Principles and Practices of Biosafety
advertisement

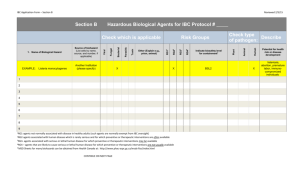
Principles and Practices of Biosafety Environmental Health and Safety San Diego State University Abbreviations BSC – Biosafety Cabinet BSL – Biosafety Level ABSL – Animal Biosafety Level BSO – Biosafety Officer BUA – Biological Use Authorization CA – California CDC – Center for Disease Control and Prevention DGR – Dangerous Goods Regulations DOT – Department of Transportation EHS – Environmental Health and Safety EPA – Environmental Protection Agency HMR – Hazardous Materials Regulations IACUC – Institutional Animal Care and Use Committee IATA – International Air Transport Association IBC – Institutional Biosafety Committee IRB – Institutional Review Board NIH – National Institute of Health OSHA – Occupational Health and Safety Administration PI – Principal Investigator PP – Physical Plant PPE – Personal Protective Equipment PS – Pubic Safety SD – San Diego USPS – U.S. Postal Service Introduction The management of biological hazards through the proper application of engineered containment and administrative controls is referred to as biosafety or biohazard control. Biosafety or biohazard control is a team effort involving the PI, research lab personnel, BSO, IBC, IRB, IACUC, EHS, PP and PS. Regulatory Requirements and Guidelines NIH Guidelines for Research Involving Recombinant DNA Molecules (April 2002) CDC/NIH Biosafety in Microbiological and Biomedical Laboratories (May 1999) CAL/OSHA Bloodborne Pathogen Standard CA Medical Waste Management Act DOT Transportation of Hazardous Materials SDSU Biosafety Requirements and Guidelines Policies established by the Institutional Biosafety Committee (IBC) that meet or exceed applicable guidelines and regulations for use of RG 2 and RG 3 biohazardous materials or agents as well as non-exempt NIH Recombinant DNA research. Policies established by Environmental Health and Safety (EHS) that meet or exceed applicable regulations and guidelines for minimizing bloodborne pathogen exposure and disposal of biohazardous wastes. Biohazardous Material Infectious microorganisms (bacteria, viruses, fungi, parasites, prions, rickettsiae, etc.) affecting humans and animals Diagnostic (clinical) specimens Recombinant DNA (viral vectors, gene therapy, cloning) Genetically Modified Microorganisms (transgenic plants and animals) Human and non-human primate cells, cell culture (primary and immortalized), tissues, blood (whole blood or any components) and body fluids Animal or plant cells, cell cultures, fluids, tissues or derived wastes which may contain pathogens Animals known to be reservoirs of zoonotic disease Institutional Biosafety Committee and Biological Use Authorization Biological Use Authorization (BUA) Application BSL 1, ABSL 1 and NIH-Exempt Reviewed and approved by BSO BSL 2 or 3, ABSL 2 or 3 and NIH- Non-exempt Reviewed and approved by IBC Currently, no facilities at SDSU meet the minimum criteria for BSL 4; thus this type of work is prohibited. Submission of New BUA New infectious agents New cell lines New vector system Enhanced replication or infectivity Expression of toxic products Partial genomes increased to more than two-thirds of whole genome New or altered procedures that pose increased risk (e.g., aerosol or other type of exposure) Work with non-human systems being changed into work with human system SDSU Biosafety Approval Institutional Biosafety Committee (IBC) Protocol Review Biological Use Authorization (BUA) with respect to containment level (biosafety level) Training Inspection Principal Investigator Develops specific protocols to ensure the safe use of biohazardous materials. Submits a BUA application and obtains approval from IBC prior to commencement of work. Complies with specific biosafety protocols, practices and procedures described in the biohazard control manual. Ensures that all laboratory staff are appropriately trained on biosafety. Reports any significant problems, violations of the policies, practices and procedures, or any significant research-related accidents and/or laboratory acquired infection to the BSO immediately. Laboratory Staff Comply with the specific biosafety protocols, practices and procedures described in the biohazard control manual. Report to the PI or the lab manager all problems, spills or violations in procedure immediately. Risk Group and Biosafety Level Classification of Infective Agents by Risk Group Pathogenicity Infectious Dose Mode of Transmission Host Range Availability of Effective Preventive Measures and Treatment Classification of Infective Agents by Risk Group Risk Group 1 Risk Group 2 Risk Group 3 Risk Group 4 Severity of Disease unlikely to cause human or animal disease can cause disease, unlikely to be serious, effective treatment and preventive measures available can cause serious disease, does not ordinarily spread from one person to another, effective treatment and preventive measures usually available, exposure route: inhalation (often) likely to cause serious or lethal disease, can be readily transmitted from one individual to another, effective treatment and preventive measures are not usually available, transmission: direct, indirect, inhalation Host Range human (healthy adult) and animals human (healthy adult) and animals human (healthy adult) and animals human (healthy adult) and animals Individual Risk low moderate (potential hazard) high high Community Risk low low low high Classification of Containment by Biosafety Levels Practices and Procedures Containment Equipment (Primary Barriers) Containment Facility (Secondary Barriers) Note: CDC/NIH has 4 biosafety level classifications currently in use. Each level is appropriate for: Operations Performed Routes of Transmission (ingestion, inoculation, inhalation, mucous membrane exposure) Laboratory Function Risk Group and Biosafety Level Classifications Not appropriate to use risk group or biosafety level when assessing toxins. Can be found in the American