humeral fracture from trampoline injury. Hx of L fibula fracture from roller blade accident. Hx of pelvic inflammatory disease treated with antibiotics 7 months ago. No past surgical history. Family and Social Hx: Mother has hx of ovarian cysts and ulcerative colitis. Father has hx of diverticulitis. 2 Brothers and 2 Sisters are healthy. Lives in apartment with one roommate. No pets, no recent travel. Works as a taste tester for a local chocolatier. DIFFERENTIAL DIAGNOSIS Appendicitis Ovarian and fallopian tube torsion Perforated appendix Endometriosis Cecal diverticulitis Meckel's diverticulitis Ovarian hyperstimulation syndrome Acute ileitis Ectopic pregnancy Crohn's disease Acute endometritis Tubo-ovarian abscess Renal colic Pelvic inflammatory disease Testicular torsion Ruptured ovarian cyst Mittelschmerz Epididymitis Torsion of the appendix testis or appendix epididymis PHYSICAL EXAM VITALS: BP 130/88, T 38.3, R 28, HR 129 GEN: Appears to be in moderate distress secondary to pain. Speech in interrupted periodically due to increased abdominal pain. HEENT: Normocephalic, atraumatic (NCAT), pupils equal, round and reactive (PERRL) and extraocular movements intact (EOMI). Moist mucous membranes. Oropharynx clear and patent, no erythema. CV, RESP: Tachycardic, regular rhythm, no murmurs, rubs or gallops. Breath sounds are clear to auscultation bilaterally (CTAB), no crackles or ronchi, and symmetrical chest rise. ABDOMINAL: Firm, non-distended abdomen, involuntary guarding and rebound tenderness in the RLQ. Negative Murphy’s sign. Positive Rovsing’s sign, and tenderness at McBurney’s point. PELVIC: No bleeding in vaginal vault, bimanual exam exhibits right adnexal tenderness, no masses appreciated. RECTAL: DRE is negative for gross and occult blood. Perianal area is intact without lesions. NEURO: Alert, awake and oriented to person, place and time. (AAOx3). CN IIVII intact. Strength 5/5 and sensation intact over all extremities. Commonly associated physical findings: •MCBURNEY'S POINT TENDERNESS is described as maximal tenderness at 1.5 to 2 inches from the ASIS, on a straight line from the ASIS to the umbilicus. Sens: 50-94%, Spec 75-86%. •ROVSING'S SIGN: Pain in the RLQ with palpation of the LLQ. Also known as “indirect tenderness” and is indicative of right-sided local peritoneal irritation . Sens:22-68% Spec:58-96%. •The PSOAS SIGN is associated with a retrocecal appendix. Manifested by RLQ pain with passive right hip extension. Due to appendix lying against the right psoas muscle, causing the patient to shorten the muscle by drawing up the right knee. Passive extension of the iliopsoas muscle with hip extension causes RLQ pain. Sens: 13 -42%; Spec: 79-97%. •The OBTURATOR SIGN: associated with a pelvic appendix. Based on the principle that the inflamed appendix may lay against the right obturator internus muscle. When the clinician flexes the patient's right hip and knee followed by internal rotation of the right hip, this elicits RLQ pain, Sens: 8%; Spec: 94%. The sensitivity is low enough that experienced clinicians no longer perform this assessment. LABORATORY TESTS CBC: normal WBC: 14,000 CMP: normal, LFTs normal UA: Negative for WBC, RBC, protein, leukocyte esterase and nitrites. Urine HCG: Negative What would you like to do next? Ultrasound The most accurate ultrasound finding for acute appendicitis is an appendiceal diameter of >6 mm. CT Abdomen CT abdomen with contrast shows: Enlarged appendiceal diameter >6 mm with an occluded lumen Appendiceal wall thickening (>2 mm) Periappendiceal fat stranding Appendiceal wall enhancement Appendicolith (seen in approximately 25 percent of patients Appendicitis Appendicitis is diagnosed based on history and physical examination, Dx can be supported by laboratory and imaging findings. Several studies have demonstrated diagnostic accuracy without the use of imaging to be 75-90%. Though this is also found to be dependent on the level of experience of the examining clinician. Though surgeon dependent it is acceptable to proceed directly to appendectomy without further imaging based on clinical diagnosis. The diagnosis of diagnosis can be difficult and delay results in perforation rates that can be as high as 80%. Most challenging patient populations for this diagnosis include children <3 years of age, adults >60 years of age and pregnant women. Imaging modalities have become increasingly utilized to support the diagnosis, especially US and CT. Some studies have suggested that the increased use of imaging has minimized the number of nontherapeutic