do kill
advertisement

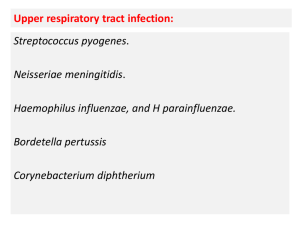
“DO Not Be Snotty: Treatment of Pediatric Upper Respiratory Infections” Stanley E. Grogg, DO, FACOP Professor of Pediatrics OSU-CHS A Common Airway Thus, URIs may include “Colds” Tonsillitis/pharyngitis/laryngitis Otitis media Conjunctivitis Rhinosinusitis What is the most common bacterial infection diagnosed in children? Tonsillitis/pharyngitis Conjunctivitis Pneumonia Rhinosinusitis Acute otitis media Which of the following bacterial organism is NOT a common URI pathogen? Streptococcus pneumonia Haemophilus influenzae, nontypable Moraxella catarrhalis Group A Beta Hemolytic Streptococcus (GABHS) Klebsiella Should be seen by PCP if? Symptoms last longer than 10 days. Severe sore throat, earache, or headache not relieved by Tylenol or ibuprofen. History of tuberculosis, rheumatic fever, kidney disease, or heart disease. Severe chest pain or shortness of breath. You are coughing up thick, green or bloody sputum. You have swollen glands on the sides or back of your neck What is the best way to decrease spread of URIs? 1. See the PCP at the first indication of infection 2. Treat the elevated temperature with antipyretics 3. Use of antibiotics immediately 4. Start OTC antihistamines/decongestants and/or Vitamin C/Echinacea early in the disorder 5. Good hand washing Handwashing and Health Children under 5 years of age in house holds that received plain soap and hand washing promotion had 50% lower incidence of pneumonia Incidence of disease did NOT differ significantly between households given plain soap compared with those given antibacterial soap Luby, SP et al, Lancer 366:225-233, July 16, 2005 How long will cold & flu symptoms last? Fever and sore throat generally improve within 4 days Cough and nasal discharge may last 2 weeks or more Both are caused by viruses, NOT bacteria. Antibiotics DO NOT work Antibiotic and “The Common Cold” Do families of health professional parents prescribe their children with nasopharyngitis antibiotic prescriptions more often than nonhealth professional parents? Huang, N, et. al, Pediatrics Vol. 116, Oct. 2005 http://www.cdc.gov/ncidod/op/antibiotics.htm • Viruses cause • All colds and flu • Most coughs • Most sore throats http://www.cdc.gov/ncidod/op/antibiotics.htm Bacteria cause: Most ear infections Some sinus infections Strep throat Urinary tract infections Antibiotics do kill specific bacteria CAM for Immune Support Echinacea Astragalus (Chinese herb) High-dose Vitamin C Zinc Mind-body strategies Nutrition Exercise Prayer http://nydailynews.healthology.com/nydailynews/14958.htm Manipulative therapy of URI infections in children Case study of over 4,600 incidents of upper respiratory tract infections Only 5% of cases treated with spinal manipulative therapy developed secondary complications. results are superior to those obtained by antimicrobial therapy or symptomatic therapy alone. It would seem unnecessary to use any therapy other than manipulative therapy. Purse FM.; JAOA, 1966 (MAY) Consider Safety-Net Antibiotic Prescription (SNAP) Disadvantages of antibiotics Adverse effects Higher treatment costs Increased bacterial drug resistance Marchetti, F. et al, Arch. Pediatr. Adolesc. Med., July 2005 Criteria for ABX or observation for AOM (AAP/AAFP Guidelines Posted March 9, 2004) Age Certain DX Uncertain DX < 6 mo ABX ABX 6 mo- 2 yr ABX ABX if severe, observe if nonsevere (SNAP?) > 2 yr ABX if severe illness, observe otherwise? ABX for AOM/rhinosinusitis (2004 AAP/AAFP Guidelines) First-line High-dose amoxicillin (90mg/kg for 5- 10 