week 8_biotechnology and medicine
advertisement

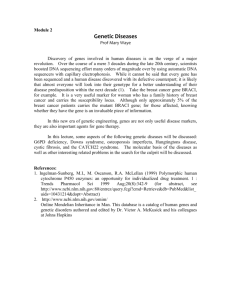
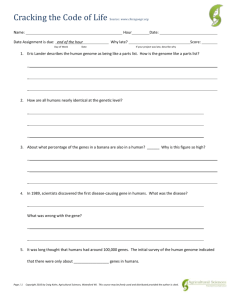
PTT 104: Biotechnology and Medicine Department of Chemical Engineering Technology, UniMAP Semester 1, 2013/2014 khadijahhanim@unimap.edu. my Course outcome: Able to differentiate scopes and importance of various biotechnological streams. TOPIC COVERS: Illustrate scopes of medical biotechnology and examine gene transfer methods, gene therapy and Human Genome Project (HGP) and applications. Lesson Contents 1. Detecting and Diagnosing Human Disease Conditions 2. Medical Products and Applications of Biotechnology 3. Gene Therapy 4. The Human Genome Project Detecting and diagnosing human disease conditions Molecular biology has advanced tremendously- providing scientists molecular techniques in combating human diseases. Using model organism: mice, rats, worm and flies. We not really unique at genetic level. Share some similarities (genes) with these organisms. A no. of human genetic diseases also occur in model organisms. Therefore, can use model organisms to identify disease genes and test gene therapy and drug based therapeutic approaches to check their safety and effectiveness prior to clinical trials in human. Why model organism? - Because we cannot manipulate human genetics for experimental purposes. - Illegal or unethical to force human to breed/ to take out their genes to learn how they function. Therefore, use model organisms. Many important genes are highly conserved between species. If a gene found in model organisms, we can make hypotheses/predictions about how the gene might function in humans. Related genes are called homologs. For eg: a gene thought to play a role in human illness can be eliminated/knock out. Then, the effects can be studied to learn about the function of the gene. Biomarkers for disease detection In theory, right diagnostic tools, possible to detect every disease at early stage. For many diseases, early detection is critical for providing the best treatment and improving the odds of survival. Detection approach- BIOMARKERS as indicator of disease. What is biomarkers? Protein produced proteins produced by diseased tissue or proteins whose production is increased when a tissue is diseased Many biomarkers are released into body fluids ie: blood and urine as a product of cell damage For eg: protein called prostate-specific antigen (PSA) released into bloodstream when prostate gland is inflamed and elevated levels can be marker for prostate inflammation/prostate cancer. Many companies are actively searching for better biomarkers that can be used in early detection and diagnosis. Detecting genetic diseases Testing - - for chromosome abnormalities and defective genes: Genetic testing occurred on fetus: identify sex/genetic diseases (occur because of alteration of chromosome no). Eg: Down syndrome: most contain 3 copies of chromosome 21. Symptoms: mental retardation, short stature and broadened facial features. Methods of detection: Amniocentesis •When the developing fetus is around 16 weeks. •A needle is inserted thru the mother’s abdomen into the pocket of amniotic fluid surrounding and cushioning the fetus • fluid contain fetus’s cells. Isolated and cultured for a few days to increase the no. •Chromosomes are put onto glass slide and stained with diff. dyes. •The chromosomes are counted •Technique also called as karyotype: use to determine the sex of a child. Amniocentesis Chorionic villus sampling • A suction tube is used to remove small portion of a layer of cells called chorionic villi- tissue that help forms the placenta. • Advantage: enough cells obtained for immediate karyotyping • Can be done earlier: 8-10 weeks. • Can cause miscarriage. Detecting genetic diseases Testing for chromosome abnormalities Fluorescence in situ hybridization (FISH) – new technique for karyotyping Blood withdrawn from adult- white blood cells used for karyotyping Chromosome spread is prepared on a slide. Fluorescent probe are hybridized to each chromosome. Each probe is specific for certain marker sequences on each chromosome. Useful for identifying missing chromosomes and extra chromosomes, but much easier to detect defective chromosomes For eg: in leukimia: DNA is exchanged between chromosomes 9 and 22 so genes from 9 are swapped onto 22 and vice versa. This exchange can be detected by FISH. Definition of Karyotypes Karyotypes describe the number of chromosomes, and what they look like under a light microscope. A karyotype is an organized profile of a person's chromosomes. In a karyotype, chromosomes are arranged and numbered by size, from largest to smallest. This arrangement helps scientists quickly identify chromosomal alterations that may result in a genetic disorder. Other methods of detection Restriction fragment length polymorphism (RFLP) analysis: defective gene sequences may be cut differently by RE than their normal genes because of nucleotides changes in mutant genes can affect RE cutting sites to create more or fewer