Biological Safety Association website: www.absa.org/resriskgroup Risk Groups and Biosafety Levels are not always the same! Bloodborne Pathogen Standard Introduction California Code of Regulations, Title 8, Sec 5193 Applies to all employees who could “reasonably anticipate” as a result of performing their job tasks contact with blood and other potentially infectious material (OPIM) i.e., body fluids, unfixed tissues or organs Limit occupational exposure to blood and OPIM which could result in transmission of bloodborne pathogens i.e., Hepatitis B virus (HBV), HIV Requires a written Exposure Control Plan Elements of an Exposure Control Plan Exposure Determination Method of Compliance HIV, HBV and HCV Research Laboratories Hepatitis B Vaccination and Post-Exposure Evaluation and Follow-Up Hazard Communication Record Keeping Evaluation of Exposure Incidents Sharps Injury Log Exposure Determination Exposure evaluation based upon the job description. Exposure evaluation based upon reasonably anticipated contact (skin, eye, mucous membrane, parenteral contact, etc.) with blood or other potentially infectious materials resulting from performing the assigned tasks. Method of Compliance Universal Precaution – treating all human blood and certain human body fluids as if infectious for bloodborne pathogens Engineering and Work Practice Controls Needleless system or needles/sharps with engineered sharps injury protection Needles and other sharps shall not be recapped, bent or broken Needles and other sharps shall be disposed in rigid, punctureproof, leak resistant and properly labeled sharps container Sharps container shall be closed immediately prior to removal or replacement to prevent spillage or protrusion of contents during handling or transport Specimens of blood or OPIM shall be placed in a closable, leakproof, properly labeled red bag prior to handling, collection or transport Personal Protective Clothing and Equipment Hepatitis B Vaccination and PostExposure Follow-Ups Hepatitis B vaccination shall be provided at no cost to employee who has a potential for becoming exposed to blood or OPIM. Post-exposure follow-ups shall be provided if an occupational exposure occurs. Hazard Communication 1. 2. Signs and Labels Signs shall be posted at the entrance to the work areas which shall bear: Name of infectious agent International symbol for biohazard in fluorescent orange-red Special requirements for entering the area Name and telephone number of lab director or other responsible person Warning labels shall be affixed to containers of infectious wastes, refrigerators and freezers containing blood or OPIM, or other containers used to store or transport blood or OPIM. Labels shall have the international symbol for biohazard in fluorescent orange-red Training Pathogenic Microbiology Bacterial Laboratory Acquired Infections 76% of exposures occurred in clinical labs; 6% in vaccine manufacturing facilities; 8% in research labs. Exposure modes: 60% inhalation, other exposure modes included ingestion (intentional, poor technique such as mouth pipetting, smoking and eating in the lab) and secondary transmission. Viral Laboratory Acquired Infections >70% associated with research labs; 32% of all viral LAIs associated with animals 18% of total were Hantavirus; of these, 8% were working with known infectious material or rodents - others thought they were working with uninfected rodents 16% were in clinical labs; rest were in production or field work Major exposure modes: inhalation, percutaneous (especially from animals) Rickettsial Laboratory Acquired Infections All rickettsial LAIs were associated with research laboratories 95% of overt infections were by Coxiella burnetii; remainder were Murine typhus All Q fever cases by inhalation; all infected staff worked with or were in close proximity to sheep Remaining cases were by percutaneous, inhalation, mucous membrane or unknown exposure modes Molecular Biology It’s a Matter of Perspective The investigators who submit IBC protocols want to perform their experiments safely. However, their perception of the risks involved will not necessarily be the same as that of a biosafety professional. Risk Assessment The following risk assessment will identify the biological containment system to be used: Properties of the donor organism Nature of the DNA sequences that will be transferred Properties of the recipient organism Properties of the environment Biological Expression System Most routine genetic engineering experiments can be performed safely in E. coli K12/pUC18 at BSL 1 provided the inserted foreign DNA sequences do not require a higher BSL. Donor Organism and Cloned DNA Insertion of well-characterized DNA sequences that are unlikely to be involved in pathogenicity may not require additional safety measures. In cases where these sequences are not characterized, a situation that is typically encountered when a library of genomic DNA of an organism is being established, a higher BSL will be required. Cloning of genes coding for proteins that have potential pharmacological activity such as toxins may therefore require higher BSL. Viral Vectors for Gene Transfer Although viral vectors used in gene therapy or gene transfer are replication-defective, they should be handled at the same BSL as the parent viral vector from which they are derived since the virus stocks may be contaminated with replication-competent viruses, which are generated by rare spontaneous recombination events in the complementing cell line. Transgenic and “Knock-Out” Animals Animals carrying foreign genetic information (transgenic animals) should be handled in the containment level appropriate to the characteristics of the products of the foreign genes. For each new line of transgenic animal, the routes by which the animals can be infected, the inoculum size required for infection, and the extent of the virus shedding by the infected animal must be determined. Animals with targeted deletions of specific genes (“knock-out” animals) do not generally present particular biological hazards. Human and Other Primate Cells and Tissues Human Source Material Blood and blood products Vaginal secretions Semen Amniotic fluid Unfixed tissues Cerebrospinal, synovial, pleural, pericardial and peritoneal fluids Cell cultures Saliva Urine Tears Sputum Feces Vomit Other excretions and secretions Second column not covered in Bloodborne Pathogen Standard, possibly not occupationally related. Human Source Material May transmit infectious agents Imperfect knowledge of infectious status Incubation period (asymptomatic) No test for every pathogen Most tissues and body fluids Bloodborne Pathogens (HBV, HCV, HIV, HTLV-1) Pathogens causing Malaria, Syphilis, Babesiosis, Brucellosis, Leptospirosis, Arboviral infections, Relapsing fever, Creutzfeldt-Jacob disease and viral hemorrhagic fever Cell Culture Risks Contaminating pathogenic agents natural (often zoonotic) or inadvertent ~20 LAIs from primary cultures in last 30 years e.g., Herpes B (CHV-1), prions Oncogenic potential could be oncogene or oncogenic agent e.g., HPV-18, MPMV genomes in HeLa cells Unexpected (adventitious) agents e.g., SIV, STLV, SV5 in primate cells, HHV-8 in BCBL-1 cells Hazardous chemicals added to culture medium Cell Culture under Bloodborne Pathogen Standard ABSA requested OSHA’s interpretation in 1994: Do human cell cultures fall under the Bloodborne Pathogen (BBP) Standard? Response: All primary human cell cultures (explants) and subsequent in vitro passages fall under the BBP Standard To be exempted from the BBP requirements, cell strains and lines must undergo testing and characterization (documented) for bloodborne pathogens (not just HBV, HCV and HIV) Cell Culture Safety Extend Universal/Standard Precautions to all human and animal cell cultures Consider working at BSL 2 (most work there already to protect the cell cultures) Handle all cultures in a biosafety cabinet If human origin and not demonstrated to be free of human bloodborne pathogens, adhere to requirements of the BBP Standard Wear PPE appropriate to human source material Summary Human Source Materials May be regulated Can be biohazardous Use Universal Precautions at all times Visible blood means increased risk Don’t consider “normal” source Human and Nonhuman Primate Cell Cultures Treat human cultures as possible biohazards Beware of non-human primate cells Beware of CNS, corneal, pituitary cells Some cells may be OK at BSL 1 Animals and Allergens Risk Assessment for Work with Research Animals Risks associated with the research agent used in the animal chemical, physical, biological Risks associated with the species of animal used zoonotic agents Risks associated with animal maintenance ergonomic factors, bites, scratches, allergens Risks Associated with the Agent Used Chemical agents carcinogens, mutagens toxic chemicals anesthetics Physical agents radiation heat sound Risks Associated with the Agent Used Potentially biohazardous agents deliberate use of an infectious agent in animals for research purposes maintenance of infected animal for duration of experiment sacrifice, necropsy and harvesting of agent or infected tissue Transmission of Biohazards During Work with Animals Airborne Release of infectious aerosols by animal by sneezing, coughing Release during nasal infection or aerosol challenge Aerosolization from bedding and excreta During surgical procedures During birthing Transmission of Biohazards During Work with Animals Direct Inoculation Needlesticks during injection/inoculation process Bites and scratches from infected animal Transmission of Biohazards During Work with Animals Direct exposure of mucous membranes (by splash or splatter) During surgical procedures During injection During necropsy Transmission of Biohazards During Work with Animals Indirect transmission and ingestion From contaminated hands or gloves to mouth Facial contamination directly from animal Transfer of parasites by animal handling Indirect transmission with eye or mucous membrane exposure Dust from bedding Splash during cage washing “Dirty” environment Risk Reduction: Containment of Infectious Agent Containment must include: Primary containment Enclosed filtered caging system Biosafety cabinets Safety equipment PPE Secondary containment The containment facility • Negative pressurization • Nonrecirculated air supply • Ventilation must consider wellbeing of animal Containment Caging Systems No Containment Open (standard) cage Some Containment Filter top cage (microisolator cage) Full Containment Fully enclosed in ventilated rack Containment Caging Systems Microisolator Cage works like a Petri dish open gaps around lid edge allow limited air exchange may lead to more labor intensive husbandry due to moisture and ammonia buildup Containment Caging Systems Individual cages sealed into rack with supplied air under negative pressure Both supply and exhaust usually HEPA filtered Ventilation must control humidity and buildup of ammonia Containment Caging Systems Can install cages in class III biosafety cabinet Cages are completely contained with glove port access Very motion-limiting Transfer in and out may be an issue Containment Caging Systems BioBubble (Ft. Collins, CO) makes softwall ventilated enclosures Can be containment or barrier style Large equipment can be surface-mounted in wall Special Animal Housing Situations Barrier colonies Special breeds - often immunocompromised, “fragile”, expensive (SCID-Hu, nude athymics) Transgenics - often even more fragile and expensive (knockouts, microinjected, combos) Specific pathogen-free (SPF) - bred and raised to be missing certain specific microorganisms Isolation colonies Extensive SPFs and defined flora animals Gnotobiotes (an entirely different animal!) Zoonoses Zoonotic disease: A disease of animals that can be transmitted under natural conditions and cause disease in humans Wild caught animals most hazardous Random source animals (e.g., from a pound) are also a risk Purpose