INSTRUCTION MANUAL
Dementia Care Planning
using
Electronic Care Coordination
May 2014
Prepared for Monash City Council
CONTENTS
1. Project outline
2. Electronic Care Coordination manual
3. Person Centred Approaches material
4. Dementia Management—Key Worker Guide
5. Advance Care Planning Guide
6. PCEHR Planning Guide
7. Gotomeeting Organiser Quick Reference
8. s2s demonstration module guide
9. Your Support Plan – consumer pamphlet
10. Planning the Plan – a guide for practitioners
11. Resource list
All these documents are available on the
Inner East Primary Care Partnership website.
Websit e : www.iepcp.org.au
Prepared for Monash City Council
Project Title:
Dementia Care Planning and Electronic Care Coordination
Version #
Date
1
24 September
2013
2
15 January 2014
Comment (to be completed with each new version
Initial draft to be updated for November 2013 SCAG meeting
This version reflects the current (ongoing) project.
Project Objectives
To improve inter-agency planning and management for clients with dementia
To involve the client and the carer(s) efficiently in the inter-agency care planning process
To use the Electronic Care Coordination (ECC) module to support this.
Project Background
This project has its origins in a number of themes that have been developing in the IEPCP over the past
couple of years. They were:
Developing the practices, processes, protocols and systems (PPPS) for the electronic care
coordination module embedded in the s2s e-referral system
These PPPS are to be found in the Electronic Care Coordination Manual
A thrust to encourage person centred practice
It has become increasingly apparent that dementia is an area in which the IEPCP has done
relatively little apart from the occasional seminar/forum
Dementia is, of course, a major growth area and certain to increase greatly in the foreseeable
future –Alzheimer’s Australia forecasts that three million Australians will develop dementia
between 2012 and 2050i
Monash, Whitehorse and Boroondara and rank third, fourth and fifth in prevalence of
dementia (2013) with Manningham twelfth (out of 79 LGAs in Victoria)ii
The health sector is heavily dependent on carers:
o 2.6 million unpaid carers in Australia iii
o estimated annual replacement value of care provided in 2012 is over $40.9 billioniv
o it is estimated that carers provided 1.32 billion hours of unpaid care in 2010v
There is a recognition in the IEPCP that to date carers have been insufficiently involved in
IEPCP projects
People diagnosed with dementia face multiple challenges including:
o Driving ability
o Legal Issues – e.g. Enduring Powers of Attorney
o Advance Care Planning
o Services, supports and residential care
Department of Health is very interested in increasing use of advance care planning (ACP)
Although dementia does not seem to be a specific target for ACP, the benefits of ACP soon
after diagnosis should be self-evident – this applies both for the client and the carer
There is a strong argument for ‘normalising’ ACP e.g. in Barwon the age of 70 is when clients
are routinely encouraged to draw up an ACP
Eastern Palliative Care is also very interested in having appropriate agency staff draw up ACPs
in great numbers earlier – often clients come to the notice of Eastern Palliative Care too late
for there to be any great benefit from an ACP
Eastern Palliative Care reports that very few of their terminal dementia patients have an ACP
There is provision in the Personally Controlled Electronic Health Records to record the Advance
Care Directive Custodian(s).
The approach to the Service Coordination Operational Plan was re-organised in 2013. It comprises
Goals 1-4, which deal primarily with core service coordination business. Goal 5 lists special projects
that use Service Coordination PPPS. Agencies were asked to register their interest in various strategies
and initiatives and the better management of dementia using ECC was identified as the top priority by
both the Service Coordination Advisory Group and the Practitioners’ Network.
Links with IEPCP Strategic Plan
This initiative is completely in accordance with the IEPCP vision for member agencies to work in
partnership and collaboration to improve the health and wellbeing of our community. The main
guiding principle is Person Centred/Consumer Driven Practice and capacity building applies across
leadership, partnership, workforce, resourcing and advocacy.
Project Benefits
Ensuring the inter-agency care plan is a centrally accessible living document
A more systematic and better organised approach to planning the management of dementia
e.g. drawing up Advance Care Directives
All participants being aware of the plans and actions of others engaged in care of the patient
Case Conference procedures (particularly using Gotomeeting) that optimise client and carer
involvement
Linkages to associated health and support systems e.g. PCEHR, Advance Care Directives
Organisation and governance
The initiative will be managed by a Project Control Group and facilitated by the Inner East PCP. The
Project Control Group will report to the Service Coordination Steering Committee. Membership
consists of the following:
Monash City Council (lead agency)
Sanderson & Associates
Alzheimer’s Victoria
RDNS
Eastern Palliative Care
Villa Maria
Manningham CHS
Christopher Foley-Jones – Facilitator – Inner East PCP
GPs will also probably be involved but are unlikely to want to be on the PCG.
It is envisaged that the PCG meet monthly initially (two meetings), then two-monthly (one meeting)
followed by three-monthly meetings. This phase of the project is scheduled for completion by the end
of calendar year 2014.
Small working parties (2-5 people) were formed to deal with the following:
1. Project design – pathways development/checklist, education, advance care directives etc.
2. Project implementation – client engagement, staff training
3. Technology group – Electronic Care Coordination registration and training, Person Centred
Training and Personally Controlled Electronic Health Records
These meet as determined by the working parties themselves. The IEPCP provides secretarial
functions and continuity to all working parties.
Project stages
1.
Initial planning
2. Project design
3. Technological elements
4. Implementation
5. Evaluation
Project Deliverables
1.
2.
3.
4.
5.
6.
7.
8.
Project outline – this document
Gantt chart
Working party agendas and schedules
Protocols and documentation for participants:
a. Project outline
b. Electronic Care Coordination manual
c. Person Centred Approaches material
d. Dementia Management – Key Worker Guide
e. Advance Care Planning Guide
f. PCEHR Planning Guide
g. Gotomeeting Organiser Quick Reference
h. S2s demonstration module guide
i. Resources list
Training
Implementation
Conference paper on this project
Evaluation report
Geographic catchment area:
IEPCP catchment – focus in first instance on Monash. Following that, Whitehorse and Manningham.
Boroondara at a later date as they will be involved in a related but separate project.
Partners involved
Partners in this project are:
Monash City Council
Sanderson & Associates
Alzheimer’s Victoria
RDNS
Eastern Palliative Care
Villa Maria
Eastern Palliative Care
Manningham CHS
Christopher Foley-Jones of the Inner East PCP will act as facilitator for the PCG and working parties
GPs will also be involved but will probably not be on any working parties.
Timelines
Project commencement October 2013
First PCG meeting October 2013
Second and subsequent PCG meetings – see Gantt chart
Working party meetings – TBD by working parties – suggestions on Gantt chart
Service Coordination Steering Committee meets – 27 November 2013
Progress report early 2014 – for first SCAG meeting in 2014
Conference paper to be presented 22 May 2014
Mid-2014 progress report
Evaluation report November 2014
This phase project to be completed by end 2014
Risk management
Key players may not wish to be involved – initiative can proceed without them but the project
would be diminished.
Initiative may become larger/more complex than originally anticipated. If so, extend timelines.
Finding funding for evaluation – either identify alternative sources or conduct an in-house
version.
BUDGET
No fixed budgetary provision but the IEPCP will cover costs associated with Electronic
Care Coordination e.g. Gotomeeting fees, minor equipment, training costs. Funds may have to be
found for independent evaluation.
Staffing costs
IEPCP and agency time
Start Date: October 2013
Other costs
Training, equipment, possibly evaluation costs
Completion Date: December 2014
Electronic Care Coordination Manual
January 2014
Prepared by:
Date:
Submitted to:
IEPCP Electronic Care Coordination Project Control Group
Manual revised 21 January 2014
IEPCP Service Coordination Advisory Group
Electronic copies available on http://www.iepcp.org.au/member-resources/resources-links
2
Contents
1. Introduction
2. What is Share Care/Case Planning/Electronic Care Coordination?
3. Conditions of use
a. Confidentiality and standards
b. Agency competence
4. Scope
5. Client selection
6. Key Worker selection
7. Client information
a. One Page Profile
b. Thumbnail Sketch
c. Client Background Documentation
8. Plan Writing Guide
9. Inter-agency procedures
10. Case Conferences
11. Gotomeeting webinar package
12. Training program
13. Further information
14. Templates
a. Client Selection Scoresheet
b. Template for inviting non-s2s participants
c. Screenshot of blank Electronic Care Coordination module
Acknowledgments
Members of the Project Control Group who originally developed these procedures and
compiled this manual were:
Christopher Foley-Jones
Kylie Durant
Belinda Johnson
Fiona Macrae
Tony Nossek
Inner East Primary Care Partnership
Manningham Community Health Service
City of Whitehorse
Royal District Nursing Service
Villa Maria
Subsequent amendments have come from a number of sources but particularly Ayesha
Fathers of the City of Monash, Kylie Draper of Eastern Palliative Care and Rod Amos of
Inner East Melbourne Medicare Local. Deb Watson of Sanderson & Associates
contributed information on Person Centred approaches.
3
1. Introduction
This manual sets out procedures for implementing electronic care coordination using the
module developed within the ESCS/s2s e-referral system through the Statewide E-care
Planning Project, which was completed in December 2011. These procedures were
developed by the Inner East Primary Care Partnership Electronic Care Coordination Project
Control Group, which was established for two primary purposes:
To develop procedures setting down how to use the s2s module for the purposes of
inter-agency electronic care coordination
To develop a process to encourage wide-spread use of electronic care coordination,
with appropriate clients, within the IEPCP catchment and beyond.
In doing this, the focus was initially on the most complex clients in the aged care sector.
However, this does not preclude other applications either within the aged care sector or in
other sectors. The mental health sector is one area which frequently plays a particularly
important role for more complex aged care clients.
A pre-condition for obtaining access to the s2s electronic care coordination (ECC) module is
an undertaking that participating agencies will observe the conditions and procedures laid
down in the manual, act in a professional manner and observe all necessary confidentiality
in all matters to do with electronic care coordination.
Note that ECC offers a central information repository accessible, with consent, to all
interested parties. It is the preferred option for inter-agency care coordination to the point
where non-electronic approaches have not been developed as they are seen as far too
cumbersome and requiring too much staff time.
The Infoxchange manual titled ‘s2s eReferral: Quick Reference User Guide – Care Planning’.
contains a more technical description of the Electronic Care Coordination Module and is
recommended reading. The present manual contains the practice-related material
necessary to carry out effective electronic care coordination.
2. What is Shared Care/Case Planning/Electronic Care Coordination?
Shared Care/Case Planning is the term used in the 2012 Victorian Service Coordination
Practice Manual (VSCPM). Previously, this process was known as inter-agency care planning
or care coordination. Here it is referred to as Electronic Care Coordination. Section 3.6 of
the VSCPM contains detailed information on this process – below are a couple of the more
relevant excerpts.
The overall principles of Shared Care/Case Planning include:
a proactive rather than reactive approach for people with multiple support needs
services are planned and delivered, based on best-available evidence in the most
timely and effective way
4
services have in place person-centred practice and a coordinated and integrated
approach
support for consumers to play an active role in co-ordinating their services
providing information on the range of service options available
goal-directed planning
nomination of a main contact person, known as the Key Worker, to support the
Care/Case plan
processes to facilitate communication between all participants
monitoring and review processes
compliance with current legislation and service provider quality standards.
Benefits of Shared Care/Case Planning:
provides consumers with a single point of contact
assists the consumer in setting and achieving goals and enables these to be made known
to all service providers involved
encourages the consumer to be actively involved
manages long-term service delivery in a clear, concise way
provides an essential checklist to ensure continuity of service delivery
provides a way of documenting essential information to be shared by others, including
life saving actions for emergencies
encourages a team approach, with the consumer at the centre
focuses on being proactive rather than reactive
increases consumer and carer awareness of support services available, and how and
when to access them
facilitates effective monitoring of the consumer’s health and social wellbeing, and
diversity needs can be identified and taken into account.
With Electronic Care Coordination, the s2s module provides:
a central, easily accessible information repository
an efficient way of conducting case conferences (on-line).
[The diagram below shows the principles underlying Shared Care/Case Planning or, in this
case, Electronic Care Coordination. Note that this is a diagrammatic representation of the
2012 SCTT Shared Support Plan as adapted for the s2s ECC module.]
5
ELECTRONIC CARE COORDINATION
AGENCY
AGENCY
AGENCY
Interaction
Interaction
Interaction
CARE PLAN
SUMMARY
CARE PLAN
SUMMARY
CARE PLAN
SUMMARY
CLIENT
ONE PAGE PROFILE
KEY WORKER
CARE PLAN
SUMMARY
CARE PLAN
SUMMARY
CARE PLAN
SUMMARY
Interaction
Interaction
Interaction
AGENCY
AGENCY
AGENCY
3. Conditions of use
Confidentiality and standards
Users of the s2s electronic care coordination module are required to observe
the relevant legislation and good practice resources including:
6
•
•
•
•
Information Privacy Act 2006 (Vic)
Health Records Act 2001 No. 2 (Vic)
EMR End User Licence Agreement (EULA) and associated documents
OEHCSA Memorandum of Understanding and IEPCP Memorandum of
Understanding
• Victorian Service Coordination Practice Manual 2012, associated documents
and subsequent releases
• Victorian Department of Health Service Coordination Tool Templates 2012 and
subsequent releases.
• And, in particular, the practices, processes, protocols & systems (PPPS) contained
within this manual.
Agency requirements
In order for clients to be assured of receiving appropriate care and to ensure that other
participating agencies can be confident that a given agency will use the Electronic Care
Coordination Module appropriately, agencies wishing to use the module must:
Participate in training on use of the module and the processes underlying electronic
care coordination - provided by the IEPCP
Undertake to observe the provisions of this Manual
Be certified by the IEPCP as having met the above conditions and then
Be activated as users of the module by Infoxchange.
Note that without activation of the module for a given agency it cannot be used by that
agency.
Also note that in the event of any issues arising in relation to usage of the ECC module, such
issues will be addressed by the IEPCP Service Coordination Advisory Group in the first
instance.
4. Scope
The s2s care coordination module was intended primarily for use by aged care agencies
dealing with more complex clients. Notwithstanding the above, other agencies not in the
aged care sector but who are involved in care of the client may be invited to participate in
care coordination plans. As mentioned earlier, the most obvious need in the case of
complex aged care clients is to be able to interact effectively with the mental health sector.
Agencies must be satisfied, particularly in the case of shared care, that the other agencies
they are dealing with will behave in an appropriate professional manner. A pre-requisite for
use of the module is this appropriate training and competence. When an agency has
achieved this, access to the electronic care coordination module must be activated by
Infoxchange on recommendation by the Inner East Primary Care Partnership.