fragments. Medical products and applications of Biotechnology Major areas in medical biotechnology: identifying novel drugs and developing new ways to treat disease. Eg: Oncogenes: genes involved in the growth of cancer. Oncogenes: produced proteins that function as transcription factors and receptors for hormones to change growth properties of cells causing cancer. Researchers are focusing on the protein produced by the oncogenes as a target for inhibitors: drugs that can bind to the protein and block their function. Pharmacogenomics: personalized medicine Pharmacogenetics is referred to the study of genetics influence on individual respond to drugs. Designing the most effective drug therapy and treatment strategies based on the specific genetic profile of a patient Individuals can react differently to the same drugs Different degrees of effectiveness and side effects because of genetic polymorphisms Improving techniques for drug delivery - In addition to developing new drugs, companies are working to develop innovative ways to deliver drugs to max their effectiveness. Getting drugs to where it need to function. Eg: drug to treat arthritis taken orally. Small amount is absorbed by body and transported to knee joint. Other factors that influence drug effectiveness: Drug solubility (ability to dissolve in body fluids) Drug breakdown by body organs Drug elimination by liver/kidneys Microspheres: tiny particles that can be filled or coated with drugs. Made by materials that closely resemble the lipids in cell membranes. Delivery of microspheres as a mist sprayed into airways thru nose/mouth has been successfully in treating lung cancer/asthma/tuberculosis/flu. Nanotechnology and nanomedicine Nanotechnology – involved in designing, building, and manipulating structures at the nanometer scale nm is 1 billionth of a meter Nanomedicine – applications of nanotechnology to improve human health Nanodevices to monitor blood pressure, blood oxygen levels, hormone concentrations Nanoparticles that can unclog arteries, detect and eliminate cancer cells; smart drugs that could seek out and target specific cells Scientists have developed smart drugs using viruses/nanoparticles that are introduced into the body to seek out or target specific cells to treat or destroy the cells. Figure shows a plastic nanoparticle covered with antibodies against cancer cell proteins that allow the particle to bind to the cancer cells. Inside the agent are contrast agents- can be used for MRI or X-ray to detect tumors, chemotherapy drugs that can diffuse out of the cell to kill tumor. Vaccines and therapeutic antibodies Vaccines: can be used to stimulate body’s immune system to produce antibodies and provide a protection against infectious microbes. Vaccines against cancer is still being developed. Cancer vaccines: not preventive but designed to treat a person who already has cancer. A person is injected with cancer cell antigens to stimulate immune system to attack cancer cells Vaccine for Alzheimer’s disease Primary purpose of vaccination: to stimulate antibodies production by immune system to ward off foreign materials. Antibodies can also be used to treat existing condition as opposed to preventing infectious microbes from causing a disease. Monoclonal antibodies used to treat Cancers Cardiovascular disease Allergies Other conditions Gene therapy Gene therapy is the delivery of therapeutic genes into the human body to correct disease conditions created by a faulty gene or genes How are genes delivered? How can genes be sent to the proper tissues and organs? Can it be effective and safe? Gene therapy: How is it done? Ex vivo gene therapy In vivo gene therapy Ex = out of Introducing genes directly into tissues and organs in the body without removing the cells Vivo = something alive Cells from a diseased person are removed, treated in the lab using techniques similar to bacterial transformation and reintroduce into the patient. Challenges: delivering genes only to intended tissues not tissues throughout the body. Eg: using virus Vectors for gene delivery Require a safe and effective delivery of therapeutic genes. Both ex-vivo and in-vivo rely on viruses as vectors to introduce genes into cells. A viral vector would use a viral genome to carry therapeutic gene/s to infect human cells thereby introducing the gene/s. Some of the potential vectors: Adenovirus (causing common cold) Influenza (flu) Herpes virus (cold sore or STD) Must make sure the virus has been genetically engineered and inactivated so that it can neither produce disease nor spread throughout the body Viral infection to human body cells By binding to and entering cells and then releasing their genetic material into nucleus/cytoplasm of human cell. DNA/ RNA Infected human cell serves as a host for reproducing the viral genome and producing viral RNA and proteins. Viral protein ultimately assemble to create more viral particles that break out of host cells so they are free to infect other cells and repeat the cycle. Viral life cycle Viruses are