bred animals pose least risk Some Animals and Their Zoonoses Animal Macaque monkeys Sheep White mouse Dogs, cats, skunks, raccoons, bats Cattle, NHP Cats Parrots, macaws Chickens Disease Herpes B virus Q fever Hantavirus Rabies Tuberculosis Toxoplasmosis Psittacosis Avian influenza Rodent Zoonoses Rat bite fever (Streptobacillus moniliformis, Spirillum minus) transmission: direct contact (bites) Lymphocytic choriomeningitis (LCM, a virus) transmission: inhalation Leptospirosis (Leptospira spp.) transmission: inhalation Others include ringworm (fungal), scabies (mites, an ectoparasite) Transmission of Zoonoses Enteric route (fecal/oral) Salmonella, Shigella, Campylobacter, Giardia, Toxoplasma, Cryptosporidium, Entamoeba, Hepatitis A Respiratory route Q fever, Chlamydia, Measles Skin contact Ringworm (Tinea), Measles, Monkeypox Control of Zoonoses Get information on species and agent Quarantine animals prior to use Use Engineering controls written SOPs and manuals Use PPE facility construction and secondary barriers Consider the need for containment caging Use Administrative controls additional protection for worker Practice good facility and personal hygiene Provide staff training Laboratory Acquired Allergies (LAA) Significant occupational disease Affects >30% of all personnel working with animals No minimum safe exposure levels to allergens have been established Animal allergens found in hair, dander, urine, saliva, serum fel-d-l cat allergen (in saliva and thus on skin) is one of the strongest allergens known for humans Sources of Exposure to LAA Hair and dander shed from animal Urine and feces dried in bedding Particulates shed from bedding material Animal saliva Routes of Exposure to LAA Inhalation of airborne allergens during cage changing during animal handling Skin or eye contact usually indirect by touching skin, eyes Percutaneous exposure animal bites (saliva) Risk Factors for Development of LAA Exposure to allergens duration frequency intensity Previous allergic conditions Other predisposing conditions illness Immunocompromised pets LAA: Exposure Control Engineering Controls enclosure dilution ventilation Administrative Controls reduce time with animals reduce density of animals housekeeping practices Personal Protective Equipment respirators and clothing Medical Surveillance Disinfection Why Disinfect? To reduce or eliminate exposure risk Biohazard waste disposal Spill cleanup Routine surface decontamination To eliminate contamination risk Preparation of microbiological media and supplies Preparation of work area for cleanliness-critical tasks Resistance to Disinfectants Prions Bacterial spores Coccidia (Cryptosporidium) Mycobacterium Nonlipid viruses (Hep A, Polio) Fungi Rickettsiae, Chlamydiae Vegetative bacteria Lipid-containing viruses Classes of Disinfectants Chlorine Iodine Alcohol Phenolics Quaternary Ammonium Glutaraldehyde Hydrogen peroxide Factors Influencing Efficacy Surface/Topography – uneven, cracked or pitted surfaces especially wooden surfaces can hide microorganisms and are difficult to disinfect Temperature - elevated temperatures may enhance germicidal action but also evaporation rate Relative Humidity – many disinfectants have optimal relative humidity range for maximum effectiveness Water Hardness – some disinfectants may be less effective when diluted in hard water Organic Load Blood, sputum, milk, bedding, feed, manure Proteins physically protect and stabilize many microorganisms Adverse effect on action of many disinfectants Concentration In most cases, the higher the concentration, the more rapid the kill Consider potential damage to surfaces or tissues Reducing concentration to avoid damage will require additional contact time Ultimately, disinfectant will no longer be active enough to be useful Contact Time Disinfectants should be effective with a short contact time Manufacturer’s recommended contact time may be unrealistic under in-use condition Contact time may depend on the method of application For surface applications, loss by evaporation may require frequent applications to achieve contact time Some Other Factors Dirt, grease and oils – all can protect the organism and will repel water based disinfectants Types of microbes present – spores, vegetative cells, viruses Dried spills (from media, buffers) can protect microorganisms from contact with the disinfectant pH Age of the product/solution Method of application (spray vs. wipe) Rate of application Storage condition Medical Waste Disposal (Biohazardous and Sharps Wastes) Who Regulates Medical Waste? Federal EPA (40 CFR part 60.51c) DOT (49 CFR Part 173.134) OSHA (29 CFR Part 1920.1030b) USPS (39 CFR 111.1) State CA Health and Safety Code Local SD Code of Regulatory Ordinance Medical Waste …biohazardous waste and/or sharps waste that is produced or generated as a result of diagnosis, treatment or immunization of human beings or animals; research pertaining thereto; production or testing of biologicals or removal of regulated waste from a trauma scene. Forms of Medical Waste Solid Labware (flasks, tubes, plates, bottle, vials) Pipettes (could also be sharps) Lab waste (stocks, specimens, cultures, swabs, vaccines) Gloves, apparel, wipes Liquid Aspirates, culture fluids, rinses, washes Sera, body fluids Sharps Anything with a point or edge capable of piercing or cutting Medical Waste Does Not Include: Waste generated in food processing Urine, feces, saliva, sputum, nasal secretions, sweat, tears, or vomitus, unless it contains fluid blood Medical solid wastes i.e., paper towels or empty specimen containers that are not biohazardous, bandages/dressings containing dried blood Hazardous waste, radioactive waste, household waste Waste generated on agricultural or livestock practices on a farm or ranch Biohazardous Waste Laboratory Wastes Human or animal specimen cultures Cultures and stocks of infectious agents Wastes from production of biologicals, live and attenuated vaccines, culture dishes and devices Pharmaceuticals