7
The agencies that will derive the greatest benefit from the module are thus registered s2s
users. Any agency wishing to be involved in ECC may express an interest to the IEPCP to
participate. Non-s2s-users may participate in ECC but will have more limited access to the
module.
5. Client selection
It is recommended that the Client Selection Scoresheet below be used to select clients in
order to target the more complex clients. However, agencies should feel free to use an ECC
plan wherever they consider this to be of benefit to the client.
It is anticipated that only a very small percentage of the total client population will be
beneficiaries of an ECC plan. The purpose of the Shared Support Plan, on which ECC is
based, is to coordinate services for clients who may have a range of characteristics
including:
1. Are being seen by more than one agency and more than one discipline 1
2. Are complex clients2 in that they have multiple issues or problems that need to be
addressed concurrently, and
3. Who are likely to experience a better outcome if the care and services they receive
are coordinated across agencies and over time.
Providing that:
4. The client/carer sees a need or benefit from becoming involved in a formal,
documented inter-agency care coordination process
5. There is sufficient time to put together a thorough care coordination plan i.e. the
client is not in a crisis situation that demands immediate resolution.
Note: The Client Selection Scoresheet overleaf should be regarded as a provisional tool.
Currently the cutoff point at which a client might be considered appropriate for an ECC
plan is 7+. The cutoff point will become clearer when more experience has been gained.
It is therefore recommended that agencies keep scores for ECC clients (using the
Scoresheet) with evaluation and research purposes in mind. It is also recommended that
key workers treat the Client Selection Tool as a resource purely for their own guidance
and do not share it with the client as some elements could be controversial. Note that
clients with dementia may automatically qualify for an ECC plan regardless of their score
on the Scoresheet.
1
Early thinking was that the establishment of a Care Coordination Plan might be triggered when the client was receiving three
or more services provided by two or more agencies – current thinking is that care coordination is required as soon as two or
more services are involved. There are a number of ways in which such care could be coordinated , including using a Care
Coordination Plan. The nature of the client’s situation is more important than the number of services or agencies involved and
will determine what documentation/procedures are required.
2
The Client Selection Scoresheet was developed within the IEPCP to identify a small group of clients with complex needs
using more than one service and for whom setting up an Electronic Care Coordination Plan would be of significant benefit.
8
CLIENT SELECTION SCORESHEET – ELECTRONIC CARE COORDINATION – MAY 2013
1
People using 2 or more services – does not include GPs
2
People with multiple disabilities (health, social, cognitive)
needing assistance in a number of areas of their life
People with frequently changing or fluctuating needs
People from CALD backgrounds where language or cultural
or family expectations means that traditional service
responses are seen as not entirely appropriate, or at least
need modification or, where they are unable to understand
the nature of services being offered
People who have an acute decline in ability to self- manage
People who have experienced a sudden deterioration in
their physical condition
3
4
5
6
7
8
9
10
11
Situation where there are two ‘clients” – the client and the
carer or significant other, both of whom have needs that are
problematic
People who are vulnerable and in reality live alone and have
no effective or immediate support from family or friends,
particularly those with confusion and memory loss
People with behaviours others find difficult and/or don’t
want assistance from services or perceive the need for
assistance when there is objectively a clear need
People with serious psychiatric/psychological issues or
serious intellectual disability
People experiencing elder abuse issues
If the score is 6 or more, client is probably suitable for an ECC plan
Weighting
1
Score
1
1
1
1
1
1 or 2
1 or 2
1 or 2
1 or 2
1 or 2
TOTAL
Note: Where there is an option to score as either 1 or 2, the practitioner is required to
make a judgment call on the severity of the condition concerned. Also note that in some
cases the client’s situation may be sufficiently complex to warrant an ECC plan even though
services are being provided by only one agency.
6.
Key Worker Selection
There has been considerable debate over how a Key Worker should be chosen and what
responsibilities a Key Worker exercises. The Key Worker (as used here):
9
Would normally initiate a care coordination process (however, another worker may
bring an appropriate client to the attention of the Key Worker)
Has the primary task of organising the Care Coordination process including
documentation and case conferences
Provides a central contact for clients, carers and service providers insofar as the
care coordination process is concerned.
Plays a central role in determining the shape of the ECC Plan in that he/she should
write the initial draft of the One Page Profile, which provides the central core on
which the ECC Plan is constructed.
The Key Worker’s responsibilities do not:
Include those of a Case Manager (although the Key Worker may also be a Case
Manager in his/her own right)
Imply any responsibility for ensuring that services provided by others meet the
client’s/carer’s needs
Include providing assistance to clients/carers for day-to-day service access and
general health and welfare issues
Confer any responsibility for or authority over actions of case managers or other
workers who are dealing with the client/carer.
Notwithstanding the above, the Key Worker may also act in his/her own right as a Case
Manager and may provide intensive assistance to clients/carers to navigate the health and
welfare system. However, such functions are not part of the Key Worker role, which is
purely facilitative.
Selection of the Key Worker may arise under one of the three scenarios:
1. The Key Worker may be the case worker for the particular client. In this scenario,
the Key Worker may still remain involved with the client as a service provider.
2. Where there is no case manager. Again, the person who becomes the Key Worker
may provide services in his/her own right.
3. If it is unclear who should act as Key Worker and the client has no preferences, then
the agency willing to perform that function and which is providing the greatest
number of services will act as Key Worker.
4. The client may wish to nominate the Key Worker.
Once the Key Worker has been identified, the next tasks are for the Key Worker:
1. To organise the ECC plan (on s2s) by completing:
a. The One Page Profile
b. Client Background Documentation
c. The ‘Reason for Plan’ (based on a Thumbnail Sketch)
10
d. Preliminary Issues and Goals (in conjunction with the client)
2. Invite participants to any required Gotomeeting webinars or Case Conferences.
3. Organise and chair Case Conferences
[See Section 9 on Inter-agency procedures for step-by-step instructions]
7.
CLIENT DOCUMENTATION
One Page Profile
Thumbnail Sketch
Client Background Documentation
ONE PAGE PROFILE
The One Page Profile (1PP) is the foundation stone of a good Electronic Care Coordination (ECC)
plan. A well-written 1PP will seamlessly lead to an ECC plan that is logical, clear and effective and
easy to put together under the various headings laid down elsewhere in this Manual.
The main defining characteristic of the1PP is its person-centred approach. The writer may use any
client-centred /person-centred tools available but those developed by Sanderson et al. are
particularly user-friendly, simple and thus recommended. Active Service Model principles should
also be observed in writing an ECC plan. Staff trained in the Flinders approach should find the ECC
person-centred format very familiar.
Another defining characteristic of the 1PP is its brevity – it should be no more than one page in
length. The 1PP will contain material that provides a particular focus on aspects that make an ECC
plan meaningful and individualised and will motivate the client towards compliance. This means a
focus on client needs and aspirations rather than on client deficits.
1PPs can be completed at any stage of client care but for ECC purposes we are looking at a relatively
high level 1PP. A 1PP written by a Key Worker will be more general than a later version where a Case
Manager has a more detailed knowledge of the client. What is required is the information necessary
to set up the initial inter-agency care plan, not ongoing day-to-day management.
In broad terms, the 1PP covers what is important to the client. The Clinical Background
Documentation (CBD), which is described below, covers what is important for the client.
Taking into account what is important to the client will make it possible to put into effect the
strategies necessary to achieve what is important for the client. Use the format provided by
Sanderson et al. to draw up the 1PP.
With dementia, for example, the important for items should routinely include setting the plan up as a
hedge against future cognitive incompetence, writing advance care plans, providing carer education,
checking fitness to drive, checking personal security etc. The important to items will determine how
agencies go about achieving those goals. The client may, of course, have a whole set of his/her own
goals important to them.
The Key Worker is responsible for the initial draft of the 1PP, which will be lodged in the
Documentation section on the s2s module very early in the ECC process. Other participants will use
it as a starting point for their conversations with the client and as a source of leads when looking to
11
develop appropriate goals together with matching strategies. Other participants may add
to/amend/correct the 1PP but should always ensure that their changes are clearly identifiable e.g.
using different coloured print.
The 1PP provides essential personal, individualised background information for other participants
while obviating the need for the client to have to repeat their whole story.
THUMBNAIL SKETCH
Thumbnail Sketch
This is a brief paragraph enabling identification of the person as an individual. It should contain basic
demographic information such as (age, marital, COB, residence, major health issues and issues giving
rise to a care plan. See example: Angelina Pomodoro, 53 year old widow of Italian
background, has advanced multiple sclerosis which severely impacts her independence and
enjoyment of community activities. Her aids and equipment currently do not meet her needs.
She also wishes to remain living in her unit but will need additional care and strategies as
her son will be working interstate.
It is always useful for the Key Worker to write out the Thumbnail Sketch as it distils the most
important information about the client into a logical format. It provides the essential information on
which the ECC plan is built and which other participants need to develop their particular strategies.
The Thumbnail Sketch, either in its entirety or abbreviated, should be used to complete the ‘Reason
for Plan’ section on the ECC plan.
Much of the information in the Thumbnail Sketch will be derived from other documentation on file
e.g. Wellness Plans, SCTTs, previous s2s referrals. The Key Worker may either use pre-existing
material such as the Living at Home Assessment Record Template, case notes if in a suitable format
or write a Clinical Background Document (see the following pages). There may also be some
elements drawn from the 1PP.
CLIENT BACKGROUND DOCUMENTATION
The Key Worker may choose to write a Client Background Documentation in its own right or attach
relevant information in the Supporting Documentation area on the s2s module. Those agencies that
complete a Living at Home Assessment Record Template (derived from SCTTs) should include that
as the sole item of Client Background Documentation. Other agencies may wish to attach case notes
if in a suitable format.
Below are elements that should be taken into account when providing Client Background
Documentation (CBD). This is not an all-inclusive list.
EXAMPLE – THUMBNAIL SKETCH AND BACKGROUND DOCUMENTATION
Below is an example of Thumbnail Sketch written using the above guidelines followed by the kind of
background information from which the Thumbnail Sketch would be derived:
Thumbnail sketch*
12
Margarita Mintoff is an 80 year old woman of Maltese descent and has a very good command of
English. She lives with an 82 year old husband with whom she has a very difficult relationship. She
has five grown-up children and has lived in the family home for over 30 years and lived in the area all
her married life. She has multiple health issues including Type 2 diabetes and osteoporosis.
Margarita is experiencing frequent memory loss,some confusion, depression and irritability – it is
strongly suspected that she is suffering early dementia.
………………………………………………………………………………………………………………………………
Current situation*
Living situation, where, with whom, financial issues, conditions etc.
Margarita lives with her husband in a modest house which suffers neglect and disorder but not to
the point of hoarding. An adult son who is has a mental illness lives in a granny flat in the back
garden. She has four other children but they play a minimal role in her care and have little contact.
Her relationship with her husband is very difficult with a great deal of squabbling but no clear
evidence of physical abuse.
Margarita states that her husband’s behaviour worsens throughout the day, and experiences
significant verbal abuse.
Health issues*
Physical and mental health issues including cognition and competence.
Margarita has multiple health issues; a right below the knee amputation, Type 2 Diabetes, peripheral
vascular disease, osteomyelitis in her sacral wound, neuropathic wound to R) 5th toe and rheumatoid
arthritis. She has a history of deep vein thrombosis and osteoporosis.
While Margarita still seems competent to make own decisions regarding finances, health and
wellness and lifestyle this may not be the case much longer.
Supports*
List both agencies and others providing support to the client
RDNS daily visits for wound care
Whitehorse Council provide 3/7 days personal care and home care 1 day per week
Commonwealth Care Respite Centre fund 2/7 personal care
Just for You agency provide 2 hours home support
ADL’s
Margarita needs full assistance with all aspects of personal care, home support and maintenance,
and meal preparation. At present, Margarita can tidy up and complete washing of light dishes.
Margarita has identified that getting meals is difficult for her. She relies on her husband to get her
evening meals for her, however states that often he is ‘unwell’ by the end of the day and unable to
prepare meals. She is also scared she will fall again in the shower.
Mobility
Include personal mobility capacity and constraints and also transport issues.
Margarita ambulates with a prosthetic lower leg and uses a gutter frame indoors and an electric
wheelchair outdoors. Margarita is able to independently transfer with supervision. As Margarita
uses an electric wheelchair to get to church and the local shops, when it is raining these activities are
13
forfeited. Margarita also has a gutter frame which she uses occasionally. She does not like using the
frame, as there is no tray for her to be able to carry items on.
Margarita requires pressure care equipment to maintain skin integrity. She has a high profile ROHO
cushion on her wheelchair,and also has an air mattress which is on loan from Maroondah Hospital
at present. She wishes to be able to have her own air mattress.
***************************
8. Plan Writing Guide
ELECTRONIC CARE COORDINATION – PLAN WRITING GUIDE
The table below is provided to assist in drawing up Electronic Care Coordination Plans. To do this efficiently two components are necessary.
The first is having the skills, relationship and knowledge necessary to fully involve the consumer and clearly identify client needs, wishes and necessary actions.
Recommended tools to do this are to be found in Client-Centred Thinking by Helen Sanderson & Associates. See
http://www.helensandersonassociates.co.uk/reading-room/how/person-centred-thinking.aspx for detailed instructions and tools. Appended to this guide are
examples of some recommended tools. This process should lead to the One Page Profile (1PP), which is the key to good plan writing. Responsibility for writing
the 1PP rests with the Key Worker although all other participants will draw on (and may add to) the 1PP. The various elements that make up a 1PP are
described elsewhere in this Manual.
The second requirement is that the various elements in any care plan be carefully defined so that staff understand what information should go where. Each care
plan has its own particular structure and associated definitions – the definitions below relate to the s2s Electronic Care Coordination module.
ELEMENT AND DEFINITION
EXAMPLES
HINTS AND USEFUL TOOLS
Reason for Plan
While any tools can be used at any stage to gain a
To help me self-manage interactions with the range of
The Reason for Plan should give the
comprehensive understanding of a client’s needs and
services I access for the treatment of my chronic
reader an immediate overview of
situation, the most useful one in the early stages of
obstructive pulmonary disorder and cardiac condition.
why the plan was drawn up and
drawing up a plan is likely to be Important to><Important
what it aims to achieve. This
To put in place techniques for me to self-manage my Type for. In particular, the One Page Profile (1PP) depends on
element should be based on
application of this tool.
