Medicine Matters Training Programme Presentation
advertisement

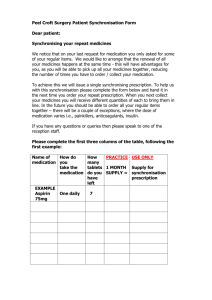
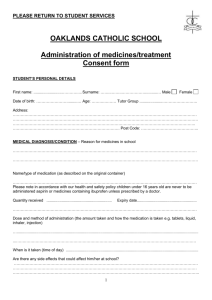
Medicine Matters Training programme in medicine management for carers Introduction Medicine must be taken by: Right person Right dose Right time Right way Learning Objectives Understand carers role Understand good practice Understand problems Understand and follow instructions Understand and follow additional instructions Identify side effects Record Know where to get help Errors happen when Lack of understanding of purpose and use Believing more is better Physical impairment Confusion Forgetfulness Side effects unpleasant Unhelpful comments Errors continued Failure to get the medicine Poor storage Old medicines Roles & Responsibilities Only trained carers can assist with medication Only when authorised by managers Consent from service user Only those medications which have been prescribed with specific instructions Needs assessment The level of help needed will be assessed by GP practice Sometimes in consultation with home care managers Level 1 user Can take full responsibility for her/his own medication Level 2 user Assistance with ordering, collection and disposal Confirming reading of medicine label Opening containers or strip packages Level 3 user Needs assistance with administration of oral dose medicine, some topical preparations and other types of medication where approved, e.g. eye drops Taking the medicine what next? Swallow Stomach Intestine Blood Eliminated Amount of medicine eliminated = amount of medicine absorbed Types of medications How many can you think of? Pills & capsules powders Liquids Patches Creams Drops Gels Sprays Inhaled Intravenous Subcutaneous Pessaries, suppositories. Help is permitted with Tablets Liquids Creams Drops* Gels* Sprays* Pessaries micro enemas* *with advice from primary health care team Help is not permitted with Intravenous medication Subcutaneous medication Diabetes testing Risk Factors What can go wrong? Forgetting to take it Taking too much, too little Taking wrong one Taking someone else’s Risk factors People factors Sensory Impairment Dementia Physical disability Risk factors Medication factors Unclear instructions Pills look alike Packaging hard to open Ordering & Collecting Medication Level 2 user Must request the carer to order Must indicate what medicine, the strength and quantity. Level 3 user Only medicines listed on the chart may be ordered Storage of medication General Safe Cool & dry out of sun Original containers Some in fridge Storage of medicines to be administered by carer Keep together in sealed container labelled Chart to be kept in care plan or alongside Look for special storage instructions Medicine in fridge to be kept separate from food Oral medicine separate from external Disposal of medication Never throw into public waste system List unwanted medicine on disposal form signed by client Return to pharmacy Get signature Dispensing Labels How to take the medicine what would you expect to find? Date of dispensing What is it and how much is there - strength Name DOB Pharmacy address Dosage amount When to take How to take Storage instructions * Expiry date may be on but is not a legal requiremnet Additional instructions Swallow whole Do not crush Take before or on empty stomach 30 minutes Take after food 30 minutes Take regularly complete course Same times Additional instructions Take with or after food During meal Do not take indigestion remedies at same time Minimum of 30 minutes preferably 2 hours Dissolve or mix with water Ensure fully dissolved Additional instructions Allow to dissolve under tongue Take with plenty of water Glassful Apply sparingly No coating on skin about fingertip to cover size of a hand Rinse mouth after use E.g. steroid inhalers may cause thrush Shake the bottle Do it thoroughly Ambiguous instructions or none! When (or as) required As directed As before No instructions Do not administer unless the instructions are clear Side effects List as many as you can think of Nausea - stomach upset Tiredness Motor function affected – dizzy – unsteady Hallucination paranoia Leg cramps Skin itching, skin pallor Side effects Rashes Headaches Confusion Constipation – diarrhoea Restlessness Mood changes General aches and pains Over the counter medicines List the types that client may buy or you may be asked to buy for them Pain killers Indigestion remedies Cold remedies including vapour rubs e.g. Vick Anti histamines Laxatives Vitamin supplements Over the counter medicines Homeopathic medicines Cough medicine Rub ins e.g. rheumatism Steroid nasal sprays Eye nose and ear drops Herbal remedies Antiseptics Check with pharmacist before buying OTC remedies Documentation Must be completed before assistance can be given Self medication assessment Medication permission (level 3) SHCO Medication chart (level 3) GP team Documentation To be completed by carer Medication administration chart (level 3) Medicines disposal chart Documentation emergencies Emergency procedures form GP team Action on reverse of medication chart GP team Administration on reverse of medication administration record Administration Practice All Formulations Clean and tidy space Wash hands Check medicine has not been given Select medicine to be given For each item, read the label, compare with medication chart Assemble medicines to be administered. Administration Practice Put medicine packages back into containers Administer Complete the administration record sheet Wash your hands Administration Practice Solid oral dose formulations (pills and capsules) Transfer the correct number of units into a clean container without touching them Prepare a drink of cold water Ensure client is upright and comfortable Hand the client the container and drink Administration Practice Ask client to take a sip of drink then place medicine on the middle of the tongue and swallow with remaining drink chin slightly down Ensure dose had been swallowed Encourage client to finish drink If client cannot take medicine themselves use a spoon not your hands Administration Practice Liquid oral dose formulations Shake the bottle Measure the correct dose Offer medicine to client If using oral dose syringe expel liquid to the middle of tongue NOT back of throat Clean the bottle with damp tissue before replacing lid Administration Practice Soluble dispersible formulations Measure dose from original container Place in a third of tumbler of cold water Swirl the solution gently in the glass to ensure adequate mixing Hand to client and offer drink afterwards Administration Practice Sublingual formulations Place tablet under the tongue and leave to dissolve Buccal formulations Place the tablet high up between the upper lip and the gum on either side of the front teeth and leave to dissolve Administration Practice Topical (external) preparations Use only as instructed Apply only where prescribed Smallest quantity that will easily rub in Use only for as long as stated Return partly used tubes Wear disposable gloves Administration Practice Transfer the quantity needed to a gloves Gently rub into the skin Dispose of gloves in a sealed polythene bag and place in general waste container Administration Practice Eye Ear & Nose preparations When approval has been given for carers to administer these s/he MUST be given a practical demonstration by the community nurse Good practice guidance is in packs Good Practice Points Clean, tidy and systematic work reduces risk of errors Good hygiene practice at all time never touch medication with your hands Seek advice if in doubt Never administer unless competent to do so Always read the label, read what is written not what you expect to be there