Human surgery specimens or tissues, including those fixed in fixatives Animal parts, tissues, fluids, or carcasses Wastes containing recognizable fluid blood or blood products, containers with fluid blood, blood from animals Wastes contaminated or containing chemotherapeutic agents Sharps Waste … means any device having acute rigid corners, edges, or protuberances capable of cutting or piercing. Needles, needles with syringes, contaminated syringes, blades, needles with attached tubing Broken glass items i.e., Pasteur pipettes, blood vials contaminated with biohazardous waste Mixed Waste … means mixtures of medical and nonmedical waste. Mixed waste is medical waste, except for all of the following: “Mixed Waste Hierarchy” Biohazard Bag …means a disposable red bag that is impervious to moisture and has a strength sufficient to preclude ripping, tearing, or bursting under normal conditions of usage and handling of the waste-filled bag. Containment and Storage Biohazardous Waste Must be segregated from other types of wastes Must be contained in “biohazard bags” Bags must be red. Bags must be labeled either with the word “Biohazardous” or with the biohazard symbol and the word “Biohazard”. Bags must also be labeled with the generator’s name, address and phone number. Bags must be securely tied to prevent leakage or expulsion of contents. Bags must be placed in a rigid container for storage, handling and transport. Containers Containers shall be leak resistant, have tight-fitting covers, kept clean and in good repair. Containers may be of any color and shall be labeled with the word “Biohazardous” or with the biohazard symbol and the word “Biohazard” on the lid and on the sides so as to be visible on any lateral direction. Reusable containers shall be washed and decontaminated unless protected from contamination by disposable liners or bags. Reusable containers shall be washed to remove visible soil and decontaminated by: Exposure to hot water (180°F) for 15 secs. Exposure to the following sanitizer for 3 mins. Hypochlorite soln. (500 ppm avail. Chlorine) Phenolic soln. (500 ppm active agent) Iodoform soln. (100 ppm avail. Iodine) Quaternary ammonium soln. (400 ppm active agent) Sharps Container …means a rigid puncture resistant container that, when sealed, is leak resistant and cannot be reopened without great difficulty. Containment and Storage Sharps Waste Must be segregated from other types of wastes. Must be contained in “sharps container”. Tightly close or tape closed the lid of a full sharps container ready for disposal. Store sharps container ready for disposal for not more than 7 days. Label sharps container with the word “Sharps Waste” or the biohazard symbol and the word “Biohazard”. Must also be labeled with the generator’s name, address and phone number that is legible and easily visible on the outside of the container. Disposal Take biohazard bag and sharps container to designated Accumulation Sites: Life Science, Room 14 Student Health Service, outside shed Generators at other locations may call EHS at (619) 594-6778 for biohazard waste pick-ups A biowaste vendor will collect biohazard bag and sharps container for disposal on a weekly basis from Life Science and Student Health Services. Biohazardous and sharps wastes will be autoclaved while animal carcasses will be incinerated. Solid Medical Waste Collection Must be rigid, puncture-proof, leak-proof Not acceptable in CA Labels have to be affixed on all 4 sides of the container. Sharps Waste Collection Sharps containers <7 gal. should not be on the floor. Lids have to be difficult to open. Labels have to be affixed on all 4 sides of the container. What’s Wrong with these Pictures? Left: Sharps sticking out of Sharps Waste container. Right: Sharps Waste container past full line. No generator label. What’s Wrong with these Pictures? Left: Bottle not labeled. Right: Cardboard box is not allowed for liquid waste. No labels. No lid. What’s Wrong with these Pictures? Left and Right: Cardboard box is not an appropriate Sharps Waste container. No labels. No lids. What’s Wrong with these Pictures? Left: Red bag should be inside the secondary container. Cardboard box is not an acceptable secondary container. Right: Bag must be red. Secondary container does not have to be red. No biohazard label. Red bag on floor ready for disposal must be transported to the accumulation site immediately. What’s Wrong with these Pictures? Left: Do not fill red bags completely. Replace more often. Right: No biohazard label. Red bag on floor ready for disposal must be transported to the accumulation site immediately. What’s Wrong with these Pictures? Left: Do not deface container. Incorrect label placed on container (need generator label). Right: Red bag must be transported in a secure secondary container to the accumulation site. Red bag must have biohazard label and generator label. What’s Wrong with these Pictures? Left: Proper Sharps Waste container not used. No generator label. Right: Generator label should be on the outside of the red bag. Secondary container needs biohazard label on all visible sides including top. Use appropriately sized red bag for secondary container. What’s Wrong with these Pictures? Left: Incorrect label placed on container (need generator label). Keep lid closed when not in use. Right: No lid. Use appropriately sized red bag for secondary container. Secondary container needs biohazard label on all visible sides including top. Containment Equipment and Facilities Biocontainment The principle of holding or being capable of holding or including within a fixed limit or area Preventing the unintentional release of biological agents through a combination of laboratory practices, containment equipment (primary barrier) and laboratory facility design (secondary barrier) Primary Barrier Primary barriers contain the agent at the source Equipment/Engineering Control Biological safety cabinet, fumehood, glove box, animal housing, centrifuge, fermenter