Mental Health and Illness
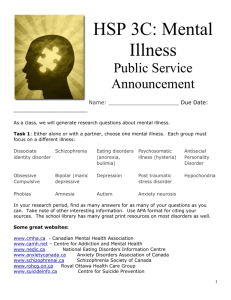
advertisement
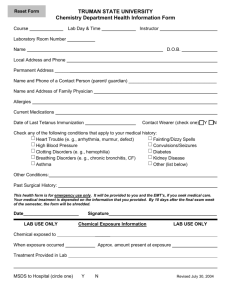
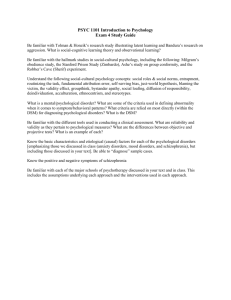
Mental Health and Illness Overview of Approaches, Definitions, Perspectives 1 Continuous or discrete? Continuous model: Mental Health Mental Illness +++++++++++++++++++++++++++++ Healthy>>>>Adjustment reaction>>>>Neurosis>>>>Psychosis We all have differing degrees of mental health at different times in our lives. Most people aren’t at the extremes but fall somewhere in the middle. Anyone can become mentally ill, given the right circumstances. 2 Discrete model Some people are mentally healthy; others have specific mental disorders. “Decision trees” can distinguish who has a specific mental disease and who doesn’t. Mentally Healthy Mentally Ill 3 What is mental health? In our society, a mentally healthy person: Has self-esteem, self-acceptance Is realizing potential Is able to maintain fulfilling relationships Has a sense of psychological well-being Has sense of autonomy Has sense of competence, mastery, purpose However, other cultures may have different ideas about what mental health is. 4 Who has mental health? We all fall short to some extent. Therefore, advocates of mental health believe that a broad range of mental health services should be available to general population, not just seriously mentally ill. They believe that prevention and education, as well as treatment, are important. 5 What is mental illness? Is it a disease, like diabetes or smallpox? Is it a form of deviant behavior—like being rebellious, choosing to dress differently, being extremely religious, being extremely creative? 6 The Medical Model and Concepts of Disease “When distress or inappropriate behavior is thought to be a consequence of a bodily dysfunction, it is called a ‘disease.’” Mechanic, p. 14. To diagnose diseases in physical medicine, doctors perform laboratory tests, do body imaging, take medical history, do physical examinations. Once disease is diagnosed, doctor generally knows: Its cause How disease is likely to run its course 7 What most appropriate treatment is Are mental illnesses like other diseases? Mental illnesses cannot be confirmed by objective laboratory tests or body imaging. Diagnosis in mental illness does not lead to an understanding of cause, of the course of the illness, or of the most appropriate treatment. Some (e.g., Thomas Szasz) have argued that mental illnesses are not diseases because of the above problems. 8 Perspective of DSM Mental disorders represent a “clinically significant behavioral or psychological syndrome or pattern that occurs in an individual and that is associated with present distress (e.g., a painful symptom) or disability.” DSM tries to make psychiatric diagnoses more similar to medical diagnoses. Sees psychiatric symptoms as indicators of disease, not deviance. 9 DSM Strength: useful tool for practitioners, insurers, courts, agencies, since it allows for communication, offers consistent set of definitions. Limitation: However, it is purely descriptive, doesn’t indicate causes, offers limited information about expected course of the disease, doesn’t suggest appropriate treatment. 10 Major DSM-IV categories Disorders usually first diagnosed in infancy, childhood, or adolescence Delirium, dementia, amnestic, and other cognitive disorders Mental disorders due to a general medical condition not elsewhere classified Substance-related disorders Schizophrenia and other psychotic disorders Mood disorders Anxiety disorders Somatoform disorders Factitious disorders Dissociative disorders Sexual and gender identity disorders Eating disorders Sleep disorders Impulse-control disorders not elsewhere classified Adjustment disorders Personality disorders Other conditions that may be the focus of clinical attention 11 Sociological perspective Mental disorders are type of deviant behavior, not a disease process. Those who are seen as mentally ill are those who violate social rules, don’t behave appropriately. Individuals who become labeled as mentally ill are those not powerful enough to resist such labels. 12 Mental illness as deviant behavior Researchers who view mental illness as deviant behavior usually study processes and rules used to define mental illness rather than symptoms in individuals. Szasz (1963, 1984): Mental illness is not a disease, since there are no physical lesions that indicate it. Calling people mentally ill denies concepts of free will and responsibility for one’s actions. 13 Bad or mad? Why do we call some deviant behaviors “bad” and some “mad”? If there is self-interest involved, we are more likely to call the behavior “bad.” Same behavior, different context, can be assigned different labels—e.g., poor person who shoplifts is more likely to be considered “bad,” whereas a very wealthy person who shoplifts is likely to be seen as “sick.” Why? 14 Assumptions behind “bad” or “mad” Ambivalent ideas: Social and behavioral sciences are deterministic, assuming that behavior is determined—by prior events, social forces, biology At the same time, we assume that individuals can distinguish between right and wrong and have “free will” and thus can be held responsible for their actions. 