presentation ( format)

Total Quality
Improvement Assessment
Of Strep C β-Hemolytic
Streptococci Treatment in a College Population
Valerie Kiefer MS, APRN
University Of Connecticut
The University of Connecticut provides primary health care to approximately
20,000 students annually.
24-Hour Care
Fee for Service
Departments:
◦ Primary Care
◦ Walk-In Clinic
◦ Women’s Clinic
◦ Allergy Clinic
◦ Counseling & Mental Health
◦ 9 Bed In-Patient
◦ Laboratory
◦ Radiology
◦ Pharmacy
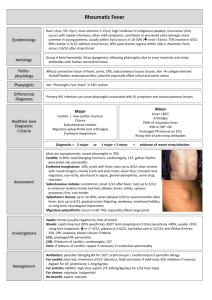
What is Group C Streptococcus?
Gram positive anaerobe which produce small or large colonies
Usually beta hemolytic
Share many clinical characteristics with
GAS
Group C can cause isolated exudative or common source epidemic pharyngitis indistinguishable clinically from GAS
Large colony
Small colony are not associated with pharyngitis
Why Study Group C Strep?
Pharyngitis and Group C Streptococcus common in college health
Do You Treat or Test for Group C strep pharyngitis?
Unknown if the association of group C
(BHS) pharyngitis in college students is related to immunity issues, lifestyle or other factors
Review Of The Literature
Studies that have shown strong epidemiologic association between group-C BHS and endemic pharyngitis in college students
Review Of The Literature
Turner et al, JAMA 1990
Association of Group C β-Hemolytic
Streptococci With Endemic
Pharyngitis Among College Students
Purpose: NGA BHS could be detected more commonly in the throats of students with symptomatic pharyngitis than among healthy controls of similar age.
Performed throughout 2 school years
NGA BHS group, only those from group C were isolated more often/compared with the control group (26% to 11%)
Established a strong epidemiologic association between group C BHS and endemic pharyngitis in college students
Group C BHS had fever, exudative tonsillitis and anterior cervical adenopathy more frequently than patients who were negative for group C
Turner et al, Journal Of Clinical
Microbiology 1997
Epidemiologic Evidence From
Lancefield Group C Beta Hemolytic
Streptococci As A Cause Of Exudative
Pharyngitis In College Students
Compared the isolation rates of strains of group C BHS from throat swab cultures of patients with exudative pharyngitis, the common cold, and healthy controls
College health/chart review
Isolation of Lancefield group A and C beta-hemolytic streptococci from throat cultures was used as an outcome measurement
Lancefield Group C strep associated with purulent exudative pharyngitis in college students.
Broyles et al, Clinical Infectious
Disease 2009
Population-Based Study of Invasive
Disease Due to β-Hemolytic
Streptococci of Groups Other than A and B
Different Species of non A, non B – hemolytic streptococci and their clinical significance
NABS Comprise multiple distinct species that cause infections. (G,B,H)
Manifestations differ, specification may be warranted in clinical settings
Tiemstra et al, Journal American Board
Family Medicine 2009
Role of Non Group A Streptococci in
Acute Pharyngitis
The role of Non Group A strep as pathogens of pharyngitis is controversial.
Data is limited and conflicting on whether these bacteria are true pathogens of pharyngitis and whether treatment is indicated in all or just select cases.
Objective: Determine whether in non-GAS identified on culture if the clinical signs and symptoms resemble group
A implicating them as true pathogens or if they resemble culture negative pharyngitis suggesting they are viral in etiology
Retrospective case control study
Mean age 26 years
GAS by RAS or culture
Neg. RSA or culture
Headache and fever associated strep infection, no difference between GAS and non GAS
Exudates and lymphadenopathy were also associated with both GAS and non GAS compared with viral infection
2 criteria were present, risk any strep infection rose to 55% (27% for non GAS or GAS)
3 or more criteria present, risk increased to 81% (non-GAS 34%, GAS 47%)
Results: Young, adult population with acute pharyngitis, non GAS was as common as GAS
Non GAS same clinical features typically associated with GAS
Suggests clinicians may want to consider treating patients with proven or presumptive non GAS pharyngitis who fail to respond to symptomatic therapy or who are at increased risk for sequelae
Further study needed/antibiotic treatment
Cooper et al, Annals Of Internal
Medicine 2001, Principles of
Appropriate Antibiotic Use For Acute
Pharyngitis In Adults, Position Paper
Examines the available evidence regarding the diagnosis and treatment of acute
GABHS in adult patients
Recommendations made that balance concerns about the potential consequences of untreated GABHS and the goal of decreasing inappropriate antibiotic prescriptions
Group A strep is the causal agent in 10% of adult cases of pharyngitis.
