Federal Regulations - National Indian Health Board

Health Reform Implementation
-- Federal Regulations --
Presentation to the
NIHB Annual Consumer Conference
September 28, 2011
Doneg McDonough
Technical Advisor to the National Indian Health Board
(DMcDonough@NIHB.org)
2
Acronyms
AI/AN: American Indian and Alaska Native
I/T/U: Indian Health Service (IHS), Tribe and tribal organization, and urban Indian organization
HHS: Federal Department of Health and Human Services
CMS: Center for Medicare and Medicaid Services, HHS
CCIIO: Center for Consumer Information and Insurance Oversight at CMS
IRS: Internal Revenue Service, Department of Treasury
IHCIA: Indian Health Care Improvement Act
ACA: Patient Protection and Affordable Care Act, including reconciliation act modifications (Pub. L. 111-148 and Pub. L. 111-152)
3
Update on NIHB regulation work
At the moment -health reform = issuance of Federal regulations
From HHS, CMS, CCIIO, IHS, IRS
In reviewing and commenting on these Federal regulations, a primary focus is to ensure that American
Indians and Alaska Natives will have timely access to a full range of needed health care services from the
AI/AN’s providers of choice.
4
Our Pitch / Framework for Comments
Federal Trust Responsibility
Federal government has a unique obligation to AI/AN
There is a unique relationship between the Federal government and Tribes
In the ACA, Congress added a new mechanism to carry out the Federal Trust Responsibility
In addition to Indian health programs (I/T/U providers) supported by direct appropriations
In addition to Medicare, Medicaid and CHIP
ACA created subsidized insurance through Exchanges
5
Our Pitch / Framework for Comments
The Federal government as well as AI/AN and Tribes benefit if the Exchange plans provide a real option for AI/AN
Potential to bring additional resources for health care services to tribal communities… thereby furthering Trust Responsibility
Potential to lessen demands on Federal appropriation to IHS
Potential to expand health care services readily available to
AI/AN
Opportunity to access full AI/AN cost-sharing protections and general premium assistance if enroll through Exchange
But AI/AN need to know that they can access their providers of choice if they enroll in an Exchange plan
6
Our Pitch / Framework (continued)
There is tension in two elements of implementation
Obama Administration’s desire to provide maximum flexibility to States in implementing health reform
For Indian-specific provisions, efficient and effective implementation requires standardization
To carry-out the Congressional intent in the ACA, we need CMS to direct States on a limited set of issues, such as --
Require Exchange plans to offer to contract with I/T/U
Require Exchange plans to use Indian Addendum
7
Our Pitch / Framework (continued)
Two general provisions in the ACA support our request that Exchange plans be required to offer to
include I/T/U providers in Exchange plan networks
ACA section 1311(c)(1)(B): Network adequacy (“ensure a sufficient choice of providers”)
ACA section 1311(c)(1)(C): Essential community providers (“providers that serve predominantly lowincome, medically-underserved individuals”)
8
Our Pitch / Framework (continued)
Two Indian-specific provisions in the IHCIA (and
ACA) support our request that Exchange plans be
required to offer to include I/T/U providers in
Exchange plan networks
IHCIA section 206: Established a “right of recovery” for services rendered by I/T/U to AI/AN
IHCIA section 408: Established that “a Federal health care program must accept an [I/T/U] as a provider eligible to receive payment under the program for health care services furnished to [AI/AN]…
9
Our Pitch / Framework (continued)
Taken together, these provisions –
Establish a requirement (most directly through IHCIA section
408) that Exchange plans offer to contract with I/T/U
The requirement to “offer to contract” does not dictate the rate at which I/T/U are to be paid
– Section 408 establishes a floor of “payment… on the same basis as any other provider…”
– Section 206 provides leverage in rate negotiations with Exchange and other health plans that if an I/T/U is not included innetwork, the I/T/U can later demand payment at the higher of
(a) the I/T/U’s reasonable charges billed or (b) the highest rates paid to other providers
10
Our Pitch / Framework (finale)
Since Congress enacted provisions establishing that I/T/U have a right to participate in Exchange plan networks and to bill Exchange plans (whether in-network or not)
And, since there are a range of Indian-specific provisions in various Federal laws that Exchange plans are obligated to adhere to
It is in the interest of the Federal government (and
AI/AN) to --
Require Exchange plans to offer to contract with I/T/U
Require the use of a standard Indian Addendum to the
Exchange contracts
11
NIHB Regulatory Work
Twice a month, NIHB updates a report titled NIHB Regulation Review and Impact Analysis Report (RRIAR)
The purpose of the RRIAR is to identify and summarize key regulations issued by CMS pertaining to
Medicare, Medicaid, CHIP, and health reform that affect –
(a) American Indians and Alaska Natives and/or
(b) Indian Health Service, Indian Tribe and tribal organization, and urban Indian organization providers.
The RRIAR includes a summary of regulatory analyses prepared by NIHB and indicates the extent to which the recommendations made by NIHB were incorporated into any subsequent CMS actions.
The analyses and recommendations include those made by NIHB, by the Tribal Technical Advisory Group to
CMS (TTAG), and in some instances by individual Tribes.
The RRIAR consists of three tables –
Table A provides a status report on the RRIAR itself, listing the regulations included in the RRIAR to date, and the components of the analysis provided under each.
Table B lists key regulations issued by CMS, due dates for comments, a synopsis of the CMS action, and a summary of the analysis, if any, prepared by NIHB.
Table C identifies the recommendations made by NIHB pertaining to each regulation, if any, and evaluates the extent to which the recommendations made by NIHB were incorporated into subsequent
CMS actions.