2 diabetes and access all necessary services.
knowledge of the particular client
i.e. contain information that can
Relationship circles may also be useful at this point to
To coordinate services necessary to ensure appropriate
only relate to a specific client.
identify who is important in the client’s world. Tip:
management of medication for me by developing
strategies to cope with glaucoma and achieve a degree of include both levels of familiarity and a quadrant approach
This element could be seen as a
to best identify strengths and weaknesses in relationships.
independence and peace of mind.
mapping out of the contents of the
Your agency might use genograms here.
15
ECC plan.
To develop strategies for long-term management of
dementia.
In addition to the tools mentioned above, ‘The Five Whys’
is likely to be useful in working out what the real issues
are. This entails delving ever deeper, by asking ‘Why?’
into each answer a client gives.
‘What’s Working/What’s
not Working’ and ‘Good Days/Bad Days’ are two more
tools that may be useful in sorting out issues. Both of
these are a systematic approach to find out what is
positive and what is negative in a client’s life,
Issues
Issues are the topic or subject that
is pre-occupying the client and/or
are preventing an optimum state of
health and well-being. They are by
nature usually very broad. Issues
address questions such as:
What is it you want to do?
What is it that is bothering you?
What is it that stops you doing
what you want to do?
State issues in the client’s words.
Goals
Goals are what the client would like
to do to address the issue or go
some way towards doing that.
Goals are specific.
Generally goals should be written
A. I want to manage my medications better - glaucoma is
causing problems
B. I am finding it really difficult to shower as I am scared of
falling.
C. The doctor says I am getting dementia and I don’t know
what I can do about it.
A. To be able to take medication every day myself with a
little bit of help from RDNS
B. To be able to shower myself with supervision three times
a week without fear of falling.
16
from the client’s point of view
other than where clearly
inappropriate.
Always try to focus on the positive
i.e. ‘What is it you would like to
improve?’
Outcomes
Outcomes are measures that
enable the client and workers to
know the extent to which goals are
being achieved. They obviously
have to be measurable.
Strategies
Strategies are the broad methods
used to achieve goals and
outcomes. They address the
question of ‘how?’
C. To understand dementia and have a way of dealing with
it.
To feel that only proper people are coming into my home
(carers and friends).
A. I am taking medication on time and as prescribed (under
supervision)
B. I am feeling less anxious when taking a shower.
A1. Use of Webster pack and use of pill bob.
A2. RNDS supervision to be provided for taking medication.
B.1 HACC services to be provided for supervision during
showering.
B2. PADL to be assessed with a view to installing shower
aids.
C. Development and implementation of long-term electronic
care coordination plan addressing dementia in particular.
D. Social worker to liaise with client and family to develop a
strategy for identifying legitimate carers and permitting
access to home.
Outcomes should be SMART –
Specific, Measurable, Achievable, Relevant and Time
Limited.
In developing strategies, ASM principles should always be
kept in mind. The aim should be to develop strategies
based on doing things with the client rather than to the
client and ensuring wherever possible that the client plays
a major role – see the strategies to the left for examples
of this approach.
Tasks should flow naturally from the strategies. If you
have tasks with no corresponding strategy, review your
strategies and maybe even your issues and goals.
Tasks are typically very clear and detailed.
Again note the use of ASM principles.
17
Task
Tasks are the specific actions
needed to ensure strategies are
implemented. They should answer
the questions ‘who, what and
when?’
A1. RN to organise for all client medications to be sent out in
Webster packs from local pharmacy with weekly delivery
(Tuesdays) to client’s home.
A2. RN to prompt and supervise client taking daily
medications from Webster pack.
A3. RN to introduce pill bob to minimise dropping of
medications.
B1. Arrange for HACC service to provide supervision with
showering 3 x week to reduce anxiety levels.
B2. OT to complete bathroom/PADL assessment for
provision of grab rails, shower stool and long handled aids to
reduce fatigue while showering and provide additional
security to enable client to maintain balance while
showering.
9. Inter-agency procedures
INTER-AGENCY ELECTRONIC CARE COORDINATION PROCEDURES 3
KEY WORKER
OTHER PARTICIPANTS
Log on to the s2s e-referral system. Select a service within your agency that has been
authorized to participate in Electronic Care Coordination. Either Search for a new client or
Create one and select Create New Care Plan. To view existing care plans in which you are a
participant, go to Client-Care Plans-My Care Plans.
1. DATES AND REASON SECTION
2. Identify client suitable for ECC
3. Explain procedure and benefits to client. In doing
this begin using the ECC Plan Writing Guide tools
4. Obtain consents
5. Begin putting together the One Page Profile, read
through Client Background Documentation and
write the Thumbnail Sketch.
6. Search for existing client or create new client
7. Select Create New Plan
8. Select ‘Draft’ as status
9. Together with client and using the Thumbnail
Sketch, complete ’Reason for Plan’. Note that this
section gives an overall mapping of the ECC Plan
10. Select ‘Start Date’
11. Select a desired ‘Review Date’ which in the first
instance should be the proposed Initial Case
Conference date. Allow sufficient time for
participants to accept and lodge their care plan
summaries.
12. Together with client, select appropriate ‘Access
Level’.
13. Save Care Plan – this will activate the ‘Activity’ panel
14. INVITING PARTICIPANTS4
15. Together with client, decide who should participate
in the ECC Plan and for what purpose
16. Add Note modeled on the following:
‘This is an invitation to participate in the Electronic
Care Coordination Plan for XXX. You will receive a
separate invitation to participate in the online Case
Conference. Copy this text to be pasted into
Invitations.
17. Make sure you are in the ‘Edit Plan’ mode (top of
screen)
3
These procedures should be read in conjunction with the Infoxchange Manual – s2s e-referral – Quick Reference Guide to Care Plans.
GPs may participate electronically in Care Coordination/Shared Support Plans such as these. This is achieved through the pra ctice being
a fully registered ESCS/s2s user like any other agency or by the practice being set up to interface with the ESCS/s2s system using Argus to
connect directly to their medical software. Another option is to involve GPs using the Gotomeeting webinar – see below for details.
4
19
INTER-AGENCY ELECTRONIC CARE COORDINATION PROCEDURES 3
KEY WORKER
18. Select plan participants by using the ‘Add’ button.
By default, the initiator of the plan will be the Key
Participant.
19. When a participant is added:
Click Give the participant consent to access
information related to this care plan
Click Create an invitation for the participant to
join Care Plan discussion depending how actively
you want the participant to be involved
Paste into the Notes section the text inviting
participation in the Initial Case Conference.
20. For s2s users, check the tick box on the left and
‘Invite’ the participant. The Plan must be saved
before the invitation will be sent to participants.
21. If a proposed participant is not a registered s2s user,
select the ‘Add External Participant’ option and fill
in necessary details. Tick Give the participants
consent to access information related to this care
plan. E-mail invitation to non-participants using the
special template developed for this purpose using
Gotomeeting.5
22. Add the client using the ‘Add External Participant’
option. Tick Give the participants consent to access
information related to this care plan.
23. If a significant other such as a carer is involved, add
that person in the same way as for clients – this will
make it possible to allocate tasks to that person.
24. SUPPORTING DOCUMENTATION
25. Review development of the ECC plan to this point,
finalise the single page One Page Profile and attach
it. See Manual for further details.
26. Using the tabs provided, upload any s2s
transactions that are relevant.
27. Upload Client Background Documentation. This may
be the LaHA Assessment Record Template of
similar. Note that a label is required.
28. GOALS6
29.
5
OTHER PARTICIPANTS
Participants receive e-mail
notifying of invitation to
participate. Access the system and
open the red envelope by your
name (top right hand corner of
screen). Open this and
accept/decline participation. You
will then be shown as Active on
this case.
Non-s2s participants receive email notifying of invitation to
participate. Accept/decline
participation
Review ECC Plan so far and in
particular the One Page Profile
(1PP) and Reason for Plan.
See templates in next section
Note that the goals (care plan summaries) are client-centred, not practitioner-centred, and that they should incorporate ASM principles.
They should therefore be formulated in close consultation with clients.
6
20
INTER-AGENCY ELECTRONIC CARE COORDINATION PROCEDURES 3
KEY WORKER
30. Conduct interviews/assessments as required using
own tools, ECC tools (see below in this Manual) and
1PP Person Centred tools.
31. Complete goals in which the Key Worker, in his/her
professional role, will be involved. Complete all
sections as required. See separate section in this
Manual on Plan Writing
32. Enter or attach any care plan summaries received
from non-s2s participants who wish to be involved.
Where appropriate, use Gotomeeting webinar for
the non-s2s participant to enter their care plan
summary directly into the ECC plan.
33. CASE CONFERENCE
34. Prior to scheduled Initial Case Conference
time/date, read through all goals and consider any
possible amendments, additions, deletions, other
actions required.
OTHER PARTICIPANTS
Conduct interviews/assessments
as required using own tools and
the ECC/ 1PP tools
Participants complete strategies
and tasks for which they, in their
professional role, are responsible.
Complete all sections as required.
See separate section in this
Manual on Plan Writing.
Interested non-s2s participants to
provide care plan summaries to
Key Worker, preferably in the
same format as used in the
module. Care plan summaries may
also be entered directly via a
Gotomeeting webinar involving
the Key Worker and an individual
participant.
Prior to scheduled Initial Case
Conference time/date, read
through all goals and consider any
possible amendments, additions,
deletions, other actions required
35. Arrange for the client/carers to be present during the Client/carers should participate in
Case Conference. This might be at the Key Worker’s the Case Conference wherever
office or preferably, if laptops and Internet access
possible.
are possible, at the client’s home.
36. Conduct Initial Case Conference using Gotomeeting Participate in Initial Case
webinar as scheduled, adjusting individual care
Conference. Note that this will be
plans where necessary and reaching agreement on via a Gotomeeting webinar.
course of action.
37. Complete Overall Assessment and What next?
Sections and obtain signatures.
38. Provide hard copies of Electronic Care Coordination
Plan as required.
39. Schedule a further review date if required. Use the Note review date and take any
‘Schedule a Review’ button at top of ECC plan.
steps required as per Case
Conference.
40. Further review(s) to be conducted as scheduled or if otherwise considered necessary.
21
10.
Case Conferences
Under these procedures there are two kinds of Case Conference.
1. At the Initial Case Conference, participants identified by the Key Worker as
appropriate to the case and who have agreed to participate will discuss the overall
Electronic Care Coordination Plan (ECC plan) and their individual inputs to the ECC
Plan. At this stage, some participating and non-participating agencies may already be
providing services. The goals, strategies and tasks set down will therefore probably
be a mixture of ongoing service provision and planned new service provision.
The Key Worker is responsible for organising the time, date and mode of Case
Conferences. These details should be listed as a Note in the Activity Panel. A typical
Note might read: You are invited to participate in the ECC plan for X. You will receive
a separate invitation to participate in the online Case Conference. Participants may
log on to the system at any time and enter any information in the relevant goals
section. On the module, selection of participants and the sending of invitation by email are automated. The Case Conference date/time is set and invitations are issued
using the Gotomeeting webinar.
Depending on the individual case, the Initial Case Conference may decide that all
necessary steps have been taken, in which case it would set a Nil review and the Key
Worker would close the case. Alternatively, a date may be set for a Review Case
Conference.
2. If a Review Case Conference is scheduled, the Key Worker is again responsible for
advising the date, time and mode of Review Case Conferences in a Note. Review Case
Conferences will be similar to the Initial Case Conference although in this case
progress is being reported on previously decided courses of action. A Review Case
Conference may also arise for the sole reason that there has been a significant
change in the client’s treatment regime or circumstances that warrant further
investigation and discussion.
3. Case Conferences may be held:
Online using the Gotomeeting webinar (the preferred mode) – with or without
videolink
By telephone or conference call
Face-to-face
4. The Key Worker is responsible for documenting the outcomes of Case Conferences
and setting review dates.
22
11.
Gotomeeting webinar package
11.1
Overview
The Gotomeeting webinar package is used for two purposes:
To conduct online case conferences
To engage non-s2s participants in ECC in a meaningful way.
The IEPCP is the holder of a corporate Gotomeeting package. This package allows up to 25
participants to participate in an online meeting, up to six of whom can use a videolink at any one
time. Agencies within the IEPCP region can access the Gotomeeting package, by contacting the
IEPCP. The webinar has applications outside ECC, of course.
Meetings can be set up in two ways – scheduled or unscheduled. Generally ECC meetings will be
scheduled. Below are examples of how Gotomeeting might be used in the ECC application.
11.2
Create Your Organizer Account - Corporate Plan
The IEPCP will invite you to become an organiser. Before being able to schedule or start a meeting,
you need to create your GoToMeeting account and download the GoToMeeting software.
To create your Organiser Account:
1. Open the GoToMeeting invitation email you received from the IEPCP (the administrator)
entitled GoToMeeting Account Confirmation.
2. In the email, click the activation link to create your organizer account.
3. On the Create Account page, enter your information and click Create Account.
4. On the Download GoToMeeting page, click the Download button.
5. If prompted, click Yes, Grant or Trust to accept the download.
11.3
Organising Online Case Conferences
The Key Worker (as Organiser) decides a Case Conference time and date. Ideally this should
be between fifteen minutes and thirty minutes in duration.
The Key Worker uses the automated Gotomeeting invitation facility to schedule the Case
Conference and invite participants. Organisers should right click on the orange daisy at the
bottom right of their screen and follow the prompts.
As shown below, enter ‘Case Conference – Henry Higgins’ in the subject and make the
location ‘Online”.
Amend the telephone number in the e-mail from +61 2 to simply 02
Key Workers must remember to insert their signature block on the e-mail so that
participants can contact them easily.
During the Case Conference the Key Worker can hand over control of the mouse and
keyboard to another participant at any time. However, the Key Worker can override that
control at any time.
The ECC Plan will be on the screen for all to examine. Input can be by microphone,
telephone or (if needs be) using the (typed) chat facility. Participants with a camera on their
computer/laptop who wish to do so can show themselves to others via a videolink.
The Key Worker will enter the outcomes of the case conference discussion with others
watching, including setting a review date (if needed).
23
When all are satisfied that the outcome has been correctly recorded, the meeting ends.
AS A MATTER OF COURTESY AND EFFICIENCY, MEETINGS SHOULD BE HELD WITHIN THE
TIME LIMITS SET.
The procedures outlined above apply to s2s participants. For non-s2s participants, see the following
section.
