A Social Norm Strategy for
Polio Eradication in Pakistan
Susan Roe, UNICEF ROSA / Kathmandu, Nepal
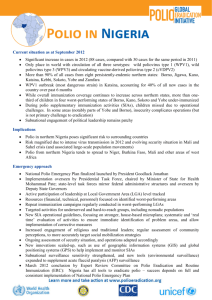
Now A Much More Localized Problem …
The Shift in Polio
Circulation from1988 to 2010
Certified Polio-free regions (114 countries)
Not Certified but non-endemic (73 countries)
Endemic with wild polio virus ( 3 countries)
The boundaries and names shown and the designations used on this map do not imply the expression of any opinion
whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or
area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent
approximate border lines for which there may not yet be full agreement.
WHO 2010. All rights reserved
Source: WHO/POLIO database, as of August 2010
2010
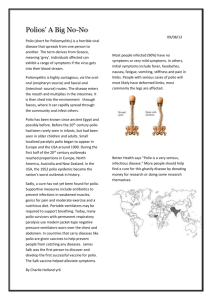
Global Efforts = Continued Progress …
Global Update for polio cases
Country
Cases
this week
Global update
2011
2012
Afghanistan
2
80
12
India
0
1
0
Nigeria
4
62
52
Pakistan*
1
198
23
Cases in endemic countries
341
87
Cases in non-endemic countries
309
4
Total cases
650
91
*Data as of 4 July 2012
GPEI Goals:
• By end 2011: Cessation of transmission in at least 2 out
of 4 endemic countries; and,
• By end 2012: Cessation of all WPV transmission!
Pakistan Epidemiology - Challenges
From 2011 cases / data:
•
•
•
•
71% cases below 2 years of age
77% Cases Pashto Speaking (89% of Karachi cases)
23% of the polio cases from 'refusal' families
88% cases living in Multiple Family Dwelling
Vaccination status (based on recall):
• 31% no OPV dose
• 73% no routine OPV dose
An Innovative Approach Needed
for Engagement with HRGs
• Pashto speakers: 73%
• Have lower knowledge and risk perception
regarding disease (factual beliefs / personal
normative beliefs – e.g. attitudes - individual);
• Yet concerns / lack of knowledge about OPV
safety are largest among Pashtuns (with rumors
of infertility / sterility also highest in this group);
• Are more likely to chronically refuse than other
groups; and,
• Among all 2011 refusal cases (47) or
89% were Pashto-speakers mostly
clustered in / around Balochistan. *KAP 2012
From WPV Cases 2009 - 2012
“Refusal” A Social Norm? Consider Social Dimensions
What do other community members do or say? (Empirical Expectations)
My neighbors don’t accept and “told me that this vaccine is brought from
America and contains family planning medicine.”
What do people in the community expect from me or others?
(Normative Expectations)
“My mother-in-law does not allow taking of the drops. She says that her
children remained safe without them, so yours will be fine.”
Are there consequences for not complying? (Normative Expectations)
“These drops are not accepted by our household (e.g. husbands) and
if we raise the issue we could be kicked out of our home if we
dare say something”.
Or perhaps - What do I do based on actions of others (but not caring
what they think)? A Descriptive Norm?!
Need for further research and investigation!!!
Challenges Associated with Existing
Polio Structure
• Top – down multi-level structure;
• Perceived as externally / internationally driven;
• Focus: individual behavior (acceptance), coverage and
prevalence numbers;
• Delivered door-to-door - isolates / privatizes action casts community as “receivers”;
• Messaging primarily one-way announcing campaign
dates and promoting readiness to receive;
• Fails to address other issues (intensive focused on
eradication but some linkage to RI - convergence); and,
• Credibility, motivation and geo-political dimensions
highly contentious (Western conspiracy, drone attacks
vs. immunization, fake campaigns to locate Bin Laden).
