What are Isolation Precautions? - Vanderbilt University Medical Center
advertisement

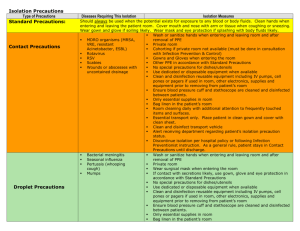
Isolation Precautions: Guidelines for Perioperative Services Previous Slide Next Slide What are Isolation Precautions? Practices that prevent transmission of certain diseases from patients to staff, and from staff to other patients Type of isolation precautions is determined by how a disease is transmitted (passed) Isolation Precautions are done in addition to Standard Precautions and include: Strict adherence to hand hygiene Personal protective equipment (PPE) appropriate for the type of isolation precautions in place Environmental disinfection Special air handling for tuberculosis Previous Slide Next Slide I - Contact Precautions Previous Slide Next Slide Contact Precautions Contact Precautions apply to diseases transmitted by direct contact with the patient’s skin and/or infectious substance and by indirect contact with the patient’s environment Gloves and gowns are used Masks are used in certain circumstances Previous Slide Next Slide Diseases Requiring Contact Precautions Clostridium difficile Congenital rubella Lice Scabies Large wounds Burn patients in ICU Previous Slide Next Slide Specific Information on Acinetobacter Acinetobacter is a group of bacteria commonly found in soil, water, food, and sewage Loves the GI tract – the “gut” flora/bug May also be found on the skin of healthy people, especially healthcare workers Resulting infections are often resistant to many commonly prescribed antibiotics – treatment may be limited to very toxic drugs Previous Slide Next Slide Specific Information on Acinetobacter Acinetobacter can be spread to susceptible individuals through direct person-to-person contact, contact with contaminated surfaces, or exposure in the environment Bacteria can survive for days on inanimate objects such as mattresses, bedrails, IV poles, computer keyboards, and phones Also may colonize in the nose or on hands Previous Slide Next Slide Specific Information on Acinetobacter Outbreaks of Acinetobacter may occur in ICUs and in other hospital units that house patients with weakened immune systems or chronic illnesses May cause pneumonia, bloodstream or urinary tract infections, and skin/wound infections Endocarditits, secondary meningitis, and ventriculitis may also result Patients placed on Contact Precautions for Acinetobacter infection remain on isolation precautions throughout their hospitalization Previous Slide Next Slide Specific Information on MRSA Methicillin-resistant Staphylococcus aureus (MRSA) is the commonly called “staph” bacteria that has become resistant to many antibiotics Patients who have invasive procedures, lengthy hospital stays, weakened immune systems, or who receive dialysis are at increased risk of developing MRSA Community-acquired MRSA (CA-MRSA) is increasing among patients who have never been hospitalized Previous Slide Next Slide Specific Information on MRSA About 30% of the US population have “staph” bacteria that normally live on the skin and in nasal passages without causing harm (colonized) Common infections caused by MRSA include skin abscesses, boils, and impetigo More serious infections that may develop include deep soft tissue abscess, blood stream infections, pneumonia, endocarditis (heart valves, inner lining of the heart), and toxic shock Previous Slide Next Slide Specific Information on MRSA MRSA is spread by worker hands that pick up the bacteria from skin-to-skin contact with a colonized or infected patient, then care for another patient without first performing adequate hand hygiene Contact with contaminated substances or items such as computer keyboards, bedrails, or medical equipment can also lead to transmission MRSA may survive for weeks to months on various surfaces! Previous Slide Next Slide Specific Information on VRE Enterococci bacteria are normally found in the human intestines, the female genital tract, and the environment and may not cause disease Vancomycin is a drug commonly used to treat enterococci infections. In some instances the bacteria is resistant to the drug and is therefore called vancomycin-resistant entercocci (VRE) Patients can be colonized or have an active infection involving the urinary tract, blood stream or wounds Previous Slide Next Slide Specific Information on VRE Risk factors for developing VRE include: persons previously treated with vancomycin or combinations of other drugs, persons receiving prolonged antibiotic therapy, weak immune system, surgery to abdomen or chest, and