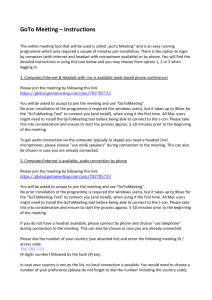
The Gotomeeting invitation should look like this:
11.4 Inviting non-s2s participants
The first step with non-s2s participants is to find out whether, and to what extent, they want to be
involved in the care planning process. The initial approach will probably be via a phone call.
If the non-s2s participant is happy to be involved, issue a Gotomeeting invitation. To do this,
you must be an organiser and have installed Gotomeeting on your computer.
Organisers who have installed Gotomeeting will see a little orange daisy in the system tray
at the bottom right of the screen. Right click on that icon and click on Schedule a meeting.
You may be asked, as a returning user, to verify your ID and password. An e-mail invitation
will pop up automatically. Enter into the e-mail the addressee and paste the following text
in above the Gotomeeting message. Remember to insert your signature block at the
24
bottom of the e-mail. See the appendices of this manual for a template that can be cut
and pasted into the invitation below.
INVITATION TO PARTICIPATE IN AN ELECTRONIC CARE COORDINATION PLAN
An online Case Conference is scheduled as above for:
Name:
Date of birth:
Other agencies/organisations involved include:
If you wish to participate in the Electronic Care Coordination (ECC) Plan, please Accept this
invitation and in your reply indicate which option(s) are of interest:
1. Providing an ECC care plan summary via Gotomeeting. [If you select this option we will
contact you to arrange an appropriate time]
2. Providing a hard copy, not later than one week prior to the Case Conference, of your
input to the undersigned Key Worker, who will be responsible for appropriate formatting.
3. No involvement other than receiving a copy of the Electronic Care Coordination Plan.
Note: Reimbursement for GP participation can be claimed through Medicare items ##729, 747, 750, 758, 872 or 10997 relating to
participating in care plans and reviews organised by others and participation in case conferencing organised by others.
FOR NEW GOTOMEETING USERS
To join a meeting from a GoToMeeting invitation email, a calendar appointment or instant
message invitation
1. Open the email, appointment or instant message that contains the meeting information.
2. Click the Join link provided in the invitation to join the meeting.
3. If prompted, click Yes, Grant or Trust to accept the GoToMeeting download.
You’ll be launched into the meeting where you’ll see your Control Panel and GoToMeeting Viewer.
Leave a Meeting
To leave a meeting
1. From your Control Panel’s File menu, select Exit – Leave Meeting. Or, you also click on your
Control Panel or GoToMeeting Viewer or webcam.
2. When prompted with the Leave Meeting dialog, select Yes.
11.5 Non-s2s participants – lodging care plan summaries
The Key Worker checks that the non-s2s participant has opted to provide an
Electronic Care Coordination care plan summary using Gotomeeting.
The Key Worker will invite them to a Gotomeeting meeting, asking that the participant
nominate an alternative day/time if the meeting proposed is not convenient.
When the meeting has commenced, the Key Worker can give the non-s2s participant control
of the keyboard and mouse so they can edit the care plan (and insert their goals) online.
25
Alternatively, if the participant has elected to provide a hard copy of the care plan summary, this
must be provided to the Key Worker not less than one week prior to the proposed Case Conference
date. In this case it is entirely at the discretion of the Key Worker what information is included in
which sections of the care plan summary. The participant will have the opportunity to make any
corrections during the online Case Conference.
On the first occasion that a participant uses Gotomeeting, they will automatically be asked to install
Gotomeeting on their computer when they accept a Gotomeeting invitation. There is no cost
associated with this and it should take only a minute or two. The Key Worker should advise
potential users of this. Participants should ideally use a microphone and speakers (either inbuilt into
the computer or, even better, as a headset) or using a telephone – in the latter case there will be the
cost of the phone call.
12.
Training
Two different skill sets are required to carry out electronic care coordination efficiently.
One obvious skill set is understanding how the module works in a technological sense. Those skills
are easy to learn as the module is largely intuitive and the instructions provided are clear, simple and
easy to follow.
A much more difficult skill set is creating a coordinated care plan that addresses the person’s needs,
is truly person-centred and is underpinned by professionally competent treatment methodologies.
Professional competence in the sense of discipline-related subject matter is beyond the scope of the
proposed training.
However, all clinicians should of course have basic interviewing skills. In addition, motivational
interviewing skills are particularly useful for the client group who would most often benefit from ECC
plans as poor motivation, goal confusion and uncertainty are very common characteristics. The
Active Service Model emphasis on doing things with the client rather than for the client should also
be borne in mind when developing the plan in conjunction with the client. The person-centred tools
listed earlier in this manual should also be invaluable in formulating a plan that truly involves the
person. In short, proper plan writing requires excellent rapport building.
How the actual information is recorded is also very important, which is why the Plan Writing Guide
has been provided. If that is followed, information will naturally find a home in the appropriate part
of the plan and overall direction should be clear with little duplication of information.
Given the above, it is proposed that the typical training program will use a train-the-trainer approach
and comprise the following:
Session 1 (2 hours)
A brief general introduction to Electronic Care Coordination
The material covered in the manual
o Client selection
o Key Worker selection and role
o Scope
o Confidentiality
o Case Conferences
A short tutorial on use of the s2s module using the ECC procedures in the manual and using
the Gotomeeting webinar.
26
Session 2 (3 hours)
A lengthy session on writing inter-agency care coordination plans including:
o Rapport building
o Person-centred approaches
o Application of ASM principles
o Plan writing skills – with particular reference to the s2s ECC module.
Development of a case study using these techniques
Completion of an ECC plan including an on-line case conference, again using the
Gotomeeting webinar.
13.
Further information
For further information or to make suggestions and provide feedback, please contact:
Christopher Foley-Jones
Coordinator - Systems of Care
Inner East Primary Care Partnership
6 Lakeside Drive
Burwood East VIC 3151
Phone: 8822 8516 Fax (03) 8822 8550 0400 525 792
christopher.foley-jones@iepcp.org.au
*************
27
14.
Templates
The appended templates are both included in the body of this manual and
are provided separately here for easy of copy-and-pasting.
CLIENT SELECTION SCORESHEET – a working document only
CLIENT SELECTION SCORESHEET – ELECTRONIC CARE COORDINATION – MAY 2013
1
People using 2 or more services – does not include GPs
2
People with multiple disabilities (health, social, cognitive)
needing assistance in a number of areas of their life
People with frequently changing or fluctuating needs
People from CALD backgrounds where language or cultural
or family expectations means that traditional service
responses are seen as not entirely appropriate, or at least
need modification or, where they are unable to understand
the nature of services being offered
People who have an acute decline in ability to self- manage
People who have experienced a sudden deterioration in
their physical condition
3
4
5
6
7
8
9
10
11
Situation where there are two ‘clients” – the client and the
carer or significant other, both of whom have needs that are
problematic
People who are vulnerable and in reality live alone and have
no effective or immediate support from family or friends,
particularly those with confusion and memory loss
People with behaviours others find difficult and/or don’t
want assistance from services or perceive the need for
assistance when there is objectively a clear need
People with serious psychiatric/psychological issues or
serious intellectual disability
People experiencing elder abuse issues
If the score is 6 or more, client is probably suitable for an ECC plan
Weighting
1
Score
1
1
1
1
1
1 or 2
1 or 2
1 or 2
1 or 2
1 or 2
TOTAL
Note: Where there is an option to score as either 1 or 2, the practitioner is required to
make a judgment call on the severity of the condition concerned. Also note that in some
cases the client’s situation may be sufficiently complex to warrant an ECC plan even though
services are being provided by only one agency.
28
TEMPLATE FOR INVITING NON-S2S PARTICIPANTS
[Complete and paste in at top of automatically generated Gotomeeting invitation]
INVITATION TO PARTICIPATE IN AN ELECTRONIC CARE COORDINATION PLAN
An online Case Conference is scheduled as above for:
Name:
Date of birth:
Other agencies/organisations involved include:
If you wish to participate in the Electronic Care Coordination (ECC) Plan, please Accept this
invitation and in your reply indicate which option(s) are of interest:
1. Providing an ECC care plan summary via Gotomeeting. [If you select this option we will
contact you to arrange an appropriate time]
2. Providing a hard copy, not later than one week prior to the Case Conference, of your
input to the undersigned Key Worker, who will be responsible for appropriate formatting.
3. No involvement other than receiving a copy of the Electronic Care Coordination Plan.
Note: Reimbursement for GP participation can be claimed through Medicare items ##729, 747, 750, 758, 872 or 10997 relating to
participating in care plans and reviews organised by others and participation in case conferencing organised by others.
FOR NEW GOTOMEETING USERS
To join a meeting from a GoToMeeting invitation email, a calendar appointment or instant
message invitation:
1. Open the email, appointment or instant message that contains the meeting information.
2. Click the Join link provided in the invitation to join the meeting.
3. If prompted, click Yes, Grant or Trust to accept the GoToMeeting download.
You’ll be launched into the meeting where you’ll see your Control Panel and GoToMeeting Viewer.
To leave a meeting:
1. From your Control Panel’s File menu, select Exit – Leave Meeting. Or, you also click on your
Control Panel or GoToMeeting Viewer or webcam.
2. When prompted with the Leave Meeting dialog, select Yes.
5CREEN5HOT OF ELECTRONIC CARE COORDINATION MODULE IN 525
Humpty Horse (20/06/2000),Care Plan
chent onlormatJon
Oates & Reason
Plan Status:
Draft
Reason for Plan:
Start Date:
End Date:
Next Rev ew Date: No REMews Scheduled§ utt A
Access level:
R;v;w=)
Everyone can view the care plan.but only actrve participants can edrt
PartiCipants m ServicesiCare and Support
I
S2S
Name
Role
Organi5ation
Phone
Email
Active
Consent
Homer lnfoxchange
Allied heatth practitioner
Banyute Community Health Service, West
Heidelberg Centre
99999999
homer@infoxchange.net.au
Yes
Yes
I
I
Supporting Documentabon
I
Type
Label
I
I No documentatiOn has been added for th1s care plan.
I II
II
I
Deiete
•S2S Re=d
Attached By
Notes
Added
I
•Attad>ment 11< Lk
Goals
Issue
I
I No goals have been added for this care plan
Goal
Participant Responsible
Outcomes
I
I
Care Plan documented by
Key Participant
Homer lnfoxchange from Banyule Community Health Service,West H e delberg C ...
Approved by key
pan cipant:
f"'
Signed
Signed Date:
Approved by client
rl Signed
Signed Date:
lilJ
or care r:
Reviews
I
Target Date
Summary & Recommendations
I No reviews have been added yet
I j] •Add Hew Rev111w
Delete
Save Care Plan
I
Panicipant Responsibl e
Dec sion
I
I
Introduction to Person
Centred Thinking & One
Page Profiles
Selected material from the
2 day course
This training course was developed by Helen Sanderson Associates.
Person Centred Thinking Tools were developed by The Learning Community for Person
Centred Practices. For more information, including terms of use, go to:
www.learningcommunity.us www.helensandersonassociates.co.uk
Purpose
• To know what is meant by Person Centred
Practice
• Explore a selection of person centred thinking
skills. See how these skills can assist with
developing care plans with people with
dementia
• Think about next steps
Ground Rules
Respect one another’s opinions, listen without
interrupting, share the floor
Mobile phones off or on silent
Misery is optional
No Obsessing – 5 minutes
3
The Learning Community for Person Centred Practices
envisions a world where all people have positive control
over the lives they have chosen for themselves. Our
efforts focus on people who have lost or may lose
positive control because of society's response to the
presence of a disability. We foster a global learning
community that shares knowledge for that purpose. All
are welcome to share and learn.
Service Centred
Person Centred
Service Centred
Person Centred
Planning For
Planning with
Talking about
Talking with
Starting with what’s wrong Starting with what’s
important to people
Health & safety dictate
Health & safety is
where you live/what you
addressed in the context
do/how you do it & with
of where and how you
whom
want to live
Dead plans updated
Living plans which
annually/ as required by
change as required by the
the service or funding
person
body
Person Centred Thinking
underlies and guides respectful
listening which leads to actions. This
results in people who:
– Have positive control over the life they
desire and find satisfying;
– Are recognised and valued for their past,
current and potential contributions to
their communities; and
– Are supported in a web of relationships,
both natural and paid, within their
communities
© TLC-PCP 2012 www.learningcommunity.us
What are person centred
thinking skills?
A set of skills that reflect and reinforce
values that:
– Help us support rather than fix
– Work for humans
– Work at every level of the organisation
– Build the culture of learning,
partnership, and accountability
– Affirm our belief that everyone can learn
& develop
© TLC-PCP 2012 www.learningcommunity.us
Help people get better lives
Not just better plans…
© The Learning Community for Person Centered Practices, Inc. 2008
Management
Skills
Important To
Important For &
The Balance
Between
Everyday
Learning Skills
Discovery/
Listening Skills
© TLC-PCP 2012
www.learningcommunity.us
Discovery/Listening Skills
6 methods for collecting information
Relationship Map
Rituals and Routines
Good Day/Bad Day
Two Minute Drill
Communication Chart
Reputations
© TLC-PCP 2012 www.learningcommunity.us
Going to the
bathroom
Backs away from
the bathroom door
Jenny is anxious
Leave it and
go back later
In the evening
Approaches you
and pulls at her
hair
She wants to go to
bed
Support Jenny
to get ready
for bed (see
her detailed
bedtime
routine)
We need to
respond to
James’
anxiety about
where Ian
(his younger
brother) is.
Ask James where he
saw Ian last – this will
help you understand
roughly what age
James thinks Ian
is/where James is in
time at that point.
If he mentions
something like that he
was ‘helping Dad,’
think of a feasible thing
that Ian could be doing
on the farm with their
father – eg. Went to fix
a fence, had to check a
cow and calf.
Avoid saying Ian is
dead unless you
have tried
everything else.
James may think
Ian is still just a
child. If you have to
say he’s died, say
something like,
“Remember Ian
lived a long &
happy life, and died
peacefully when he
was 82. This may
be like hearing it
for the first time, so
James may need
support to deal
with the news.
Everyday Learning Skills
• 4 + 1 questions
• Learning Log
• Working/Not Working (also called
“What Makes Sense/Doesn’t Make
Sense”)
© TLC-PCP 2012 www.learningcommunity.us
\1\k"at ha.te we tr ied?
4+1
Q's
w-a.
Wlat te.te we lea-ned?
w-a
;;re we pleased <i:xlo..lt?
w-a
next ?
are we COf1Cef"ned abolt ?
Learning Log
y:
e,
Learning Log for Doug (and Mary)
Date
Activity
Who
was
there?
What worked well? What would
you do the same next time?