Existing Communication / Social Mobilization Strategies
• Message development - demand creation, addressing incorrect
factual beliefs and shifting attitudes (Individual);
• Enlistment of multiple relevant network members / influentials
as part of process and to enhance credibility and trust (Social) ;
• Introduction of new “relevant network - Com Net (in HRDs) to
forge linkages with communities for engagement and interaction
(Social);
• Recruitment of HR group members / women as part of network –
and build capacity (Social);
Existing Communication / Social Mobilization Strategies
• Specific HRG strategies reach out to marginalized populations (festivals
and religious gatherings – information provision (Individual);
• New mass media campaign (How Far Would You Go?) to activate
stakeholders across levels & increase visibility (Individual);
• Enlistment of celebrity and culturally relevant advocates to promote polio
for the wider population (localized ownership - Individual);
• Continued work with media to promote relevance, benefits and success at
local level (visibility, local ownership / support - Individual).
Further Considerations …
• Data related to factual beliefs and personal
normative beliefs (attitudes) available through past
research initiatives;
• Resistance to the vaccine may be
affected / influenced / motivated
by social expectations;
• Will require more investigation /
research into Empirical and
Normative expectations;
• In addition to survey tools – use of
in-depth interviews and focus group
discussions can also be applied.
Sample Empirical Questions:
Do your neighbors accept polio drops every time they are offered? Why or
why not?
Do your leaders encourage you to immunize your child and that polio drops
are safe and cause no harm?
Does your family members (husbands / mother in laws) welcome polio
vaccinators when they come to your door?
Does your community encourage one another to support social mobilization
around OPV and to accept drops when they are offered each and every
time?
Sample Normative Questions:
Do you feel that your neighbors think that you ought to accept polio drops
every time they are offered?
What happens to a member of the Pashtun community who accepts polio
drops when others feel that he / she shouldn’t?
Do you think that your neighbors believe you and others in the community
should accept OPV because it is beneficial for the whole community?
What would your community do or say about someone who accepted polio
drops when others disagree or feel they should be refused?
Desired Outcomes …
• Polio acceptance / demand creation at care-giver
and household level (PB - Individual);
• Positive attitudes around vaccine acceptance and
service seeking behavior (PNB - Individual);
• Demand and acceptance for polio drops
demonstrated and promoted by others (EE - S);
• Create expectation that community / relevant
network expects others to demand and accept
OPV each and every time it is offered (NE - S).
To do this – in addition to existing strategies - need to
introduce new social norm around polio acceptance
within the HRG (e.g. Pashtun) community.
Proposed Way Forward
• Review data / conduct additional research related to further
learning and next steps addressing social expectations;
• Revisit existing messages and strengthen interdependent
dimensions / social normative perspectives;
• Use collective meetings (facilitated by Com Net and relevant
network members or leaders) for values deliberation and
unpacking scripts related to good parenting, child health and
social identity;
• Use triggering to explore issue of social dilemma and for
addressing incorrect factual beliefs / rumors;
• Restructure existing networks through blending of Com Net and
traditional leaders in support of organized diffusion;
• Use traditional gatherings or religious festivals as a mechanism
for bringing polio discourse more out into the open while
building credibility and trust;
• Use of pledges or “public affirmation of commitment” to new polio
acceptance norm (building visibility, confidence and trust);
• Consider use of symbolic, collective immunization events to signal
shift to new norm, build confidence and solidify internal motivation
(also ensure acceptance when H2H rounds commence);
• Sustain and prevent “slippage” through continued engagement with
local Com Net workers and social mobilizers / vaccinators from local
community;
• Continue / build on existing polio social mobilization activities in
support of organized diffusion to sustain and reinforce (other partners
and media to expand reach and spread);
• Promote harmonization of social and moral norms around
immunization and gather evidence to negotiate with officials regarding
timing / severity of proposed legislation;
• Explore possibility for replication especially along migration routes,
cross border or at end point destinations; and,
• Celebrate “win – win” situation with community, leaders, GoP, PEI
partners as related to implications for county, regional and global
eradication.
Potential Risks /Additional Challenges
• Time / effort required for additional research / analysis
for new data related to expectations;
• Community dialogue / discussion needs skilled
facilitation – capacity?;
• Sensitivity of specific group being targeted / singled out;
• Visibility of collection immunization could also be misunderstood or perceived as sensitive (and backfire with
other groups / media);
• Limited time (GPEI goals) for implementation / process!
Many Thanks for Kind Attention!