Secondary Barrier Secondary barrier is the structure surrounding the primary barrier Facility/Engineering Control Rooms, building Types of Facilities Basic laboratory Containment laboratory Primary Barriers - Equipment Personnel Protection Any aerosol generated within the cabinet is contained and kept away from the researcher Product Protection Air within the work space of the cabinet has been filtered so that is is virtually free of airborne particles and organisms; thus protecting the work from outside contamination Environmental Protection Aerosols generated within the unit are removed from the air before the air is discharged Ventilation Equipment Classes and Types Chemical Fume Hood 100 fpm face velocity Offer only personnel protection Always exhaust air to the outside Do not offer protection to the product or the environment, as there is no filtration of intake and exhaust air (Sometimes air cleaning treatment is added to the exhaust.) Do draw contaminants in the laboratory air directly over the product being worked on Used for work with chemical hazards Any Comments? Fumehood - keep hood clean, sash should be closed when hood is not in use, equipment should be 9” from sash Clean Bench / Laminar Flow Hoods Provide product protection only Product protection is provided by creating a unidirectional airflow generated through a HEPA filter Discharge air goes directly into workroom Applications – Any application where the product is not hazardous but must be kept contaminant free – Preparation of non-hazardous intravenous mixtures and media – Particulate free assembly of sterile equipment and electronic devices Eliminate Clean Bench in containment laboratory Biological Safety Cabinets Designed to contain biological hazards Inward airflow for personnel protection HEPA filtered exhaust air for environmental protection Supply air HEPA filter for product protection (except Class I) Separated into Classes and Types – Class I – Class II • Type A1, A2 • Type B1, B2 – Class III Microbiological studies, cell cultures, pharmaceutical research and procedures… Class I Cabinet 75 fpm face velocity Provides personnel and environmental protection No product protection Requires an exhaust blower to pull the air through - usually to the outdoors Applications – Housing centrifuges, fermenters – Cage dumping in an animal lab – Aerating cultures Class II Cabinets Ventilated cabinet Provides personnel, product, and environmental protection Open front with inward airflow for personnel protection Downward HEPA filtered laminar airflow for product protection HEPA filtered exhaust air for environmental protection Any Comments? BSC - remove unnecessary objects, keep grill at front of cabinet unobstructed Primary Barriers Personnel Chemical Fumehood Product Environment x Laminar Flowhood x Class I Biosafety Cabinet x x Class II Biosafety Cabinet x x x Class III Biosafety Cabinet x x x Isolators x x x Types of Biosafety Cabinets NSF/ANSI Standard 49 – 2002 Type Face velocity (lfpm) Airflow Pattern Radionuclides/ Toxic Chemicals Biosafety Level(s) Class I 75 In at front; rear and top through HEPA filter No 2, 3 No Class II Type A1 75 70% recirculated through HEPA; exhaust through HEPA No 2, 3 Yes Class II Type A2 100 30% recirculated through HEPA; exhaust via HEPA and hard ducted Yes (Low levels/volatility) 2, 3 Yes Class II Type B1 100 No recirculation; total exhaust via HEPA and hard ducted Yes 2, 3 Yes Class II Type B2 100 Yes 2, 3 Yes Class III NA Yes 3, 4 Yes Same as B1, but plena under negative pressure to room and exhaust air is ducted Supply air inlets and exhaust through 2 HEPA filters Product Protection Biological Safety Cabinet Certification First Certification Annually When moved When filter is changed When repaired or modified Note: Certification is paid by the researcher, not EHS Other Primary BarriersEngineering Control Gasketed blenders, homogenizers Cotton plugs, filters for flasks in shakers Filtered pipette tips HEPA and hydrophobic vacuum line filters Plasticware substituted for glassware Gas burners with shield, microincinerator Centrifuges Interlock, solid cover, safety buckets, O-rings Secondary Barrier- Facilities Laboratory Biosafety Level 2 Lockable doors (a must for restricted agents) Sink Bench tops impervious and easily cleaned Biological safety cabinet (if applicable) Eyewash Inward airflow (desirable) Biosafety Practices and Procedures Hierarchy of Controls Administrative Control Engineering Control Work Practices Personal Protective Clothing or Equipment Administrative Controls Substitution Authorization/Approval Written biosafety procedures required for the experimental procedures and equipment including inventory of biological agents or materials Laboratory personnel biosafety training Medical Surveillance (BSL 2 and above) Health history Medical screening Immunization Serum storage Post-exposure prophylaxis Engineering Controls Biological safety cabinets, glove boxes Animal containment caging systems Safety equipment (filtered or sealed equipment) Ventilation system Containment facilities Personal Protective Clothing and Equipment Provides barrier against skin, mucous membrane or respiratory exposure to infectious agents during procedures Prevent spread of contamination Does not eliminate the hazard Integrity wanes with use (i.e., change gloves frequently) BSL 1: Work Practices and Procedures Applications Non-infectious agent and tissue culture, media preparation Prevent Cross Contamination Keep cultures covered Flame instruments and containers Use sterile media and equipment Keep hands or face away from cultures BSL 1: Work Practices and Procedures Biosafety Procedures Work with agents may be conducted on open bench Wash hands often No mouth pipetting No eating or drinking in lab Minimize aerosol generation Decontaminate work surfaces Wear applicable PPE BSL 2: Work Practices and Procedures Increasing emphasis on safety procedures and practices Increasing need for staff training Increasing need for