use of indwelling catheters VRE is spread by direct contact with infected stool, urine, or blood containing VRE Can also spread indirectly by hands or via contaminated environmental surfaces Previous Slide Next Slide Circulator Responsibilities for a Contact Precautions Case Post the RED Contact Precautions sign on the OR door, along with the red “No Traffic” sign Ensure that all staff don gloves, gowns, and masks before the patient enters the OR Inform the receiving department of the patient’s isolation status prior to transferring the patient! Previous Slide Next Slide II - Airborne Precautions Previous Slide Next Slide Airborne Precautions Airborne Precautions apply to diseases transmitted by the airborne route Bacteria or viruses are released into the air when an infected patient talks, coughs, or sneezes These droplets float on air currents and/or remain in the air for long periods of time A susceptible person who does not wear respiratory protection can breathe in the droplets and potentially become infected Previous Slide Next Slide Diseases Requiring Airborne Precautions 1. Pulmonary Tuberculosis (TB) 2. Measles 3. Chicken Pox Unusual bioterrorism agents and others such as … - Smallpox (Bioterrorism) - Viral hemorrhagic fevers (Bioterrorism) - SARS Patients are placed on droplet precautions when any of these diseases are suspected or confirmed Previous Slide Next Slide N-95 Respirators ALL STAFF providing care to patients on Airborne Precautions must wear an N-95 respirator!! N-95 respirators must be fit tested annually by Vanderbilt Environmental Health and Safety (VEHS) – your mask size can change over time Previous Slide Next Slide Airborne Precautions Post the blue Airborne Precautions sign on the OR door before the patient arrives, along with the red “No Traffic” sign Patients coming to the OR who are on Airborne Precautions should be scheduled as the last case of the day whenever possible Limit traffic through the OR during the case Previous Slide Next Slide Airborne Precautions Patients should be placed in negative pressure rooms while on their designated floor/unit Keep the door closed!!! Limit transport of patient from room except for essential purposes Have the patient wear a regular surgical mask any time they are transported from their room Inform the receiving department of the patient’s isolation status prior to transferring the patient Previous Slide Next Slide Airborne Precautions Responsibilities for Anesthesia Providers Non-ICU patients on Airborne Precautions will be recovered in the OR after the completion of the surgical procedure – not in PACU! ICU patients may be recovered in a negative pressure room on their assigned unit The patient will then be transported back to their designated floor/unit Anesthesia machine filters will be changed out after the case (same procedure as for any case) Previous Slide Next Slide Airborne Precautions Responsibilities for OR Charge Nurses When an Airborne Precautions case is boarded, the OR Charge Nurse will order the portable HEPA Unit from Central Supply so that it will be ready to use immediately after the case Previous Slide Next Slide Airborne Precautions Responsibilities for CT-I Staff After patient leaves the OR, bring in the HEPA Unit Place HEPA Unit in the center of the OR, away from the return air vent Plug HEPA Unit into electrical outlet and turn the Unit “on” Previous Slide Allow HEPA Unit to run for ONE HOUR before cleaning the room OR may then be cleaned with standard germicidal agent Portable HEPA Unit Next Slide III - Droplet Precautions Previous Slide Next Slide Droplet Precautions Applies to diseases transmitted by close contact with respiratory secretions Infectious droplets are expelled when a patient coughs or sneezes Droplets remain airborne for about 3 feet, then fall to the floor Previous Slide Next Slide Diseases Requiring Droplet Precautions Influenza Pertussis (Whooping Cough) Mumps Meningitis caused by meningiditis Fifth Disease (Parvovirus B-19) Patients are placed on droplet precautions when any of these diseases are suspected or confirmed Previous Slide H. influenzae or N. Next Slide More on Droplet Precautions Post the green Droplet Precautions sign on the OR door, along with the red “No Traffic” sign Limit traffic through the OR during the case Wear a regular surgical mask when providing patient care – not an N-95 respirator Previous Slide Next Slide More on Droplet Precautions Wear gloves when handling items contaminated with respiratory secretions Wash hands after removing gloves Previous Slide Next Slide