effective in infecting human cells They can make good vectors: efficiently infecting human cells Adenovirus: can infect many types of body cells efficiently HIV virus: on entering a host cell they copy their RNA genome into DNA and then randomly insert their DNA into the genome of the host cell where it remains parmanently- Integration. - Integrate therapeutic genes into DNA of human host cells, allowing permanent insertion of genes into chromosome as a way to provide lasting therapy. Some virus only infect certain body cells. Allow for targeted gene therapy. For eg: herpes virus (infects cells of the central nervous system) may effectively treat genetic disease of the brain, Alzheimer and Parkinson disease. Other delivery options: - - Naked DNA DNA by itself without viral vector, that is injected directly into body tissues. Transfect cells by mixing them with naked DNA in a tube. Disadvantages: relatively small no of cells uptake. May not be enough cells expressing the therapeutic genes for gene therapy to have any effect on the tissue. Other delivery options: Liposomes - small-diameter hollow microspheres made of lipid molecules - Packaged with gene and injected or sprayed into tissues A similar technique involves coating a tiny gold particles into cells using a DNA gun Antisense RNA and RNA interference for gene therapy Antisense RNA Technology A way to block translation of mRNA molecules to silence gene expression Called RNA or gene silencing Promising way to turn off disease genes Used successfully in cell culture, but has yet to live up to its promise as a treatment for disease RNA interference (RNAi) Double-stranded RNA molecules are delivered into cells where the enzyme Dicer chops them into 21-nt-long pieces called small interfering RNAs (siRNAs) siRNAs join with an enzyme complex called the RNA-induced silencing complex (RISC) RISC shuttles the siRNAs to their target mRNA where they bind siRNA-bound mRNAs are degraded so they cannot be translated into a protein Curing genetic diseases: Targets for gene therapy Focusing on single gene mutations or deficiencies. For eg: sickle cell anemia Easier to cure compare to multiple genes The first human gene therapy In 1990, a patient with severe combined immunodeficiency (SCID). SCID- lack a functioning immune system caused by a defect in a gene called adenosine deaminase (ADA) ADA produce enzyme involved in metabolism of nucleotide dATP. Lack of ADA causes accumulation of dATP. and is toxic to T cells Without T cells, B cells cannot recognize antigen and make antibodies - - - - - To treat SCID: Normal gene for ADA was cloned into a vector and then introduced into an inactivated retrovirus. Ex vivo gene therapy was used. Small amounts of T-cells were isolated from patient’s body and cultured in the lab. Her T cells, were infected with ADAadenovirus and the infected adenovirus were further cultured. Retrovirus integrate their genome (containing ADA genes) into the patient’s chromosome during culturing. These ADA-containing T cells were reintroduced back to the patient’s body. Treating cystic fibrosis Cystic Fibrosis – two defective copies of a gene encoding a protein called cystic fibrosis transmembrane conductance regulator (CFTR). Normal protein serves as a pump to remove chloride ions from cell The CFTR important for maintaining the proper balance of Cl inside cells. Absence/altered of CFTR causes CF. Produced by many cells in the body – skin, pancreas, liver, digestive tract, male reproductive tract, and respiratory tract. Abnormality of this gene in trachea can cause accumulation of Cl ions lead to extremely thick mucus that clog airways. Normally, mucus in trachea helps sweep dust and particles out of the airways to keep this materials out of the lungs. But when water enter trachea- mucus become thick. Thick mucus-provide ideal environment for microbes to grow- leading to infections. Can lead to pneumonia and respiratory failure. Others: can cause infertility and salty sweat. Treatment of CF Normal CFTR gene into liposomes and spraying the liposomes into the nose and mouth of CF patients as an aerosol or into airways via hose. But not reliable cure because DNA delivered via liposomes does not integrate into chromosomes. Challenges facing gene therapy Potential risks of viruses as vectors Death of Jesse Gelsinger in 1999 due to complications related to adenovirus vector Death of 2 children in France in 2002 Temporary cessation of a large number of gene therapy trials and FDA stopped most retroviral studies Greater patient monitoring Challenges facing gene therapy Can gene expression be controlled? Can we safely and efficiently target only the cells that require the gene? How can gene therapy be targeted to specific regions of the genome? How long will therapy last? Will immune system reject? How many cells need to be corrected? Human genome project Many of the disease genes were discovered thru HGP. Scientists have been developing complex map showing the locations of normal and diseased genes on human chromosomes.