days) Non-type 1 penicillin allergy Cefdinir (Omnicef), cefuroxime (Ceftin) or cefpodoxime (Vantin) Type 1 penicillin allergy Macrolide or sulfonamide Ceftriaxone (1-3 days) if toxic AOM/rhinosinusitis Treatment Failures (2004 AAP/AAFP Guidelines) High dose amoxicillin/clavulanate (Augmentin ES) at 90/mg/kg in bid doses Cefdinir (Omnicef) Cefuroxime (Ceftin) Cefpodoxime (Vantin) Ceftriaxone (50 mg/kg IM qd 1-3 days) Comment: All oral cephalosporins offer comparable efficacy. TX based on other factors such as palatability URIs and Complications In an era of increasing bacterial resistance, it is crucial for PCP’s Make an accurate diagnosis Use antimicrobial agents judiciously Treat the pain Prevention of AOM DO Breast feeding Vaccines Avoid Daycare Smoke Allergens Pacifiers Prophylactic antibiotics What organism is MOST likely to cause AOM with conjunctivitis? 1. Adenovirus 2. Haemophilus influenzae 3. Klebsiella pneumoniae 4. Moraxella catarrhalis 5. Streptococcus pneumoniae 2. Haemophilus influenzae The MOST likely cause of exudative tonsillopharyngitis? 1. Adenovirus 2. Group A betahemolytic streptococcus (GABHS) 3. Coxsachie virus 4. EB Virus 5. Rhinovirus 1. Adenovirus What organism is the MOST likely etiology of pharyngitis-conjunctivitis? 1. Adenovirus 2. Haemophilus influenzae 3. Klebsiella pneumoniae 4. Moraxella catarrhalis 5. Streptococcus pneumoniae 1. Adenovirus Group A Beta Hemolytic Streptococcal (GABHS) Tonsillitis Which of the following symptoms is NOT likely due to GABHS Nausea/vomiting Sore throat Adenopathy Headache Cough/runny nose The MOST important reason to treat GABHS is the following 1. 2. 3. 4. 5. Shorten the coarse of the illness Decrease the carrier state Prevent rheumatic fever Decrease the extension of infection None of the above Match the type of tonsillopharyngitis with the organism Exudative Erythematous Ulcerative Membranous URI symptoms 1. Adenovirus 2. GABHS 3. Coxsachie virus 4. EB Virus 5. Rhinovirus Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infection (PANDAS) Children with multiple streptococcal infections had a markedly increased risk of Tourette’s syndrome (TS) and obsessive-compulsive disorder (OCD) Post-infectious autoimmune phenomenon? Mell et al, Pediatrics, July 2005 T or F: Adenoidectomy and/or Insertion of Tympanostomy Tubes Reduce the incidence of acute otitis media Procedures of adenoidectomy and/or tube insertions have taken on many features of “ritual surgery” Hammaren-Malmi et al, Pediatrics, July, 2005 You are seeing a 6-year-old girl with bilateral conjunctivitis and moderate discharge. Which of the following pathogens is the MOST likely etiologic agent? Adenovirus Haemophilus influenzae Klebsiella pneumoniae Moraxella catarrhalis Streptococcus pneumoniae “Pink Eye” Bacterial conjunctivitis True or False Most children will get better regardless of antimicrobial therapy AAP Grand Rounds, Sept. 2005 3 year old with persistent runny nose and fever of 101 When would you suspect rhinosinusitis URI changes to a “thick yellow” color after 5-7 days Usually good sign What is the best screening test in children for rhinosinusitis? History Physical Facial x-ray MRI CT Scan (limited) “A pill for every ill” Unfortunately, it takes less time and less talk to write a prescription than it does to extol the virtues of observation, patience and analgesia In conclusion MOST upper respiratory infections are viral Amoxil is NOT a good “cough” medicine Fever is GOOD: helps the body stimulate an immune response Treat discomfort with analgesics Rapid Strept tests or throat cultures may be indicated