What didn’t work? What
should be different next
time? What did you learn?
5/9/04
Time at home with
Doug while Mary was
at cards. 12.45 – 4pm
Josie &
Doug
Playing a Beethoven CD and repeating
Beethoven’s 9th when Doug said what a
great tune it is. Making a cup of tea and
suggesting we drink it on the verandah
when Doug started to get anxious. He
was much calmer outside.
Forgetting to have Doug’s walker
ready for him before suggesting we
go outside – he got up immediately
then almost fell and only had me to
hold onto!
12/9/04
As above
Doug &
Sue
Looking at family photos with Doug. He
couldn’t see them, but I could make
guesses or describe them – eg. who’s
this little boy with the blonde hair? He
could then tell stories about his family.
Reading the newspaper to Doug,
he became very worried about
some of the stories and then
worried about them all afternoon –
especially about the salinity levels
of The Murray.
19/9/04
As above
Doug &
Josie
Reading the cattle market reports from
the local paper. Talking with Doug about
our own steers and asking his advice.
Changing the subject to talk about Mary’s
garden when he started worrying about
needing to drench the yearlings.
26/9/04
As above
Doug,
Josie &
Mary (to
start
with)
When Mary didn’t want to go (Doug had
been sick), I didn’t rush her, we had a
cup of tea and I reminded her that she
needed her time away so she could keep
looking after Doug. When she said she
only goes because the family make her, I
agreed that she had better go as they
would be upset with her otherwise, she
then left a little happier.
Playing music later in the afternoon
– Doug held his head a lot, and
said there was a lot of racket going
on. Even though I turned it off, he
grew more and more anxious from
then on. A trip to the toilet followed
by a cup of tea seemed to help.
Not being able to go outside when
Doug grew restless (too cold). We
moved into the kitchen to just get a
change of scene – helped a bit, but
not as good as outside. I will ask
Mary where I can find a blanket
that’s okay to take outside next
time – I know Mary would not like a
good blanket taken out.
Recording Learning for Doug & Mary
What’s Important To Doug?
What’s Important to Mary?
If Doug and Mary are to have a good balance of Important to and for, what do others need to know and do
to support them?
Things to figure out:
rtng
_./(
'DcCiJioMttkiWJ ,
ffqrccMeJ1t
/tMpOrtttl1t ofecis iOI'IS itt M y life
!tow I 111U.!t be ii1IIO/Yeof
------.
Decisions in my life
How I must be involved
Who can help me with this
decision?
Who makes the final
decision
What clothes I wear
Ask me whether I want to wear
dress trousers and shirt or work
shirt and pants. Look at my
calendar and remind me if I have
visitors coming today.
Me
When I go to the doctor
When I’m sick, I need to be told
as soon as possible, and
reminded every hour so there’s
no surprise. I must not miss visits
from family to go to the doctor
District nurses, home care
staff and family. I will refuse to
go if you haven’t involved me!
Who enters my house
I am told a set time when my
house will be cleaned, and the
times staff will be arriving. Always
knowing if it’s a new person.
Home Care coordinators, with
me and family – but, if they
come at the wrong time or it’s
someone I don’t know, I won’t
let them in.
How I spend my money
I need to know about my
expenses each week – this
needs to be written down so I can
decide whether to spoil family
when they visit
Me - but this is dictated by
how many expenses I have
that week. My son talks this
through with me every
Sunday.
Decisions in my life
How I must be involved
Who can help me with
this decision?
Who makes the final
decision
What I eat
Discuss with me the
types of foods & meals
I enjoy
I am offered a choice of
two low sugar meals
and desserts – I decide
which option I will
have.
If I stick to my special
diet
District nurse tells me
daily what my blood
sugar levels are.
May
What time I have my
meals
Not negotiable on days
when it’s carers not
family
Rostering people
When I go out & where I
go
That you listen to me
May and family
when I say I want to go members. Staff when I
out and where, & help
have funding left.
me plan it
Management Skills
• Matching
• The Donut
© TLC-PCP 2012 www.learningcommunity.us
MATCHING
. -0 •
r-rA, r--..
PERSONALITY
CHARACTERISTICS
NEEDED
•SHARED INTERESTS
I
-:a.-. . . .
-
.. ... 1>;_( 9
1\ff.v
Not ovr Paid respo.-.sibWty
I
What you see/hear depends on what you
are looking/listening for
Look/Listen
Understand
© TLC-PCP 2012 www.learningcommunity.us
“…you can’t do this
work with other people if
you have not done it for
yourself…”
John O’Brien, (a long
time ago)
Important TO
What is important to a person includes those
things in life which help us to be content,
comforted, fulfilled, and happy. It includes:
•People to be with /relationships
•Status and control
•Things to do and places to go
•Rituals or routines
•Rhythm or pace of life
•Things to have
© TLC-PCP 2012 www.learningcommunity.us
Important FOR:
•
Issues of health:
― Prevention
& treatment of illness/ medical
conditions
― Promotion
•
of wellness (eg. diet, exercise)
Issues of safety:
― Environment
― Well
being ---- physical and emotional
― Free
from fear
What others see as necessary to help the
person:
― Be
valued
― Be
a contributing member of their
community
© TLC-PCP 2012 www.learningcommunity.us
All choice no responsibility -
to
Health and safety can dictate -
to
balance
for
for
lrrport ant to
\/\.hat else do we nee ::I t o krlO\N or learn?
lrrport ant
for - - - - - - - - - - -- - - --- -
Choose one of the things that is important FOR you (preferably one you avoid or
struggle with), talk with the person next to you about what others may need to
know or do to support you with this. Remember to pay attention to the things that
are Important TO you to see if any of these things can help. Record these tips for
support in the space below, or if they’re work related, on your one page profile.
© The Learning Community for Person Centered Practices, Inc. 2008
What is important to Arthur
How best to support Arthur
/JJ.Nays have his walking stid: within
reach.
That people sit and talk withhim.and
listen to him too - he loves company
and is an amazing storyteller.
Arthur womes that he is very ill and
people are keepingit from him give him lots of reassurance that it
is just oldage -he will have a good
laugh with you then.
That people sit with him when they call
to serve his breakfast dinner and tea
- he dislikes eating alone.He loves hiS
meals to be piping hot
Always explain very clearly to him
about any upcomingappointments
usually at the hospital- do not tell
him at the last minute.
SeeingSally and Stephenevery other
day.
Arthur has very little visionand is
hard of hearing. when youenter
his flat via the keypad code you will
need to call out to Arthur that you
are there.if Arthur is in bednever
approachhim.he willthink you are
a burglar and will hit out With his
walking stid:.
That you listen to his stories.especially
about the war.but never instigate a
conversation around the war - he only
talks about it when he is in the mood.
That you can talk about all the old
boxers wtih him - cassius Clay is
favourite but he will not refer to him as
Muhammed Ali.
Knowing if anythingis happen1ng that is
different from the normalroutine.
Must always have at least £10 inhis
pocket
Must wear his woolbob hat whenhe
wants and not be encouraged to take
it off -he likes wearingit andbecomes
agitated when people suggest he takes
it off in the flat
What those who know Arthur s-v
they like and admire about him
Charming
Salt of the earth.
Arthur is frightened of being 'put
ina home·- tell him that we are all
doing our best to help him stay at
home.but when he goes outside
in the middle of the night we are
frightened he willget hurt.
A real character.
Fullof humour.
A realgent.
Just the most gorgeous gentle man.
Arthur
Deb’s Good Day/Bad Day
Good day
• James eats breakfast without a battle
• I have an achievable to-do list
•
prepared
the night before and manage
to check most things off
• I hear a story about people being
supported to have positive control
• Creating new material with someone
else (HS A or other)
• time planning directly with people
• I don’t need to go shopping for
groceries or attend to other domestic
tasks (on office days I work from home)
Bad day
• lots of tears at childcare and I feel
awful for first couple of hours
• Overwhelmed with admin and
finance tasks
• no food in the house
• ridiculous number of emails to get
through
• hearing about a silly bureaucratic
decision that will have a negative
impact on someone’s life
• I’m scattered and disorganised, and
waste time trying to prioritise
34
Good Day/Bad Day
Good Day During Work Week
Bad Day During Work Week
A really good day
A day that is too challenging
•What happened that
contributed to your good day?
•What do you look forward to
doing?
•What threw your day off?
•Made the day bad for you?
•Made you frustrated? Bored?
•Who do you look forward to
seeing?
• What happens that gives you
energy to deal with difficult
situations?
•Took the fun out of it?
•Be sure to include those daily
frustrations
•What motivates and interests
you at work OR on a work day?
It is a work day. Write down a composite of actual good moments and bad
moments that have happened at anytime a day when you also work.
© TLC-PCP 2012 www.learningcommunity.us
'
Write down a composite of moments that make up a good
and bad day at work
----------.
.. .............................. \Mat ve likeand adnireabout..........................
i
:------------ -------------------·
!
rllXJ r !ant to m ..........................
--------------------------------
1-bwi:Est to 9.4'port . . . . . . . . . . . . .. .
I
r
--- 1······················;
.
n
:
I!
-· :!en
l :l.
I,
;::L .:
......
;
•
;.
:
•
t •••••••••••••••••••••_
0
@
·---
•
•
:
•
Ill
.
,
•
A One (1) Page Profile can be used
• For a specific purpose: for example new situationslike a new job; meeting new people; at the front
of the persons records.
• An at a glance positive way to share key
information about:
• What people like and admire
• What is most important to
• How to best support
All one page profile have these three sections at minimum
To see examples and read stories of one page profiles go to
https://onepageprofiles.wordpress.com/
TLC-PCP 2012
www.learningcommunity.us
-r:p.s - "=r d Vdc::>p/":J y<:::>LLr
=,
?prcn<:/
Li,f and a,d,...;r
Phdo
Thb oction nccdc to be your po::oitivc 'proud' i!ot of
ln!)crt photo into your one
PC:t9to mctke it more
qucdi tiesstrengU1s ctnd tants. Avoid words like
poroona.l.
'uouD.I y" or c timc!i'.
It ::. often helpful to k torunmotco,
·tP. on
friend::;.fam
ily, Writ f.! ynur n.rtnlf-! snmP.WlU
IL"-P. r• lsili vP. ff-!P.dtuu-::k sh.;uf.!lli n
Hrn.Hils nr from the profi e too!
oupcrv ::; on meet ng::; to complete thio ction.
wna.r 's ;
orr
ro
.Sc:>A?
a.r ......
('"at work"' or '"about the project'" can be added to spec
ify the purpo&e of the one pagM)
This &eetion needs to have enough detail that someone who does not know
youcould
unaerstand wnat matters to you,ana It you took tne name onme one page prome you couJa Stil
be identified.
Instead of this
Being organisecl
write this
Being organised - navlng a to cso list tor eacn Clay, us ng me task
l st on Outlook. c-hecking things off as they are completed gives
rne great JOYI
Having fun at work
FUN at work working on creative project!:;; to make the work
HnvirnnmP.n1 tlf!IIP.t.
Going to lunch with coworkcro once o week and laughing
IOQH'lhP.r
WO«.>
ro
.su_p,Porr Soh1ebcx.y aC ...x:>r_f ••.•
Tnls sectionlncluaes lnfotmation tor:
..
wnat is nelp1U
I? wnat s not?
What others can do to make work t me more productive? ros tive?
Specific cu-eet.S you wctnt to identify for support - you may be working on getting better ctt
something (i.e•.time management) and have specific things thel others can do to support
Instead of thi s
Help w1m
staying
organised
I
Write this
Staying organised- 1 onen aver commit my time ana aon't leave
enougn time forlogg ng.If my desk starts to get pUes of paper all over
it.Iam not keeping up wttn my logg ng. A gentle question or - now
are you
don
i g? have you scheduled office time th
is week?"' wiU help me to
re alse 1 neeCI to stop and lOOk at my scneCiule.
If I could, I would…
“If I could, I’d
jump on the
motorbike
and just ride
and ride.”
“I’d love to just
sit by the sea,
watching the
water and
letting the time
go by”
If I could I would………
Write a list of practical things that you
would do if you could?
This could be things you’d like to do more of;
things you have never done but would love to
try; things you used to do but have not done for
a long time
\1\k"at ha.te we tr ied?
w-a.
Wlat te.te we lea-ned?
w-a
I
w-a
;;re we pleased <i:xlo..lt?
next ?
are we COf1Cef"ned abolt ?
Contacts
Deb Watson
Helen Sanderson Associates Australia
0402314323
debw@helensandersonassociates.com.au
www.helensandersonassociates.com.au
Find us on Facebook
The Learning Community for Person
Centred Practices:
www.learningcommunity.us
Websites
www.helensandersonassociates.com.au
www.thinkaboutyourlife.org
www.thinkandplan.com
www.progressforproviders.org
https://onepageprofiles.wordpress.com/
www.celebratingfamilies.co.uk
www.supportplanning.org
www.learningcommunity.us
www.positiveproductivemeetings.com
Issue/action/task
1
2
DEMENTIA MANAGEMENT – KEY WORKER GUIDE
Version: 10 February 2014
1. Awareness,
2. Initial Assessment
3. Management,
4. End of Life
and Diagnosis, and
Care, Support and
Recognition and
Post-Diagnosis
Review
Referral
Support
3
Diagnosis
Identify Key Worker (KW)
Care Planning
Care planning (KW)
4.