More on Droplet Precautions After the patient leaves the OR/PACU/etc., the room can be cleaned with the standard germicidal agent Patients should be placed in private rooms while on their designated floor/unit, but negative pressure rooms are unnecessary During transport, patients wear a regular surgical mask Previous Slide Next Slide Common Tasks for ALL Isolation Precautions Cases The following slides describe steps that are taken for every case involving isolation precautions Previous Slide Next Slide Scheduling any Isolation Precautions Case Surgeon or resident boards the case Surgery scheduler determines whether or not the patient is on isolation precautions (if uncertain, scheduler contacts the patient care unit) Surgery scheduler documents isolation status in ORMIS, which feeds onto the eOR board and the electronic White Board There are 4 possible choices for isolation status: - None - Airborne - Droplet - Contact Previous Slide Next Slide Circulator Responsibilities for any Isolation Precautions Case Post the appropriate “Isolation Precautions” sign and the “No Traffic” sign on OR door Ensure all needed supplies and equipment are available in the OR Remove all unnecessary equipment from the OR before the case begins Ensure ALL staff involved in the case don gown, gloves, and masks before the patient enters the OR (if patient is on airborne precautions, use N-95 respirators instead of surgical masks) Isolation Cart with gowns, gloves and other isolation supplies is kept outside the OR door Close all cabinets (cannot open cabinets during the case!) Previous Slide Next Slide OR Charge Nurse Responsibilities for any Isolation Precautions Case Assigns a “runner” to the OR, who will assist in obtaining additional supplies for the case (this person will NOT enter the OR at any time!) Previous Slide Next Slide Anesthesia Provider Responsibilities for any Isolation Precautions Case When transporting a patient direct to the OR: -don appropriate PPE prior to entering patient’s room - assess patient’s condition and equipment needed for transport - conduct handoff with bedside nurse, including verification of the patient’s isolation status Previous Slide Next Slide Responsibilities for Other Staff Assisting with Transport to the OR Don PPE prior to entering the patient’s room Verify the patient’s isolation status with the bedside nurse Team places a clean sheet over the patient Place patient charts in a plastic bag (obtain a plastic Isolation Bag from the yellow Isolation Cart) Place monitors, charts, etc. on top of the clean sheet for transport to the OR Have a “clean” person available (one who has not touched the patient or patient’s bed/belongings) to push elevator buttons and open doors Previous Slide Next Slide During the Case… Responsibilities for CT-I Staff Saturate a rag with germicidal disinfectant agent and wipe down patient’s bed in hallway (includes mattress, side rails, headboard and footboard) Wait 10 minutes for the bed to dry – place an isolation bag on bed during the drying phase so others know it belongs to a patient on isolation precautions Make patient bed as usual Drape bed with clear plastic Put isolation sign on bed Previous Slide Next Slide Communication Regarding Return of Patient to the Unit Circulator calls unit charge nurse to inform them of impending transfer and verifies isolation status Anesthesia provider calls report to the patient’s bedside nurse and verifies isolation status Circulator conducts “rolling call” to unit as the patient leaves the OR Unit receives call and notifies charge nurse and bedside nurse that patient is in transit and verifies isolation status Previous Slide Next Slide Responsibilities for Staff Assisting with Transfer Back to the Unit All staff involved in patient transport don new PPE before transfer begins Have a “clean” person available (one who has not touched the patient or patient’s bed/belongings) to push elevator buttons and open doors Transport monitors and other equipment are wiped down with a germicidal disinfectant agent before leaving the patient’s room Staff remove PPE prior to exiting patient’s room Anesthesia provider and bedside nurse conduct report/handoff and verify isolation status Previous Slide Next Slide After the case The OR should be cleaned with germicidal disinfectant agent according to normal standards All linen and trash from the room are handled in the same manner as from any case Previous Slide Next Slide Questions or Concerns? Contact Infection Control & Prevention Phone: 60725 Pager: 835-1205 Previous Slide Next Slide