12
Numerous regulations under review
13
Value of AI/AN Cost-Sharing Protection
(HHS Indian Offset)
Value of premium and cost-sharing assistance in an Exchange
$16,000
Comparison of Premium and Cost-Sharing Costs: Illustration of
Minimum Employer-Sponsored Coverage versus Exchange Coverage
(Family of 3 at 250% FPL)
Total: $15,098 Total: $15,456
$14,000
$12,000
$10,000
$8,000
$6,000
$4,000
$2,000
$0
$5,378
$4,349
$5,371
$3,630
$3,685
$8,141
Enrollee cost-sharing
Employee/enrollee premium
Employer/sponsor premium
Minimum Employer Qualifying
Coverage (ACA) Family (of 3) in Exchange at 250%
FPL (ACA)
14
Key Issues: (Tribal) employer responsibility
For larger employers subject to employer requirements under ACA (50+ FTE) –
Employers offering coverage pay into Exchange if
Plan does not cover 60% of expected costs (60% actuarial value), or
Employee’s share of premium is more than 9.5% of income and
Employee enrolls in plan through an Exchange
Employer pays $3,000 per employee enrolling through Exchange
Employers not offering coverage
Pay $2,000 to Exchange for every full-time employee beyond the first 30
15
Key Issues: Premiums and cost-sharing
Employees can leave employer coverage if “unaffordable”
Employer-Sponsored Coverage: Distribution of Premiums and Cost-
Sharing for Covered Services
(individual coverage; illustration)
Total: $5,789
Total: $5,536
$6,000
$740 / 13%
$5,000
$959 / 17%
Employee Cost-sharing
$1,972 / 36%
$4,000
Employee premium
$677 / 12%
Employer premium
$3,000
$4,090 / 71%
$2,000
$2,887 / 52%
$1,000
$0
Average Employer-Sponsored
Coverage (2009)
Minimum Employer Qualifying
Coverage (ACA)
16
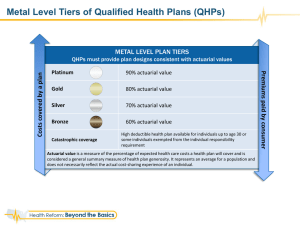
Key Issues: Premiums and cost-sharing
For coverage through an Exchange –
All plans must offer “essential benefits package” that is defined by Secretary
The plans offered in an Exchange vary by their actuarial value (i.e., the average share of health care costs that are paid by the plan)
– Bronze (60% actuarial value)
– Silver (70% actuarial value)
– Gold (80% actuarial value)
– Platinum (90% actuarial value)
17
Key Issues: Premiums and cost-sharing
• Government assistance is provided only to individuals/families that are enrolled “in the individual market offered through an exchange”
• Assistance available to persons in the exchange with incomes at or below 400% of FPL
• Premium assistance (Sec. 1401)
– Tax credits limit enrollee premium costs
– Enrollees pay the premium amount up to the value of the premium cap and the government pays the additional premium cost, if any
• Government premium assistance is tied to the cost of the second lowest silver plan in the exchange, or the plan selected, whichever is lower
– Tax credits are not available to individuals with employer-sponsored coverage
• Small business owners may be eligible to receive tax credits to offset 35% – 50% of their employee health insurance costs
• Cost-sharing reductions (Sec. 1402)
– First, the law imposes reduced out-of-pocket limits (specified in law) by income level
– Second, the law specifies the actuarial value of plans by income level, but the plans adjust the actual costsharing structure (i.e., deductibles, co-payments, co-insurance) to achieve the actuarial value
– Health plans will receive a payment from HHS to compensate for the average added costs (increased actuarial value) from the reduced enrollee cost-sharing
– AI/AN with income at or below 300% of FPL have no cost-sharing requirements for covered services
18
Key Issues: Premiums and cost-sharing
Enrollee premium protections
(annual)
Maximum Enrollee Premium Contributions in
Exchange (percent of income; 2010 poverty levels)
Income
Level
Up to 133%
133% - 150%
150% - 200%
200% - 250%
250% - 300%
300% - 400%
401+%
Initial
Premium % in Tier
2.0%
3.0%
4.0%
6.3%
8.1%
9.5% no limit
Final
Premium % in Tier
2.0%
4.0%
6.3%
8.1%
9.5%
9.5% no limit
Maximum Enrollee Premium Contributions in
Exchange (dollar amount; 2010 poverty levels)
Income
Level
133%
150%
200%
250%
300%
350%
Single
$432
$650
$1,365
$2,180
$3,087
$3,601
Family (of 3)
$731
$1,099
$2,307
$3,685
$5,218
$6,088
19
Key Issues: Premiums and cost-sharing
Enrollee cost-sharing protections
(annual)
Cost-Sharing Protections through an Exchange for Persons at or Below 400% of FPL
Income Level
Actuarial Value of Coverage Single Family
Maximum out-of-pocket (non-premium) costs*
0 - 100% 100%
101 - 150%
151 - 200%
201% - 250%
94%
87%
73%
251% - 400%
400% +
70%
Average out-of-pocket (non-premium) costs**
0 - 100%
101 - 150%
151 - 200%
201% - 250%
251% - 400% nominal nominal
$1,980 $3,960
$1,980 $3,960
$3,000 $6,000
$3,960 $7,920
$5,950 $11,900 minimal minimal
$282 $807
$612 $1,748
$1,271 $3,630
$1,412 $4,034
* Maximum out-of-pocket costs are 2011 figures which will be increased annually by the average increase in premiums nationally for the prior year.
** Average out-of-pocket costs calculation is extrapolated from the cost of the average employer-sponsored health plan offered in 2010 as reported by the
Kaiser Family Foundation.