5
6
One Page Profile
Client Background Document
Advance care planning
7
8
Decision re competency
Appointment of person
responsible/substitute
Advance Care Directives
MEPOA
Review (GP)/KW
Discuss
Other POA
Register PLWD on PCEHR
GP to download data to PECHR
Register ACD Guardian on PCEHR
Electronic Care Coordination
Set up s2s module
Attach CBD and One Page Profile
Attach ACP, ACD and MEPOA
Identify/invite participants
Collect care plan summaries
Organise and run Case
Provide information (KW)
9
10
11
12
13
14
15
16
17
18
19
20
Referrals for assessment
Lead agency
Assessment and diagnosis
Discuss care planning
Formulate care plan
Discuss (KW)
Discuss (KW)
Discuss (KW)
Write (KW)
Write (KW)
Encourage PLWD/carer to
consider
Review (GP)/KW
Appoint
Implement/review care
plan
Review (KW)
Review (KW)
Review with PLWD/carer
Review (GP)/KW
Review
Assist PLWD/carer (KW)
Advise/assist PLWD/carer
(KW)
Provide information
Assist PLWD/carer (KW)
Encourage GP (KW)
Key Worker to register
Assist PLWD/carer (KW)
Advise/assist
PLWD/carer (KW)
Provide information
Assist PLWD/carer (KW)
Encourage GP (KW)
Key Worker to register
Key Worker
Key Worker
Key Worker
Key Worker
Key Worker
Review (KW)
Review (KW)
Review (KW)
Review (KW)
Review (KW)
Key Worker
Implement/review
care plan
Review (KW)
Review (KW)
Review with
PLWD/carer
Review (GP)
Review
Conference
Issue/action/task
21
22
23
24
25
26
27
28
29
30
31
32
Likely issues/goals for PLWD
Referral to GP to assess
competence
Advance Care Planning
MEPOA
Guardian of Advance Care
Directives (registration)
PCEHR registration
Health issues
Personal (psycho-social) issues
Safety and OHS
Home modifications
Wandering/security
Carer education
Carer Respite/support
Transport
Fitness to drive
Recreation
Provision of services in home
1. Awareness,
Recognition and
Referral
2. Initial Assessment
and Diagnosis, and
Post-Diagnosis
Support
4. End of Life
3. Management,
Care, Support and
Review
Referral (KW)
Address/refer (KW)
Review (KW)
Address (KW)
Review (KW)
Address (KW)
Address /refer (KW)
Address /refer (KW)
Address /refer (KW)
Review (KW)
Review (KW)
Review (KW)
Review (KW)
Address /refer (KW)
Address /refer (KW)
Address /refer (KW)
Address /refer (KW)
Address /refer (KW)
Address /refer (KW)
Review (KW)
Review (KW)
Review (KW)
ADVANCE CARE PLANNING GUIDE
1.
2.
3.
Preliminary reading
Summary referral
chart
Advance care
planning
4.
General
background
5.
Competent>< noncompetent
Writing a care plan
(competent person)
6.
6.
Writing a plan of
care (non-
Version: 10 December 2013
The References at the end of this guide show recommended background reading (listed in descending order of usefulness).
For an overview of possible services see http://www.health.vic.gov.au/hacc/downloads/pdf/dementia_pathways2012.pdf
page 9. For EMR service contact details see http://www.iepcp.org.au/active-service-model-emr-hacc-alliance
Advance Care Planning is a process enabling a person to make decisions about his or her future health care in consultation with
health care providers, family members, and other important people in their lives. A Person Centred Approach should be used to
draw up a plan, which will be attached to the s2s Electronic Care Coordination module and possibly also in an Advance Care
Directive. Note that you should always attempt to do an Advanced Care Plan but that the Person Living With Dementia (PLWD)
may not be willing at this stage to complete an Advanced Care Directive. Inform client/carer that the IEPCP plans to institute
advance care planning for all frail and elderly as a matter of routine. Note that advance care planning is a holistic, long-term
planning process.
Use these links as a guide:
A Brief History Of Advance Care Planning
The law of Advance Care Planning
Things to keep in mind
The ethics of advance care planning
Advance care planning in different healthcare settings
Training to do: Advance Care Planning
Watch Health Professionals Explain Advance Care Planning
Substitute Decision Maker
To decide what form the care plan should take, you need to know whether the PLWD is competent or non-competent. . See
Competence and Capacity for guidance.
‘Starting the conversation’ video at http://www.health.vic.gov.au/acp/ may be a good way to engage clients/carers.
It is recommended that you use the following structure with the client.
1. Thinking about your past health experiences
2. Thinking about your current health and your future medical care
3. Planning your care (taking into account your individual situation)
4. Choosing someone to speak for you (your substitute decision maker)
5. Writing down your wishes
6. Informing others of your decisions
7. Regularly reviewing your Plan
8. Doing advance care planning for a family member / friend
If the PLWD does not have capacity for this process, then the ‘person responsible’ should be consulted and use the dot points
on p. 19 of the ‘Plan of Care’ document on http://www.advancecaredirectives.org.au/pdf/20130605-Plan-of-Care-book.pdf to
7.
competent person)
Advance care
directives background
8.
Medical Enduring
Power of Attorney
9. Medical approvals
10. Lodging of
documents
11. Case Conferences
REFERENCES
Advance Care
Planning
A guide to services
for people with
dementia and their
carers 2012
A Plan of Care
Dementia Services
Pathways
Victorian
Information Leaflet
Take Control
Dementia Services
Directory EMR
formulate the plan.
For Advance Care Directives documents see:
Vic Advance Care Directive - Competent Person
Vic Advance Care Directive - Non Competent Person
Note that the PLWD may not want to complete an Advance Care Directive. In the case of non-competent PLWD, the
carer/person responsible/substitute decision maker should be involved.
Direct PLWD/carers/substitute decision maker to this site if they want to draw up a Medical Enduring Power of Attorney
(MEPOA) Clients/carers can be directed to the ‘Take Control’ kit for further information on POA and guardianship.
Obtain medical signatures on Advanced Care Directives and MEPOA.
1. Attach Advance Care Plan (in dot point format) to s2s electronic care coordination module.
2. Attach Care Plan Directive to s2s electronic care coordination module (if available).
3. Attach MEPOA to s2s electronic care coordination module if appropriate.
4. Register substitute decision-maker/person responsible on PCEHR (if appropriate)
5. Register Advance Care Directive on PCEHR (if appropriate and when this becomes possible).
Participate in Case Conferences as required and be prepared to set review dates for Advanced Care Directives.
http://advancecareplanning.org.au/resources/victoria The main source for brief, readable information and Advance Care
Directives and Medical Enduring Power of Attorney forms and information.
http://www.health.vic.gov.au/hacc/downloads/pdf/dementia_pathways2012.pdf An excellent overview and conceptual
framework
Good guide for handling non-competent persons with dementia and advance care planning generally – NSW document.
http://www.health.gov.au/internet/publications/publishing.nsf/Content/ageing-dementia-services-pathways-2011toc.htm~ageing-dementia-services-pathways-2011-framework.htm Commonwealth document – good overview.
Victorian Information leaflet A useful booklet to give clients a brief overview of Advance Care Directives.
http://www.publicadvocate.vic.gov.au/file/file/Publications/take_control%202012.pdf A kit for making powers of
attorney and guardianship. Make available to clients/carers as required.
http://www.iepcp.org.au/active-service-model-emr-hacc-alliance Contact details for Eastern Metropolitan Region dementia
services.
ADVANCE CARE PLANNING INFORMATION SHEET
Advance care planning is a process for making and writing down future health care
wishes in advance. What you write down in your Advance Care Plan only comes into
effect if and when you become unwell and are unable to make or communicate those
wishes for yourself. It is important to know that medical treatment, including surgery,
should only be given with your fully informed consent and that you have the right to
refuse any treatment. If you become seriously ill, information in your Advance Care Plan
will guide your family and doctor when making medical treatment decisions on your
behalf. The Respecting Patient Choices® Program staff can assist you with advance
care planning.
Advance care planning can include:
1. Appointing a Medical Enduring Power of Attorney (MEPOA)
This is a legal document that allows you to appoint another person (your agent) to make
medical treatment decisions on your behalf, but only if you are not able to make or
communicate decisions for yourself. Your MEPOA is not authorised to make nonmedical (e.g. financial) decisions for you. (Other Powers of Attorney, such as a General
or a Financial Power of Attorney, are not authorised to make medical decisions).
When selecting someone to be your agent, it is important to choose someone 18 years
or older, whom you trust, who knows you well, who is willing to respect your views and
values, who will be a good advocate for you and who is able to make decisions under
circumstances that may be difficult or stressful. Often a family member is a good choice
as an agent, but not always. It is important that the person you select agrees to act as
your agent and that you tell them your preferences regarding future medical treatment.
Please note: your agent cannot be a witness on your MEPOA form. One of the witnesses
must be a person who can sign statutory declarations (e.g. doctor, dentist, pharmacist, a
minister of religion, a lawyer, a justice of the peace).
2. Completing a Refusal of Treatment Certificate (RTC)
In Victoria, if you have a current medical condition, you may give legally binding
directions about medical treatment that you do NOT want by completing a RTC. This
document records your instructions for limiting the treatment of your current illness and
doctors must comply with it when treating you. However, a RTC does not apply to new
medical conditions that may arise later. A RTC enables you to refuse some or all current
and future treatments for your current condition, except palliative care (relief of pain and
suffering). If you become unable to make your own decisions and you have a MEPOA,
then this person (your agent) may also complete a RTC on your behalf.
3. Writing down other wishes for future medical care
You may choose to record your wishes regarding future medical treatments on a
Statement of Choices. This document also enables you to document your health care
values. It is still most important to discuss your wishes with your agent (if appointed),
family and doctor. Ideally your agent should witness your Statement of Choices. The
Statement of Choices is designed to inform your agent, your family and your doctors of
your medical treatment wishes in order to assist them in making decisions if you can no
longer do so for yourself.
Victorian Version. © August 2011 Austin Health
1 of 4
Changing or cancelling advance care planning document(s)
You might want to change or cancel your advance care planning document(s) in the
future if there is a change in your personal or medical circumstances. For example, the
person that you appointed may no longer be the best person for that role, or your goals
for medical treatment may have changed. You can change or cancel these documents
by drawing a line across the document, writing void on it and signing and dating it. These
documents can also be revoked by the completion of new document(s). The most recent
dated document overrides the older document. To revoke the Refusal of Treatment
Certificate, it is advisable to also fill in the cancellation section of the existing certificate. It
is also important to inform your agent, family and your doctors of the changes and
provide them with copies of your new documents.
Your Advance Care Plan may include any / all of the following:
Medical Enduring Power of Attorney
Refusal of Treatment Certificate
Statement of Choices
A written document (signed and dated) outlining your
treatment wishes and/ or your values.
How to do advance care planning
1.
2.
3.
4.
5.
6.
7.
Think about your beliefs, values and your goals for what is important in your life.
Talk to your family and friends about your wishes for health care in the future.
Talk to your GP, hospital doctor or other health professionals and find out more
about your illness and what may occur in the future. Discuss with them your
health care wishes.
If you wish, choose a person to be your agent, and discuss your beliefs, values,
goals, and your wishes regarding medical treatment with them. Ensure that they
understand your viewpoint.
Write down your choices / wishes in an Advance Care Plan.
You need your documents witnessed. One of those witnesses needs to be
your doctor.
If possible, give copies of your documents to the relevant people (in case they
need them in the future); this may include your agent, family or friends, your
doctor or hospital.
Need further information?
Detailed information and help is available for all aspects of advance care planning.
Ask to speak to the Respecting Patient Choices® Consultant at the hospital.
Phone Respecting Patient Choices® Program at
_on:
More information is also available from:
www.advancecareplanning.org.au
www.publicadvocate.vic.gov.au
Or call the Office of the Public Advocate on 1300 309 337
Victorian Version. © August 2011 Austin Health
2 of 4
Statement of Choices
Victoria
A record of my future health care wishes
I,
declare that:
1) My current health problems* include:
of
2) This document has been explained to me and I understand its importance and purpose. I may complete
all or part of this document. It is a guide for my future medical treatment*. It will only be used if I am
unable to make decisions for myself, and will be taken into account when determining my treatment.
3) I understand that it is important to discuss my wishes with my doctor, and my family, including the
’Person Responsible‘ or my Medical Enduring Power of Attorney (if appointed).
4) I request that my wishes, and the beliefs and values on which they are based, are respected. I have
written on page 2 of this form the things that I value most in life, and other things that may help my
doctors and other decision makers.
5) I understand that doctors will only provide treatment that might be medically beneficial. I also understand
that irrespective of any decisions by the doctor about CPR and life prolonging treatment, I will continue
to be cared for, including care to relieve pain and alleviate any suffering.
CPR (Cardiopulmonary Resuscitation) Initial appropriate box
A
It has been explained to me by Dr
CPR and I understand and accept this.
that I would not benefit from attempted
OR
I would like CPR attempted if it might be medically beneficial.
OR
I do NOT want CPR, even if the doctors think it could be beneficial.
AND
Life Prolonging Treatments Initial appropriate box
e.g. breathing machine (ventilator), kidney machine (dialysis), feeding tube, surgery
I would like life prolonging treatment in order to prolong my life as long as possible.
OR
B
I would like life prolonging treatments only if the doctors expect a reasonable outcome. To me, a
reasonable out come means:
OR
I do NOT want life prolonging treatments at all. If life prolonging treatment has been commenced
I request that it be discontinued and that I receive palliative care.
OR
C
I choose to delegate decisions regarding CPR and life prolonging treatments to my Medical Enduring
Power of Attorney or the following person:
(insert name of MEPOA and contact number)
OR
(insert name and relationship)
* If you have specific health problems you may choose to complete a Refusal of Treatment Certificate which is legally binding (unlike the Statement
of Choices which is a guide). Refer to Advance Care Plan Information Sheet.
Victorian Version. © August 2011 Austin Health
3 of 4
The things that I most value in my life are: (eg. independence, enjoyable activities, talking to family and
friends):
Future situations that I would find unacceptable in relation to my health:
Specific treatments that I would NOT want considered for me :
Other things that I would like known, which may help with making decisions about my future medical
treatment:
I ask that, if possible, my Medical Enduring Power of Attorney and / or family include the following people in
discussions and decisions about my health care:
If I am nearing death I would like the following: (for example, music, spiritual care, customs or cultural beliefs
met, family members present):
This is a true record of my wishes on this date.
My Signature
Date
Witness’ signature
(preferably Medical Enduring Power of Attorney)
Witness name (Print)
I, Dr
believe that
(Registered Medical Practitioner)
(your name)
is competent and understands the importance and implications of this document.
Doctor’s signature
Name:
Relationship:
Signature:
Date:
Date
The contents of this Statement of Choices have also been discussed with:
Name:
Relationship:
Signature:
Date:
Victorian Version. © August 2011 Austin Health
4 of 4
ADVANCE CARE PLAN FOR THE NON-COMPETENT PERSON
INFORMATION SHEET
Your family member/friend has been assessed as being unable to make independent
decisions about their own medical care and, therefore, is regarded as non–
competent or not having legal capacity. This, however, may not exclude them from
saying what they do and don’t want for themselves. They may assist you in
completing an advance care plan on their behalf, based on their wishes.
Advance care planning is a process for making and writing down future health care
wishes. It is normally undertaken by competent people, with support from their family
and doctor. If a person is no longer competent, then their family, particularly the
Person Responsible, are able to undertake advance care planning on the person’s
behalf. This ensures that the person only receives treatment that the person would
want and is in the person’s best interests.
The process of advance care planning considers the person’s current state of health,
their beliefs, values and goals in life and their future treatment options. It is important
when completing an advance care plan on behalf of your family member/friend that
you include them, where possible, in these discussions to the best of their ability. A
health professional who is trained in advance care planning, is available to guide you
through the process.