competent supervision Biohazard sign posted at entry door Biohazard labels affixed on regulated waste containers Use of personal protective equipment as a barrier to exposure: lab coat, gloves, eye and face protection Some work on open bench allowed BSL 2: Work Practices and Procedures Aerosol generating procedures performed in a biosafety cabinet: Homogenizing Vortexing Vigorous mixing Pipetting infectious liquids Sonication Pouring If breach occurs: Evacuate lab, post spill sign With appropriate PPE and disinfectant, decontaminate centrifuge, buckets, other items or areas Correct Use of Biosafety Cabinets Start Up Turn off ultraviolet light (if so equipped) as soon as you enter the room. Turn on all blowers and BSC illumination lights. Allow five minutes of operation to purge system; check flow alarm system audio and visual alarm function (if so equipped). Decontaminate readily accessible interior surfaces and items with a disinfectant (appropriate for the agents or suspected agents present) before loading and wait at least 10 minutes prior to start of work. Correct Use of Biosafety Cabinets During Use Load supplies prior to work. Do not overload cabinet. Separate clean and dirty side. Work in center of work area. Do not block front or rear grills. Minimize disruption of airflow (turbulence). Clean up spill promptly. Discard waste within the cabinet. Correct Use of Biosafety Cabinets Shut Down Decontaminate and remove all items from interior work area. Decontaminate readily accessible interior surfaces with a disinfectant appropriate for the agents or suspected agents present. Turn on ultraviolet light (if so equipped). Allow five minutes of operation to purge system. Then wait at least 10 minutes. Turn off BSC blower. Correct Use of Biosafety Cabinets Moving/Installation BSCs must be decontaminated prior to moving. In order to ensure filter integrity, the equipment must be recertified after the BSC is installed at its final new location. Arrangements need to be made well in advance in order for contractors to meet your schedule. The PI is responsible for contacting the contractor or to schedule this work. Decontamination Decontamination is usually performed by certified professionals. Certification All BSCs that are used for handling biohazardous materials must be recertified annually. SDSU has contracted with a specific contractor to provide a consistent level of certification and maintenance service. Contact EHS at (619) 594-6778 to obtain contractor information. Correct Use of Biosafety Cabinets – Open Flames DO NOT use Bunsen burners or open flames Fire hazard Can damage HEPA filter Interferes with proper air flow Microincinerator preferred Burner with pilot light not a good alternative Open flames react with disinfectants (flammables) Safe Use of Centrifuge Use sealed tubes, rotors, and safety cups/buckets that are sealed with O-rings Inspect tubes, O-rings and rotors for wear, and buckets for cracks, chips, erosion, etc. Do not use aluminum foil to cap centrifuge tubes Clean and maintain gaskets and O-rings Change O-rings if compromised Load/unload centrifuge tubes, rotors and accessories in BSC Small, low speed centrifuges may be placed in a BSC; however, high speed centrifuges pose additional hazards Do not overfill tubes Balance buckets, tubes and rotors properly before centrifugation Wait 5 minutes (or 30 mins. for high speed centrifuge) after each run before opening Do not decant or pour off supernatant. Use a vacuum system with appropriate in-line reservoirs and filters Safe Use of Blenders Avoid use of glass blender jars, unless covered with polypropylene jar Place disinfectant-moistened towel over the top of the blender during use Before opening the blender jar, allow the unit to rest at least 1 minute for aerosols to settle and then open in a BSC Decontaminate promptly after use Minimizing Aerosols Use careful pipetting practices Avoid drops onto hard surfaces Wipe up spills promptly with appropriate disinfectant For ejection of liquid from micropipette No blowout No pressure ejection Use wall contact Use capped tubes when mixing, blending, or vortexing Pour liquids carefully Avoid bubbles Careful Pipetting Techniques Never blow out last drop in pipette Use pipetting aids with filters Never mix by suction and expulsion (mix by sonication) Discharge liquid down side of container, using tip-to-wall contact Deliver as close as possible to contents Work over plastic-backed absorbent matting (ensure it doesn’t slide forward or backward blocking air grill) Use Extreme Care with Sharps Use sharps if only absolutely required as part of a process Percutaneous exposure risk Employ safe work practices Utilize safe sharp devices Aerosol exposure risk Use biosafety cabinet for removal of air from needle Use mechanical methods for needle removal Never bend, recap or manipulate sharps by hand Keep hands away from needle Vacuum System Protection In-line filter and disinfectant in collection and overflow flasks Signs and Labels Biohazard Signs Completely filled out biohazard sign must be displayed at entrances to laboratories where biohazards are present and tissue culture rooms Features fluorescent orange-red sign with lettering “biohazard” and the international biohazard symbol in contrasting color, name of biohazardous agent or material, special entry requirement and PI and BSO contact number Available free of charge from EHS, call (619) 594-2865 Biohazard Label Must be attached to containers of biohazards or biohazardous waste containers. Features fluorescent orange-red label with lettering “biohazard” and the international biohazard symbol in contrasting color. Red bags and sharps containers must also have the generator address label affixed prior to use: San Diego State University 5500 Campanile Drive San Diego, CA 92182 (619) 594-6778 Laboratory Moves It is important that the laboratory is safe: For custodians to clean For contractors to work in For the next group of laboratory personnel to occupy