15 Definitions and labeling can be problematic Not so much in voluntary treatment—if an individual seeks help from a mental health professional, then common goals can be identified and pursued. If an individual is forced into treatment, then many ethical dilemmas can arise. 16 How can mental illness be measured? Some researchers (sociologists, public health specialists, social workers) prefer to study how mental illness develops in communities, rather than its manifestations in those who are being treated for mental illness. 17 Terms useful in assessment of mental illness in communities: Epidemiology: study of how illness is distributed in a population, rates of disease, who appears to be susceptible, in an attempt to identify causes and discover interventions (example of work of John Snow on cholera in London in 1854) Morbidity: prevalence of diseases in a population Comorbidity: occurrence of more than one disease in the same individual 18 Terms (continued): Prevalence: How often the disease occurs Point prevalence: percentage of population affected with an illness at any given point in time Lifetime prevalence: percentage of population ever affected with an illness Incidence: rate at which new cases appear within a given time period 19 Epidemiological studies of mental illness 1st in USA: Epidemiologic Catchment Area (ECA), 1981 2nd in USA: National Comorbidity Study (NCS) 1990’s Also a number of studies of prevalence and types of mental illness in other cultures 20 Cross-cultural studies What is normal in one culture is not necessarily normal in another Therefore, measurement in cross-cultural studies is a real problem This holds true in cross-national studies and in studies of diverse ethnic groups within nations 21 What causes mental illness? No one really knows. Research so far is inconclusive. Research is being carried out from diverse perspectives: Psychological Biological Sociological 22 Biological, developmental, or social? Since human beings are both biological and social animals, it doesn’t make sense to argue about what causes mental illness. Causes are complex, involving some combination of biological vulnerability, environmental conditions, social stressors, social network and supports, psychological orientations, and learned behavior. 23 Possible psychological/ developmental causation: Psychological research into causes of mental illness examines individual personality (early development, cognitive styles, personal identity) Perspectives Psychoanalytical—early developmental influences, such as child abuse/neglect, quality of parenting Cognitive-behavioral/behavioral—how ways of thinking affect behavior, social learning Phenomenological/existential—focus on choice, responsibility, meaning Family dynamics—focus on family roles, communication patterns 24 Possible biological causation: Factors examined by researchers: Genetics Neurochemisty Viral causation 25 Possible environmental/social causation: Factors examined by researchers: Chronic strains in the environment Poverty Poor living conditions Dangerous neighborhoods Overwhelming role responsibilities Negative life events—stress and coping Natural disasters Unemployment Adjusting to new environments and roles 26 Environmental/social causation (continued): Another factor examined by researchers: Labeling Social control—how mental health diagnosis and treatment acts as an agent of social control Relationship between social attitudes toward mental illness and the course of mental disorders—effects of stigma, discrimination, and social exclusion 27 Environmental/social causation (continued): Collective mobilization Notion that society produces disabilities by how it: Defines persons with impairments Limits access to community facilities and employment Discriminates against them Impairments can become either a major aspect or minor aspect of a person’s identity, depending on how society and government respond to persons with impairments 28 Disease or problem in living? Some problematic behaviors are given the status of disease in DSM: Alcohol abuse and dependence Drug abuse Conduct disorders in children They may not really fit into the disease model It may be more valid to consider them as problems in living 29 Public definitions of mental illness Most people who seek treatment for mental disorders do so because they feel distressed. Some people, however, feel they do not need help but are identified by others (e.g., family, friends, police, schools, employers). Evaluators have to make difficult judgments in such cases. 30 Role of values Values of evaluator can influence judgments about individuals being evaluated. Evaluators’ notions of what is appropriate behavior are shaped by their culture and social context. If an evaluator accepts the worldview of his/her society, then people with different worldviews can be seen as deviant—mad or bad. 31 Value of the disease model Disease model attempts to be objective and universal, avoiding value judgments about behaviors. Psychiatrists attempt to separate out symptoms from cultural content (e.g., schizophrenia). 32 DSM Decision Tree: Mood Disorders 33