Pre-Existing Advance Care Planning Documents:
1. A previously appointed Medical Enduring Power of Attorney (MEPOA)
If the person has previously appointed a MEPOA (referred to as an agent) the agent
will now become the primary decision maker for medical treatment on behalf of the
non-competent person. A copy of the Medical Enduring Power of Attorney document
should become a part of this advance care plan.
2. A previously completed Refusal of Treatment Certificate (RTC)
The person may have completed a RTC while still competent. If the RTC is valid for
the current illness then the person's refusal of specified treatments, or all treatments,
is legally binding and cannot be overridden by the doctors or others.
3. A Previously Completed Statement of Choices
The person may have previously completed a Statement of Choices (SOC) or a
similar written document expressing their wishes about future medical treatment that
they would, or would not want. Although not legally binding, the doctors and the
family must take the documented wishes into account when making decisions about
medical treatment. You may wish to review previously completed SOC to reflect
current circumstances.
What advance care planning can be done for a non-competent
person?
1. If the person had previously appointed a MEPOA then that agent (usually a
family member or close friend) is able to complete a RTC on the person’s behalf. As
a legally binding document, the RTC can ensure that the person does not receive
unwanted medical treatment or investigation that is related to their current condition.
By law a RTC cannot be used to withhold palliative care (the relief of pain and
suffering).
1 of 4
May 2009
2. If a MEPOA has not previously been appointed then the person’s medical
decision maker, known as the Person Responsible, is identified from a government
list. This is usually a family# member. The Person Responsible can consent, or
withhold consent, to medical treatment offered by the doctor but they cannot
complete a Refusal of Treatment Certificate.
3. Writing down other wishes for future medical care:
As the Person Responsible (the MEPOA, if one exists) you may choose to record the
wishes of the non-competent person on a SOC. In completing a SOC, and
documenting health care wishes, it is important to:
Take into account the person’s previous (and current) health care wishes
Take into account what is in the person’s best interest (including the
benefits and the burdens of possible treatment)
Involve discussion with family and significant others
Discuss these wishes with their doctor(s)
What if a person regains their legal capacity (their competence)?
A person who regains their legal capacity is once again responsible for their medical
decision-making. The agent’s power ceases while the person remains competent.
Changing or cancelling advance care planning documents(s)
You might want to change or cancel the advance care planning document(s) in the
future if there is a change in the person’s medical condition. You can change or
cancel these documents by drawing a line across the document, writing void on it
and signing and dating it. These documents can also be revoked by the completion
of new document(s). The most recently dated document overrides the older
document. To revoke the RTC, it is advisable to also fill in the cancellation section of
the existing certificate. It is also important to inform the important family members
and their doctors of the changes and provide them with copies of the new
documents.
How to do advance care planning for a non-competent person:
1. Think about what their beliefs, values and goals would be at this time
2. Involve family and significant others in advance care planning discussions
3. Talk with their doctor(s) about their current and future state of health and how
this may impact on what they would regard as an acceptable outcome
4. Document their wishes on a SOC
5. These documents will need to be witnessed by their doctor.
6. Give copies of this document to all relevant people who care for your family
member including their doctor(s), aged care facility, family members, and the
hospital
Need further information?
Detailed information and help is available for all aspects of advance care planning.
Ask to speak to the Respecting Patient Choices® Consultant at the hospital.
Phone Respecting Patient Choices® Program at
on:
More information is also available from:
www.respectingpatientchoices.org.au
www.publicadvocate.vic.gov.au
Or call the Office of the Public Advocate on 1800 677 402
#Definition of family: Those closest to the person in knowledge, care and affection. This includes the immediate biological
family; the family of acquisition (related by marriage/domestic partnership); and the family of choice and friends (not related
biologically or by marriage/domestic partnership).
2 of 4
May 2009
Statement of Choices
(Victoria)
SITE
LOGO
For the non-competent person
A record of future health care wishes
This document relates to the following person:_
of
(person’s address)
1) I understand that he/she has been assessed as not having legal capacity to appoint a Medical Enduring
Power of Attorney or make medical decisions independently.
2) This person has the current health problems*:
3) This document has been explained to me and I understand its importance and purpose. I may complete
all or part of this document. It is a guide and will be taken into account when determining future medical
treatment* for this person.
4) I request that this person’s wishes, beliefs and values on which these decisions are based, are
respected. I have written on this form the things that they value most in life, and other things that may
help their doctors and other decision makers.
5) I understand that doctors will only provide treatment that might be medically beneficial. I also understand
that, irrespective of any decisions by the doctor about CPR and life prolonging treatment, he/she will
continue to be cared for, including care to relieve pain and alleviate any suffering.
CPR (Cardiopulmonary Resuscitation) Initial appropriate box
A
It has been explained to me by Dr_
CPR and I understand and accept this.
that he/she would not benefit from attempted
OR
I would like CPR attempted on him/her if it might be medically beneficial.
OR
I do NOT want CPR for him/her even if the doctors think it could be beneficial.
AND
B
Life Prolonging Treatments Initial appropriate box
e.g. breathing machine (ventilator), kidney machine (dialysis), feeding tube, surgery
I would like life prolonging treatment for him/her in order to prolong their life as long as possible
OR
I would like life prolonging treatments for him/her only if the doctors expect a reasonable
outcome. By reasonable outcome I mean:
OR
I do NOT want life prolonging treatments for him/her at all. If life prolonging treatment has been
commenced on him/her I request that it be discontinued and that he/she receive palliative care.
* If you are the MEPOA for the above named person, you may choose to complete a Refusal of Treatment Certificate
which is legally binding (unlike this Statement of Choices which is a guide). Refer to Information Sheet.
3 of 4
May 2009
The things that he/she most values are: (eg. independence, enjoyable activities, family and friends):
Future state(s) of health that he/she would find unacceptable:
Specific treatments I believe he/she would NOT want:
Other things I would like known about him/her which may help with future medical decisions:
If he/she is nearing death I would like the following (for example, music, spiritual care, customs or cultural
beliefs met, family members present):
I
have
hereby
made
choices
based
on
the
best
interests
of
taking into account their wishes, the wishes of family members and
significant others, and the benefits and burdens of treatment. I request that the stated choices recorded
are respected by health professionals, now and in the future.
(insert non competent persons name),
Name
Signature
Date
Relationship to person
I, Dr
MEPOA/Person Responsible
believe that
(Registered Medical Practitioner)
(MEPOA/ person responsible name)
is acting in the best interests of and on behalf of the person stated above. The MEPOA/Person
Responsible understands the importance and implications of this document.
Doctor’s signature
Name:
Relationship:
Signature:
Date:
Date
The contents of this Statement of Choices have also been discussed with:
Name:
Relationship:
Signature:
Date:
4 of 4
May 2009
PCEHR PLANNING GUIDE
1.
Background
2.
3.
4.
Registering PLWDs
5.
Using eHealth record
6.
Version: 28 January 2014
Note that the use of eHealth records is still a fairly new concept, is constantly evolving and its applicability and usefulness will
steadily increase over time.
An eHealth record provides:
personal access to a summary of in individual’s health information that can be viewed via the government
www.eHealth.gov.au website at any time
the ability for individual’s to add appropriate health information to their eHealth record
access to view individual’s Medicare and Pharmaceutical Benefits information
the ability for medical professionals, registered with the eHealth record system, anywhere in Australia to view an
individual’s eHealth record (with the individual’s permission)
emergency access to an individual’s health information if they are incapacitated and unable to provide medical history
In the event of an emergency, staff at a hospital will be able to view a summary of the individual’s medical history, current
medications immunisation and any know alerts/allergies of an individual who has an eHealth record.
For the Dementia and inter-agency care planning project there are four ways in which an eHealth record can benefit a PLWD:
By the Key Worker/Carer/Client registering a basic eHealth record for the PLWD
By the GP uploading patient data on to the individual’s eHealth record (Key Worker to suggest this to GP)
By nominating an Authorised Representative (Guardian/Substitute Decision Maker) on the eHealth record
By nominating the Advance Care Directives custodian on the eHealth record (individual’s will be able to upload their
Advance Care Directives document in the near future).
Key Workers should not expect it to be easy to achieve all the above - achieving any of these points is a significant benefit.
PLWDs/Key Workers/Carers can register the PLWD for a national eHealth record by visiting www.ehealth.gov.au or by
calling 1800 723 471. Answers to some questions about recent Medicare payments or doctor visits will be required.
A unique email address (ie not shared) and MyGov Id are also required if you want to view the eHealth record online.
However, this process is simpler if the Key Worker sends a completed Assisted Registration form into IEMML.
Once the PLWD has been registered and receives their Individual Verification Code (IVC), refer to the blue booklet titled
‘Setting Up Online Access to your eHealth Record’ and follow the simple instructions.
Under ‘Personal’ on the eHealth record, the PLWD (probably with assistance from the Key Worker/Carer) can upload:
Personal Health Note
Personal Health Summary
Details of the Advance Care Directive Custodian
7.
PBS and MBS items
8.
Future access
9.
General Practitioners
10.
Recording on s2s
11.
Further information
Personal Details
Emergency Contacts
PBS and MBS items will be uploaded automatically if you have selected the option to include the last two years of MBS/PBS
items
For future access to the PCEHR the MyGov Id and password are required. Answers to the three secret questions must also be
known. Note that MyGov Id allows PLWDs to link to a number of Government services e.g. Centrelink, Medicare, Veterans
Affairs.
GPs have the option to “Opt-In” as an authorised healthcare provider, so proactive use of the eHealth record is the exception
rather than the rule at this point in time.
When making an appointment;
Ask the Receptionist if their practice can upload eHealth records, if they can, request an extended consultation so that the
GP can prepare and upload the initial Shared Health Summary.
GPs are entitled to claim a higher MBS consultation the first time they upload a Shared Health Summary as they may need
to ‘clean’ up the information in the individual’s record e.g. end dating previous medical history and medication items so
information uploaded reflects the current health status of the individual
Key Workers should not become disheartened if the practice is not registered to the national eHealth record system – the
eHealth record is still very useful without the GP input.
Both as an indication that the PCEHR has been registered and also as a memory aid for the person living with dementia, carer
or service provider, it is suggested that the fact that a PCEHR exists be recorded as follows on the s2s care planning module
under ‘Supporting Documentation’ - + Attachment or Link:
Label – PCEHR TB123456 (this is the client’s myGov Id number)
Click link and enter www.eHealth.gov.au, which will take you to the eHealth website
Under Notes, anything pertinent you think might be useful.
For further information about PCEHR, go to http://publiclearning.ehealth.gov.au/
Contact Inner East Melbourne Medicare Local, eHealth team on (03) 8822 8444
ORGANIZER QUICK REFERENCE GUIDE
GoToMeeting organizers on both personal and corporate plans can hold meetings with up to 25 attendees.
Organizers must first create a GoToMeeting account and then download the GoToMeeting desktop application before
hosting meetings.
Install GoToMeeting
1. From a Windows or Mac, you can practice hosting a meeting by going to www.gotomeeting.com and selecting
Host a Meeting. Or, you can also begin downloading GoToMeeting.
2. Enter your GoToMeeting email address and password, and then click Log In.
3. Click Meet Now to start an instant meeting.
Schedule a Meeting
1. On a Windows, right-click the GoToMeeting daisy icon
in the system tray. On a Mac, double-click the
GoToMeeting Suite icon, and select Schedule a Meeting.
2. On the Schedule a Meeting dialog, enter a subject, date and time, and then select the audio information you
want to provide to your attendees. W hen you’re done, click Schedule.
3. You’ll see a GoToMeeting invitation email appear in your default email client, which you can send to attendees.
Start a Scheduled Meeting
Option 1: Start a meeting from your desktop
1. On a Windows, right-click the GoToMeeting daisy icon
icon or double-click the GoToMeeting Suite icon on a
Mac, and select My Meetings.
2. On the My Meetings dialog, select the meeting you want to start and then click the Start button.
Option 2: Start a meeting from the GoToMeeting website
1.
2.
3.
4.
Log in to www.gotomeeting.com.
On the My Meetings page, locate the scheduled meeting you want to start and click the Start button.
If prompted, click Run, Yes or Always to accept the GoToMeeting download.
You’ll be automatically launched into the meeting where you can use the Control Panel to begin showing your
screen.
Start an Instant Meeting
1. On a Windows, right-click the GoToMeeting daisy icon
in the system tray or double-click the GoToMeeting
Suite icon on a Mac, and select Meet Now.
2. You’ll be automatically launched into the meeting where you can begin hosting your meeting!
End a Meeting
•
•
On a Windows, select the File menu from the Control Panel, and then select Exit – Leave Meeting. Or, you also
click
on your Control Panel or GoToMeeting Viewer or webcam.
On a Mac, select the GoToMeeting menu on Control Panel and then select Quit GoToMeeting. You can also
select the File menu > End Meeting. Or, you can click
on your Control Panel or GoToMeeting Viewer or
webcam.
© 2012 Citrix Online, LLC. All rights reserved.
1
ORGANIZER QUICK REFERENCE GUIDE
Manage Audio
Now you have an extended choice of audio conferencing for your online meetings. With GoToMeeting’s integrated
audio, you can choose to connect to the audio conference using telephone and/or mic and speakers (VoIP).
Note: If you choose to provide your own conference call information for the meeting, GoToMeeting will include your dial-in
numbers with the meeting information; however, GoToMeeting audio features (such as VoIP and integrated audio controls) are
disabled if you choose this option.
VoIP Best Practices
Audio quality can vary based on your audio software, hardware manufacturer and operating system. When using
VoIP, the following best practices are recommended:
•
As with any online meeting solution, it is important to test your sound quality and audio settings before your live
meeting. In addition to testing your audio settings from the GoToMeeting Audio pane, we recommended that you
start your meeting ahead of time with a few test attendees so they can provide feedback on your voice quality.
•
For optimum sound quality, a headset is recommended, preferably a USB headset for ease of use.
•
If a headset is not available, a microphone and speakers are required, preferably a USB microphone for ease of
use.
•
If using a microphone, it should be at least 1.5 feet away from any speakers that are built in or connected to
your computer.
•
Using your webcam’s microphone is not recommended.
•
If you plan to record your meeting, be sure to start your meeting ahead of time and test the Recording feature.