Antibiotics are prescribed to 75% of adult patients with acute pharyngitis.
Incidence of complications regardless of treatment with antibiotics is low.
Antibiotic therapy instituted within 2-3 days of symptom onset hastens symptomatic improvement by 1-2 days in patients/cultures grow GABHS.
Antibiotics do not have this effect with a negative culture.
Symptom duration is strongly related to patient satisfaction.
Antibiotic treatment benefits only those patients with GABHS.
Limit antibiotic prescriptions to patients who are most likely to have GABHS infections.
Rutecki, Top Papers Of The Month,
Does This Patient Have Group A Strep
Pharyngitis?, Consultant 2012
This paper discussed pharyngitis and the
Centor Criteria.
Include Centor Criteria in
Management/approach to pharyngitis.
Shah, Centor and Jennings,
Severe Acute Pharyngitis Caused by
Group C Streptococcus, 2006 Case
Report
Group C Strep. / Approx. 5% prevalence
Present Broad Spectrum of Severity
Less common cause of acute pharyngitis but has both similar microbiology and presentation to group A.
Both cause exudative or epidemic pharyngitis which are indistinguishable clinically.
5 Important Considerations/Neg.
RSA/ Worsening Symptoms
Mono
Acute HIV
Group C
Peritonsillar Abscess
Lemierre’s Syndrome
(Fusobacterium necrophorum)
Neg. RSA /possibly worsen over the next week
Reasons We Treat Strep Throat
Strep A causal agent 10%
Reduce Symptoms
Prevent the spread of Streptococci
Prevent Infectious Complications
◦ Tonsillar Abscesses
◦ Sinusitis
Prevent Rheumatic Fever /2011 incidence of rheumatic fever in the US was 1 per 1 million strep throats
Prevent Glomerulonephritis
Majority of adults have a self limited illness who do not need antibiotics
Group C Strep-
Does not cause some of the complications caused by Group A
Uncommon cause of pneumonia
Group C Strep sinusitis has been reported
Rarely isolated from blood cultures/fewer than 1% of all bacteremia
Group C and G Strep meningitis have
been reported and are often associated with endocarditis
Group C Strep arthritis uncommon/occurs in joints with preexisting rheumatologic abnormalities
Role of Non-Group A Streptococci
Conflicting and limited data
◦ Guidelines/Standards treat Strep A
◦ Controversy regarding management strategy for adult pharyngitis
◦ Dr. Centor points out in the article: Pharyngitis
Management: Defining the Controversy
JGIM (2007)
◦ Randomized trial data suggests a symptomatic benefit for treating Group C patients
Infectious Diseases Society of America
(IDSA) 2012 Clinical Practice Guideline for the Diagnosis and Management of
Group A Streptococcal Pharyngitis
Group C Strep common cause of acute pharyngitis among college students and adults
Primary reason to identify GCS as the etiologic agent of acute pharyngitis is to initiate antibiotic therapy that may reduce the clinical impact of the illness
Currently, there is no convincing evidence from controlled studies of a clinical response to antibiotic therapy in patients with acute pharyngitis from GCS isolated from the throat
CDC recommends not treating GCS.
Community Vs. College Health
Rapid Strep A testing (RSA)
◦ Fever
◦ Exudative Tonsillitis
◦ Adenopathy
◦ No cough
◦ A back up throat culture is not routinely performed
◦ Community/Follow up visit
UCONN
RSA
Back Up Throat Culture
Treated by Clinical Presentation
RSA Neg.
Strep C No Improvement
Antibiotic
Follow up visit or antibiotic left at clinic for pick up by student
Time period of antibiotic treatment could range from 1-5 days post visit
OSOM
RSA
Ultra Strep A Test
98.2% Sensitive
Single Swab Culture
Quality of the test depends on the quality of the sample. Negative results can occur from inadequate specimen collection
Does not differentiate between carriers and acute infection
Used as an adjunct to other information available to the provider
Purpose of Study/Quality Issues
Addressed
Quality Improvement Assessment
To determine if antibiotic use in the treatment of Group C BHS in the college population is appropriate in relationship to community standards/guidelines.
◦ College Population DIFFERENT!!
To evaluate if the University of Connecticut’s quality of care and guidelines are appropriate in the treatment of Group C BHS
To assess the time frame of treatment or non treatment of Group C BHS .