appendectomies. In acute appendicitis. However many surgeons will and should proceed with surgical exploration in the absence of imaging if there is strong clinical support, as other studies have shown that imaging studies do not improve diagnostic accuracy for acute appendicitis. Imaging should be performed when the diagnosis of appendicitis is suspected but unclear, and in more challenging patient groups described in previous slides . Histological Interpretations Acute appendicitis is thought to be caused by progressive increase in intraluminal pressure that compromises venous outflow from the appendix which is a normal true diverticulum of the cecum. Often caused by a small stone-like mass of stool called a fecalith. Ischemic injury and luminal stasis causes the structure to become favorable to bacterial proliferation. This results in an inflammatory response including tissue edema, neutrophilic infiltration of the lumen and muscular wall and periappendiceal soft tissue. Histological Features Cont’d Congested subserosal vessels Modest perivascular neutrophilic infiltrate within all layers of the wall Serosa has a dull, granular and erythematous surface Diagnosis of appendicitis requires neutrophilic infiltration of the muscularis propria As the process continues focal abscesses may form within the wall Treatment The goal of therapy of acute appendicitis is early diagnosis and prompt operative intervention. However, this goal is not always easily accomplished since many patients do not seek medical attention in a timely manner and the diagnosis of appendicitis can be difficult. Many surgeons use an aggressive approach, accepting a certain number of negative appendectomies, traditionally 15%, although the use of imaging studies appears to have reduced the negative appendectomy rate to less than 10 %. The preoperative preparation for appendectomy includes intravenous hydration, correction of electrolyte abnormalities, and perioperative antibiotics. Both open and laparoscopic approaches to appendectomy are appropriate for all patients. Patients treated with a laparoscopic appendectomy have significantly fewer wound infections, less pain, and a shorter duration of hospital stay, but higher rates of readmission, intra-abdominal abscess formation, and higher hospital costs. Summary Classic symptoms of appendicitis: right lower quadrant abdominal pain, anorexia, fever, nausea and vomiting. Atypical or nonspecific symptoms: indigestion, flatulence, bowel irregularity, and generalized malaise; and not all patients will have migratory abdominal pain. Diagnostic imaging should be performed when the diagnosis of appendicitis is suspected but unclear. We perform a standard abdominal CT scan with intravenous and oral contrast An appendectomy rather than medical management with antibiotics alone is the gold standard for patients with a history and clinical findings, and radiographic images, consistent with appendicitis. Although some patients do well with antibiotic therapy alone, they are at risk of recurrent appendicitis. Path evaluation of inflammed appendix will involve modest perivascular neutrophilic infiltrate within all layers of the wall and congested subserosal vessels. If a normal appearing appendix is identified during surgical exploration for right lower abdominal pain, an appendectomy should be performed. It is important to search for other causes of the patient's symptoms, including terminal ileitis, cecal or sigmoid diverticulitis or a perforating colon carcinoma, Meckel's diverticulitis, mesenteric adenitis, or uterine, fallopian, or ovarian pathology in a female. References: Black, Carrie E., MD, and Ronald F. Martin, MD. "Acute Appendicitis in Adults: Clinical Manifestations and Diagnosis.” UpToDate, 13 Sept. 2012. Web. 20 Dec. 2012. <http://www.uptodate.com.proxy. medlib. iupui.edu/contents/acute-appendicitis-in-adults-clinicalmanifestations-and-diagnosis?source=search_result&search= appendicitis&selected Title=1~150>. Kumar, Vinay, Abul K. Abbas, Nelson Fausto, Stanley L. Robbins, and Ramzi S. Cotran. "Chapter 17 The Gastrointestinal Tract." Robbins and Cotran Pathologic Basis of Disease. Philadelphia: Elsevier Saunders, 2005. 826-28. Print. Smink, Douglas, MD, MPH, and David I. Soybel, MD. "Acute Appendicitis In Adults: Management." Acute Appendicitis in Adults: Management. UpToDate, 27 Aug. 2012. Web. 20 Dec. 2012.<http://www. uptodate.com.proxy.medlib.iupui.edu/contents/acute-appendicitis -in-adults-management?source=search_ result&search= appendicitis &selectedTitle=3~150>.