To join the audio portion of the meeting via mic & speakers
1. Expand the Audio pane in your Control Panel.
2. Select Use Mic & Speakers (b)
3. You will be automatically connected into the audio conference over VoIP.
Note: Windows organizers may change the audio input and output from the Audio Preferences tab which is accessed from the File
menu. Mac organizers may manage the audio input and output directly from the Audio pane (c) or from the Audio menu in the
toolbar.
To join the audio portion of the meeting by telephone
1. Expand the Audio pane in your Control Panel.
2. Select Use Telephone (a)
3. Dial in to the conference call with the information provided.
© 2012 Citrix Online, LLC. All rights reserved.
2
ORGANIZER QUICK REFERENCE GUIDE
During a conference call, participants and organizers can enter commands using their phone keypads.
Organizer Telephone Commands
Command
*2
Feature
Count
*3
*4
*5
Exit
Menu
Listening
Modes
*6
*8
Mute/ Unmute
Tone controls
Details
Provides the number of participants currently on the conference
call.
Exits the conference call.
Provides a menu of available conference commands.
Sets listening modes for audience. Pressing *5 sets the following
options: Open conversation mode (default), Mute the audience –
the audience can unmute, Mute the audience – the audience
cannot unmute.
Mutes the organizer’s line. Pressing *6 again will unmute the line.
Sets entry and exit tones. Pressing *8 sets the following options:
Entry and exit tones on (default), Entry and exit tones off, Entry
tone off exit tone on, Entry tone on exit tone off.
Attendee Telephone Commands
Command
Feature
Details
*3
*4
Exit
Menu
Exits the conference call.
Provides a menu of available conference commands.
*6
Mute/ Unmute
Mutes the attendee’s line. Pressing *6 again will unmute the line.
Use Presenter Controls
The Control Panel Grab Tab enables organizers and presenters to collapse the Control Panel to minimize space
when accessing desktops while still being able to access the Grab Tab.
•
Click and drag to move Grab Tab
up or down (a)
•
Hide or display Control Panel (b)
•
Mute or unmute your audio line (c)
•
Share or disable your webcam (d)
•
Share your screen with participants (e)
•
Pause your shared screen so the image
of your desktop remains frozen (f)
Give Keyboard & Mouse button grants
shared mouse and keyboard controls to
another participant (g)
•
•
•
Pass the Presenter Role to another
participant (h)
Draw, highlight and place arrows onscreen, as well as use the spotlight and
clear all markings (Windows only) (i)
© 2012 Citrix Online, LLC. All rights reserved.
3
ORGANIZER QUICK REFERENCE GUIDE
Share Your Webcam
Meeting participants can share up to 6 high-resolution video conferencing streams while viewing the presenter's screen.
You can share your webcam in any of the following ways:
•
•
•
•
•
Click the webcam button
on the Grab Tab.
Click the Share My Webcam button in the Webcam pane on the Control
Panel.
Select Share My Webcam from the Webcams drop-down menu.
Click the webcam button
next to your name in the Attendee List
(Windows-only).
Right-click your own name in the Attendee List and select Share My Webcam.
Manage your webcam from your video feed
•
Temporarily Pause/Play your video by selecting the Pause or Play button on
the top-right corner of your webcam feed. (a)
•
Resize the webcam viewer and screen sharing using the slider. You can click
and drag any part of the slider to adjust the display. (b)
•
When only webcams are being shared, participants can resize webcams by
clicking and dragging the bottom-right corner of the Viewer. Expand and
minimize how webcams and/or screen sharing is displayed by clicking and
dragging the bottom-right corner of the viewer.
If only webcams are being shared (not screen sharing), you can adjust the size
and position of the webcam viewer by using the Webcams drop-down menu
and selecting one of the following Webcam Positions: Top, Left, Bottom,
Right.
© 2012 Citrix Online, LLC. All rights reserved.
4
ORGANIZER QUICK REFERENCE GUIDE
Manage Attendees
Organizers can manage attendees by right-clicking or Ctrl-clicking attendee names in the Attendee List and selecting
or deselecting the desired attendee options.
•
Displays the number of attendees and
maximum number of attendees for
the meeting (a)
•
•
Indicates attendee role and color of
assigned drawing tool (b)
Mute or unmute the attendee (c)
•
Mute or unmute all attendees (d)
•
Assign an attendee with presenter
and/or organizer roles (e)
•
Give keyboard and mouse controls to
an attendee (f)
•
Provide an attendee with on-screen
drawing tools (g)
•
Choose pen color for yourself or your
attendees (h)
•
Allow your attendee to see the list of
other attendees (i)
Allow your attendee to chat (j)
•
•
Send a chat message directly to the
attendee (k)
•
Copy the attendee’s email address to the
clipboard (l)
•
Dismiss an attendee from the meeting (m)
© 2012 Citrix Online, LLC. All rights reserved.
5
s2s demonstration site guide – to access care planning module
1. The s2s demonstration module can be accessed on https://demo.s2s.org.au
2. Login as homer with password infoxchange.
3. Select the role of Allied health practitioner Banyule Community Health Service, West
Heidelberg Centre Occupational Therapy
4. Go Client – Care Plans - My Care Plans
5. Find and open Angelina Pomodoro 158105 – this is on the second page
6. Open the Person Centred Story.
7. Look down the screen at the goals and see how these have been developed from the Person
Centred Story.
[NOTE THAT THE PERSON CENTRED STORY HAS NOW BEEN BROKEN DOWN INTO TWO
COMPONENTS – ONE PAGE PROFILE AND CLINICAL BACKGROUND DOCUMENT.]
9. YOUR SUPPORT PLAN – consumer pamphlet
The embedded Support Plan below is intended for use by people living with dementia and their carers.
The aim is to provide an overview of what is involved in inter-agency care planning for dementia and
electronic care coordination.
Your Support Plan
final.docx
This pamphlet also provides a succinct overview of inter-agency care planning and electronic care
coordination. When printing it off, flip on short side and create a tri-fold document.
/…
10. PLANNING THE PLAN – a guide for practitioners
Remember when writing a plan that it is a long term project. The initial effort will be time-consuming
but you are setting up a plan that should accompany the client throughout his/her journey. Although
the plan is a living document, changes after the initial Case Conference are likely to be incremental
only apart from major changes in health or living situations.
Note that the s2s module is not laid out in a logical fashion as regards inviting participants. Goals
should be worked out before participants are invited, not the other way round.
Also note that it is important how you present care planning to clients. Initially you should speak of
broad benefits or example e.g. kinds of home modifications that can be arranged, meals on wheels,
HACC services, Advance Care Planning, Personally Controlled Electronic Health records, respite,
linking carers in with people who can provide advice and assistance.
The second phase is where you can be more specific about what benefits there could be for the
client/carers/families. It is of a more personal nature e.g. Mary could attend a PAG at XYZ on
Tuesdays, we can help with labelling items in the home, we can arrange overnight respite etc. You will
only be able to do that when you have planned the plan.
The steps for planning a plan are laid out below.
1.
2.
3.
4.
5.
6.
7.
8.
9.
Read and attach L@HA
Write One Page Profile
Formulate Reason for Plan
Set a review time and date for the Initial Case Conference
Create a list of issues. Do this on paper listing issues, possible strategies and who will be
involved. These should include:
a. Personal issues – usually arising from One Page Profile or carers/family – things
important to the client/carers
b. Educational/advice/respite needs for carers
c. HACC services – these will often relate back to their medical needs
d. Advance Care Planning
e. PCEHR
f. Home modifications (physical and management)
g. Other
Prioritise those issues. The first version of the care plan should include immediate issues. You
can note issues for further attention e.g. PCEHR and Advance Care Planning and have the
strategy to pursue those further at the next review date but do not attempt to do to much
immediately.
From your list of issues, work out who will be involved in the care plan and should be invited.
Remember to invite, immediately after the Key Worker, the client and the carer(s).
For s2s members, Add participants and in the notes write ‘You are invited to participate in this
ECC plan – the initial online Case Conference will be at XX time on YY date’. Copy this from the
first invitation so that you can paste it into all subsequent s2s invitations.
For non-s2s members, write in the participant’s name and then enter details in the screen that
pops up.
10. Then use GoToMeeting to Schedule the initial Case Conference. Follow the instructions in the
Manual re pasting the ‘Invitation to Participate in an Electronic Care Coordination Plan’ at the
top of the GotToMeeting invitation. If a GP is involved, schedule a 15 minute Case Conference
and specify that e.g. 10.30-10.45 on Thursday 22 May.
11. Create goals for each issue – ensure goals are small enough to achieve by the next review and
note that they will frequently have to be planned in stages. That is, the initial goal will often
read ‘discuss’ rather that do. The first review might be to further discuss, the second review
to write, the third to place on record etc.
12. Create outcomes for each goal – if you have written a ‘smart’ goal incorporating outcomes,
then just put ‘As above’.
13. Create strategies for each goal
14. Create tasks for each strategy – decide who will do each task and on the importance and
difficulty
15. Collect care plan summaries
16. Hold Case Conference using GoToMeeting
17. Click on the Review (bottom of screen) and then Edit Review.
18. Use the template and drop down lists to record progress and client and participant comments.
19. Be prepared for participants wanting to alter goals, outcomes and target dates. That is their
right – they will often have a better idea of what is achievable than the Key Worker.
20. Write Case Conference summary and set the following review date.
********************
11.
DEMENTIA AND INTER-AGENCY CARE PLANNING
RESOURCE LIST
Participants are invited to submit to info@iepcp.org.au any resources that could be useful for this
project. Remember that we are not looking for every possible item about dementia and its
management but rather documents that distil the main points into a useable format. The ultimate
aim is to produce a simple decision trees, checklists or frameworks that will assist practitioners to
systematically take all necessary steps for the better management of dementia.
1. ‘Dementia Pathways Tool’ – designed primarily for GPs and practice nurses but could be a
useful tool. It may be best as a second level resource i.e. one step removed from a basic
checklist or decision tree. It is a high quality document. Grampians Medicare Local
http://www.grampiansml.com.au/dpp/
2. ‘Dementia Services Pathways’ – main DoHA website on dementia – contains good
background information http://www.health.gov.au/internet/publications/publishing.nsf/Content/ageing-dementiaservices-pathways-2011-toc.htm~ageing-dementia-services-pathways-2011-framework.htm
3. ‘A Guide to services for people with dementia and their carers 2012’, Department of
Health. An excellent overview and conceptual framework – see
http://www.health.vic.gov.au/hacc/downloads/pdf/dementia_pathways2012.pdf
4. An EMR Dementia Services Directory has been drafted and is currently circulating for
comment and feedback.
EMR Dementia
EMR Dementia
Services Directory V6Services Directory V6
5. ‘A Plan of Care’ – described as a book to help people in New South Wales make health and
personal care decisions on behalf of a person with dementia. Treat as background reading.
20130605-Plan-of-C
are-book.pdf
6. ‘Starting the conversation’ – a short introductory DH video on advance care directives.
Could be useful as a quick training tool. http://www.health.vic.gov.au/acp/
7. For Victorian Advance Care Planning templates for both competent and non-competent
persons and also Enduring Medical Power of Attorney template.
http://advancecareplanning.org.au/resources/victoria
8. Refusal of treatment Certificate- competent person. This is contained within the Medical
Treatment Act 1988 http://www.legislation.vic.gov.au/domino/Web_Notes/LDMS/LTObject_Store/LTObjSt6.nsf/
DDE300B846EED9C7CA257616000A3571/6D329679B5FA4D17CA2579FE001CD4EE/$FILE/88
-41aa046%20authorised.pdf
9. ‘Dementia statistics for Victoria’, 2013 report commissioned by Alzheimer’s
Victoria/Australia. Contains detailed information about prevalence and incidence of
dementia down to LGA level. http://www.fightdementia.org.au/victoria/dementiastatistics-for-victoria.aspx
10. ‘IEPCP Electronic Care Coordination Manual. ‘ Sets down the procedures to be followed in
implementing the Electronic Care Coordination Manual including person centred planning.
Electronic Care
Coordination Manual
11. MOOC Dementia Course - 2014
This course is highly recommended.
The University of Tasmania'a Understanding Dementia massive open online course
(MOOC) has attracted 9300 registrations from more than 60 countries, with plans to
continue the course twice a year, starting again next March.
The MOOC, which is a free 11-week course delivered online and requires about three
hours a week of study, covers both the science of dementia and evidence-based strategies
for professional care, is aimed at anyone with an interest in dementia care as well as
healthcare professionals, community and residential facility support staff and people in
the early stages of the disease.
See http://www.utas.edu.au/wicking/wca/mooc for more details and to register for 2014.
12. Health pathways
Here are the links to the Cognitive Impairment / Dementia pathway:
Hunter New England http://trial.healthpathways.org.au/21918.htm
Username: trialHPA
Password: first
Canterbury http://trial.healthpathways.org.nz/21918.htm
Username: trialHP
Password: leap
13. Dementia, Driving and Mobility
http://www.racv.com.au/wps/wcm/connect/racv/Internet/Primary/road+safety/advice+_+inform
ation/drivers+with+a+disability/dementia+and+driving
14. CALD sources
See http://www.seslhd.health.nsw.gov.au/Multicultural_Health/Events/docs/Santalucia.pdf
For overview and further references.
15. Carers and Support
Best single source http://www.fightdementia.org.au/ Useful information particularly for
carers and a general overview of dementia and its management. See Services and Support.
16. At Home with Dementia – a NSW publication with useful tips on what to do to make the
house safe and user-friendly https://www.adhc.nsw.gov.au/ data/assets/file/0011/228746/at_home_with_dementia_
web.pdf Particularly useful for carers.
17. Assisted Living Centre – advice and information on technology http://ilcaustralia.org.au/contact_us/victoria
18. Beyond Life Histories – a HISA resource at Person Centred approaches 201 level. Nine ways
to apply a personalised approach to dementia.
http://www.helensandersonassociates.co.uk/media/86863/beyondlifehistories.pdf
19. http://www.health.nsw.gov.au/dementia/Publications/assessment-mgmt-people-bpsd.pdf
will take you to ‘Assessment and Management of People with Behavioural and
Psychological Symptoms of Dementia (BPSD) - A Handbook for NSW Health Clinicians’.
This is a very comprehensive coverage of dementia and should be of interest to clinicians
with the time to read it or to be used as a reference when problems arise.
20.
i
ii
iii
Dementia Prevalence in Victoria – The Statistics 2013. Alzheimer’s Australia 2013
Dementia Prevalence in Victoria – The Statistics 2013. Alzheimer’s Australia 2013
ABS (2009) Survey of Disability, Ageing and Carers.
Access Economics (2010) The Economic Value of Informal Care in 2010
v Access Economics (2010) The Economic Value of Informal Care in 2010
iv