Same day treatment
Next day treatment
Treatment within 2-5 days of visit
To evaluate key indicators in relationship to
Group C BHS in the college population.
◦ Tonsillitis
◦ Mononucleosis
Collected data before & after an educational action for clinical staff
Performance Goals
Difficult to set/lack of guidelines
College Health taken into account
75% adult pharyngitis patients treated with an antibiotic
Performance Goals
70% Total Patients Treated with antibiotic
10% Patients Treated with antibiotic day 1
10% Patients Treated with antibiotic day 2- 5
Looked at:
Under and over usage of antibiotics
Quality of care and outcome issues as well as practice guidelines
Data Description
Retrospective Chart Audit January/11 to
March/11
786 Diagnosed With Pharyngitis
PeopleSoft#
Date of Examination
Positive for Group C BHS
Negative treatment with an antibiotic
Treated with an antibiotic/time frame
Tonsillitis or Mononucleosis
Follow up visit or phone call
Antibiotic Use
Before Corrective Action:
119 Positive Group C BHS
Patients diagnosed with
Strep C
Same Day
Treatment
Next Day
Treatment
Treatment in 2-5
Days
No Treatment
Cases of
Tonsillitis
January
Patients
13
3
3
6
3
February
Patients
March
Patients
Total
15
14
2
7
6
24
11
10
11
10
52
28
15
24
19
%
44%
23%
13%
20%
16%
Follow-Up Done
Before Corrective Action
Patients diagnosed with
Strep C
Follow-up
Phone Call
Follow-up Visit
January
Patients
February
Patients
March
Patients
Total
13
9
30
4
37
13
70
26
%
59%
22%
Follow-Up Done
Before Corrective Action
80
70
60
50
40
30
20
10
0
January
Patients
February
Patients
March
Patients
Total
Follow-up Phone Call
Follow-up Visit
Data Analysis
Before Corrective Action:
80% Treated with an antibiotic
44% Same Day
23% Next Day
13% Day 2-5
16% Tonsillitis
6% Mononucleosis
59% Follow-up Phone Call
22% Follow-up Visit
Antibiotics Used
Penicillin VK 500 mg TID
Zithromax (Z-Pak)
Amoxicillin 875 mg BID
Augmentin 875 mg-125 mg BID
Clindamycin 300 mg TID
Biaxin 500 mg BID
IDSA Recommendations
PCN 500 MG BID
AMOXICILLIN 50 MG/KG QD
(MAX = 1000 MG)
AZITHROMYCIN 12 MG/KG QD
(MAX = 500 MG)
Performance Goals Comparison
Goal: 70% Treated
Performance: 80% Treated
Goal: 10% Treated/Next Day
Performance: 24% Treated/Next Day
Goal: 10% Treated/Day 2-5
Performance: 13% Treated/Day 2-5
Discussion
Community Standards/College Health
Standards
Laboratory On Site/Depending on the time the student is seen, we will get a throat culture back the next day
2 Day Illness History/Average of 2 days of illness before they come in for an evaluation
Issues Of Concern
Antibiotic Offered Too Soon/Patient would have eventually improved and not needed to be treated with an antibiotic
80% Antibiotic Treatment for Strep C was too high in relation to community standards and we were prematurely over prescribing antibiotics
Laboratory Turnaround/Prompt turnaround of backup throat cultures contributed to our increased antibiotic usage. If the backup culture was returned 1 day post visit / probability of student still having a sore throat was high which in turn could influence the provider to prescribe an antibiotic
Issues Of Concern
Reevaluation Of Symptoms
Prescribing antibiotics without consistent reevaluation of patients was not appropriate medical care or follow up and addressed quality of care issues
Corrective Actions
Positive Group C BHS results would not be reported until 3 days post visit/Address the quick turnaround time of cultures from our laboratory
Laboratory results available if needed/provider call the lab for a result if there was a clinical concern
Provider would continue patient education/Issues or concerns call or make an appointment to be seen
Comfort Measures/Treatment for Sore Throat
Corrective Actions
Clinical Judgment/Same day treatment would not be addressed due to the involvement of the providers judgment regarding antibiotic usage
Group C BHS reported to clinician
Student with continued symptoms/ follow –up visit/antibiotic would not be left at the clinic or in the pharmacy
Original provider or back up clinician
Corrective Actions