Disposal and Decontamination of Biohazardous Waste In preparation for moving, observe the following guidelines: Label ALL biohazardous waste red bags and sharps container Dispose of all biohazardous waste red bags and sharps containers at approved accumulation sites EHS will not pick-up biohazardous waste except in unusual situations Chemically disinfect biohazardous waste Autoclave liquid biohazardous waste and dispose of down the drain Moving the Biosafety Cabinet Disinfect all BSC work surfaces prior to moving the BSC to a new facility. BSCs used for work with pathogenic organisms may require paraformaldehyde decontamination before being moved. Each BSC must be recertified for correct airflow and filter integrity after it has been moved and placed in its final location. Moving or Disposing of Refrigeration Units Clear all materials stored inside the refrigeration units. Disinfect all refrigeration units prior to removal or disposal. Obtain clearance notification from EHS prior to removal or disposal of refrigeration units. Shipment and Transportation To Whom are the Shipping and Transportation Regulations Applicable? Under IATA, DGR apply to anyone who handles, offers for transport, transports dangerous goods or causes dangerous goods to be transported. Under DOT, HMR apply to each person who performs, or causes to be performed, functions related to the transportation of hazardous materials such as determination of, and compliance with, basic conditions for offering; filling packages; marking and labeling packages; preparing shipping papers; handling, loading, securing and segregating packages within a transport vehicle, freight or cargo hold; and transporting hazardous materials. Emergency Response to Biological Incidents Response to Biological Spills in the Laboratory (Intentional or Accidental) Exposure Management For splash to eyes, mucous membranes, or broken area of the skin Irrigate eyes with clean water, saline or sterile irrigants Flush splashes to mouth, nose, and broken area of skin with water Exposure Management For needlesticks or cuts with human blood, fluids, infectious agents or antibiotic resistant organism Flush needlesticks and cuts with soap and water Get medical evaluation ASAP Inform PI, BSO and health professional (required mandatory reporting of incident) Public Health Service has recommendations for post-exposure follow-up Spill Clean-Up You can clean-up a biological spill if: You are aware of the hazards and clean-up procedures (training required) There is no potential for personal or environmental damage The appropriate spill clean-up equipment is available One or two people can clean-up the spill thoroughly in less than an hour Note: Spill incident still needs to be reported to BSO/EHS. If spill is in gallons or liters, call BSO/EHS. Biological Spill Clean-Up KitBasic Nitrile gloves (double gloving), splash goggles, shoe covers Small disposable broom with dustpan, tongs or forceps (for picking up sharps) Paper towels or other absorbent in the lab Sharps container and/or biohazard waste bags Disinfectant agent suitable for the agents in the lab Spill Clean-Up for BSL 1-2 If there is a spill inside the biosafety cabinet: Keep the BSC running during spill and clean-up to contain aerosol. Place absorbent paper on spill and soak with disinfectant. Allow 20 minutes of contact time. Wipe up spill, working from the edges to the center. Clean spill areas with fresh paper towels soaked in disinfectant. Disinfect the BSC interior and any other equipment in the BSC with disinfectant. Discard contaminated disposable materials using appropriate biohazardous waste disposal procedures. Place contaminated reusable items in biohazard bags or autoclavable pans before autoclaving. Run BSC 10 minutes after clean-up before resuming work or turning BSC off. Note: If you are working in a BSC and the power went off in the room or the BSC fan stops blowing, IMMEDIATELY LEAVE THE ROOM. Spill Clean-Up for BSL 1-2 If the spill is in the laboratory but outside the biosafety cabinet Call the BSO if the material is RG 2 or greater. Clear area of all personnel. Wait at least 30 minutes for aerosol to settle before entering spill area. Remove any contaminated clothing and place in biohazard bag to be autoclaved. Put on disposable gown, safety glasses and gloves. Initiate cleanup with disinfectant as follows: Place dry paper towels on spill then layer a second set of disinfectant soaked paper towels over the spill. Encircle the spill with additional disinfectant being careful to minimize aerosolization while assuring adequate contact. Allow at least a minimum of 20 minutes contact time to ensure germicid action of disinfectant. Wipe up spill, working from the edges to the cente Clean spill areas with fresh paper towels soaked in disinfectant. Decontaminate all items within the spill area. Discard contaminated disposable materials using appropriate biohazardous waste disposal procedures. Spill Clean-Up for BSL 1-2 If the spill is outside the laboratory, in transit: To prevent a spill, transport labeled biohazardous material in an unbreakable, well-sealed primary container placed inside of a second unbreakable, lidded container (cooler, plastic pan or pail). Should a spill occur in a public area, do not attempt to clean it up without appropriate PPE. Secure the area, keeping all people clear of the spill. Call the BSO to assist in the clean-up. Stand by during spill response and cleanup activity to provide information and assistance. Biosecurity Biosecurity vs. Biosafety Biosecurity refers to ensuring the security of biological materials to prevent theft, illicit use or release. Biosafety focuses on reducing exposure to and release of biological materials. Integrating biosecurity and biosafety programs is important for work with select agents. Inspection Inspection Elements Laboratory Identification Containment Facility/Equipment Work Practices Hazard Communication Biohazardous Waste Handling Laboratory Personnel