Implemented
January 2012
Re-Measuring Of Data
Chart Audit
January 2012 to March 2012
107 Charts Audited
773 With Pharyngitis Diagnosed
Same Criteria
PeopleSoft #
Date Of Examination
Positive For Group C BHS
Negative Treatment With An Antibiotic
Treated With An Antibiotic
Time Frame of Treatment
Same Day, Next Day, Day 2-5
Tonsillitis or Mononucleosis Diagnosed
Follow Up Visit or Phone Call
Data Collection
After Corrective Actions:
107 Positive Group C BHS
Patients diagnosed with
Strep C
Same Day
Treatment
Next Day
Treatment
Treatment in 2-5
Days
No Treatment
Cases Tonsillitis
January
Patients
14
1
0
8
9
February
Patients
March
Patients
Total
25
0
5
21
10
14
2
3
14
10
53
3
18
43
29
%
50%
3%
7%
40%
27%
xxx
Antibiotic Use
After Corrective Action
60
50
40
30
20
10
0
January Patients February Patients March Patients Total
Same Day Treatment
Next Day Treatment
Treatment in 2-5 Days
No Treatment
Follow-Up Done
After Corrective Action
Patients diagnosed with
Strep C
Follow-up Phone
Call
Follow-up Visit
January
Patients
14
6
February
Patients
March
Patients
Total
25
15
22
4
61
25
%
57%
23%
70
60
50
40
30
20
10
0
January
Patients
Follow-Up Done
After Corrective Action
February
Patients
March Patients Total
Follow-up Phone Call
Follow-up Visit
Data Analysis
Initial
60% Treated With An Antibiotic (80%)
50% Treated The Same Day (44%)
3% Treated The Next Day (23%)
7% Treated Day 2-5 (13%)
27% Diagnosed With Tonsillitis (16%)
7% Diagnosed with Mononucleosis (6%)
57% Follow Up Phone Calls (59%)
23% Follow Up Visit (22%)
Data Before & After Corrective Action
%
Total Rx with Antibiotic
Treated Same Day
Treated Next Day
Treated Day 2-5
Dx as Tonsillitis
Dx as Mononucleosis
F/U Phone Call
F/U Visit
Before
Corrective
Action
80
44
23
13
16
6
59
22
After
Corrective
Action
60
50
27
7
57
23
3
7
Results
Overall Antibiotic Treatment Decreased
33%
Next Day Treatment Significantly Reduced
From 23% to 3%
Treatment From Day 2-5 Decreased 47%
Same Day Treatment Slightly Increased
From 44% to 50%
Tonsillitis Increased To 68%
Follow Up Phone Calls
Follow Up Visits Down 4%
Performance Goal Comparison
Goal: 70% Treated
Performance: 60% Treated
Goal: 10% Treated/Next Day
Performance 3% Treated/Next Day
Goal: 10% Treated/Day2-5
Performance 7% Treated/Day 2-5
Data Analysis
Improvement and Achievement of Our
Performance Goals
Decreased Antibiotic Usage
This affects antibiotic resistance and has a positive effect on health issues
Improved Quality Of Care
Providing follow up visits on students who were not improving. The only antibiotic provided to students post initial visit were given at the time of follow up office visits by providers
Limitations Of Assessment
Strep C Only/QI Assessment
College Health
Clinical Judgment
Tonsillitis and Mononucleosis
FUTURE STUDY
Comparing Group A Clinical Presentation to Group C Presentation
Centor Criteria
Predictive Method to Diagnosis Strep A
Relationship In Predicting Strep C
Centor Criteria
Set of 4 criteria which may be used to identify the likelihood of a Group A Strep infection in patients complaining of pharyngitis.
It is a method that can be used to quickly diagnosis the probability of Strep A.
Based On 4 Criteria
Fever ≥100.5
Absence Of Cough
Tonsillar Exudate
Tender Anterior Cervical Adenopathy
Centor Criteria
Score 0-1: less than 10% Probability
Not worthwhile to test.
Score 2-3: Intermediate Probability
Score of 2, 15% Prob.
Score of 3, 32% Prob.
RSA test done.
You can follow with a throat cx.
Score 4: 60% Probability
Consider empiric antibiotic Rx.
Some perform a RSA.
Presence of all 4 criteria: 40-60% prob. of GAS present
Absence of all 4 criteria: negative predictive value of greater than 80% GAS not present
High predictive value – Better at ruling out rather than ruling in strep throat.
Centor Criteria/application to testing on students with pharyngitis and Group C
BHS
Pharyngitis/ Centor Criteria EHR
Implementation of guidelines for treatment of Group C BHS in the college population
Throat Facts
8/1/12-5/15/13
Point Of Care
1,425
Rapid Strep In Lab
53
Back Up Throat Cultures In Lab
401