Iodine Contrast and IVU
advertisement

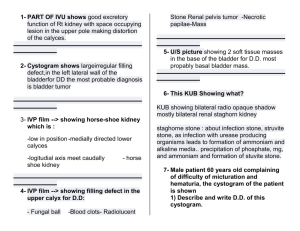
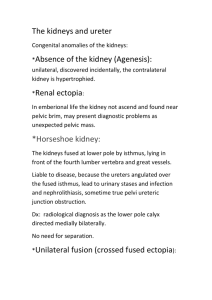
Unit 6 Radiography of the Excretory System RDSC 233 Bontrager pp. 539-574 & Patient Care in Radiography chap. 10. Anatomy of the urinary system Positioning of: Radiographic anatomy Iodinated Contrast Media Tomography Review The Intravenous urogram (IVU) procedure KUB scout LPO & RPO Obliques Cone down of kidneys Post void upright Film Critique Exposure Factors Atlas of Human Anatomy Second edition (313) Need to know Fibrous capsule Upper & lower pole Medial & lateral borders Renal artery and vein Renal pelvis Ureter Ureteropelvic junction (UPJ) (infundibulum) Atlas of Human Anatomy Second edition (313) & Bontrager (543) Cortex * Need to know Renal pyramids (medulla) ** Renal papilla Minor & major calyces (calices) s. calyx * Glomerular and Bowman’s capsule, Glomerulus ** Loop of Henle, renal a & v, collecting tubule Atlas of Human Anatomy Second edition (343) F e m a l e Need to know Body, fundus, & neck of bladder. Mucosal lining, submucosa, muscular & serous layers Ureteral orifice at uereterovesicle junction Internal urethral orifice Trigone of bladder M a l e Urethra (female 4 cm) Prostrate, prostatic urethra & urethra (male 20 cm) Bladder capacity: 250 cc urge to void 700 cc capacity Atlas of Human Anatomy Second edition (248) Need to know Relative position of Kidneys to spine Lt. Upper pole, T11-12 interspace Rt. Lower pole, L3 Ureters (12”) & psoas muscles Iliac crest and inferior poles Lateral border is posterior to medial border Superior pole is posterior to inferior pole Superior pole is medial to inferior pole Radiographic Anatomy Right Renal Arteriogram Radiographic Anatomy of the urinary system Circulation of iodine contrast before the nephron phase (first appearance) of kidney in an IVU nephron “blush” renal a. IVU Tomogram minor calyces catheter cortex Ureter major calyx renal pelvis Ureteropelvic junction (infundibulum) 15 minute KUB with full bladder IVU Tomogram, late nephron phase, collecting system beginning to visualize Upper pole rt. kidney medulla Hilum * Lateral border Lower pole rt. kidney Rt iliac crest cortex * In middle of medial border, superimposed on psoas m. Anatomy Review Contrast Agents January 1896 – First contrast injected into the vascular system of an amputated hand. 1904 – First cystogram. Air (negative contrast) injected retrograde into bladder. 1906 – First retrograde uretrogram using opaque contrast. 1923 – First excretory urography, called a “special procedure” due to the risk associated with the toxic substances used. 1950s – Less toxic, Iodine preperations were introduced under the brand names of Hypaque, Conray, and Renografin. 1986 – Nonionic iodine contrast agents were introduced. 127 Iodine 53 Iodine: atomic number 53. Essential for nutrition, abundant in thyroid. Principle ingredient in the surgical scrub, betadine Non-metallic, commonly found in salt water swamps or brackish waters, in grayish-black, lustrous plates or granules. A halogen (group VII elements including fluorine, bromine, and chlorine), iodine readily binds to salt. Original “ionic” iodine contrasts were bound to sodium or meglumine salt. When injected, the molecule begins to disassociate, releasing ionic particles (+ cation and - anion) at a concentration 4 to 8 times higher than the particle content of blood (Osmolality). Characteristics of Ionic Contrast Iodine concentration determines the radiopacity of the agent. Measured in %weight/volume. Ranges from 10 to 82, dependent on its use. Many products include the concentration of iodine salts in the brand name: Renografin-60, Hexabrix 76, Isovue-200 (20%). See appendix L in Patient Care in Radiography. Water soluable. Unlike barium in suspension, iodine preparations must mix with blood. Stable in solution. The iodine molecule must remain in solution. Products that do not meet this requirement are packages as a solute, and solvent. Low viscosity. The thickness of an agent significantly affects the ease in which a bolus is injected, and the rate of drip infusion. Low toxicity. Any preparation not natural to the body is toxic to some degree, as are natural substances given in excess. The goal of contrast media is to keep adverse reactions to a minimum. Low osmolality. The number of particles in solution is the chief factor of toxicity. The Osmotic Effect 1. As contrast is injected osmolality increases 2. Blood entering the capillary bed is hypertonic to the fluid in the surrounding tissues. 6. Flexibility of vessels walls allow vasodilation to accomodate hypervolemia. 3. Extravascular fluid crosses the semipermeable membrane of the capillary to achieve isotonicity, causing hypervolemia 4. Fluid drawn from RBCs, causes sickling. 5. Epithelial cells lining the intimal wall are similarly effected, and can lead to inflammation and thrombophlebitis Nonionic, low-osmolality contrast agents (LOACs) Quickly became popular in the late 1980s Nonionics do not disassociate into as many particles, and therefore create fewer ions, and less osmolality. The cost is much greater, but comes with the promise of fewer contrast reactions. From Patient Care in Radiography, 5th edition. pg.269. Precautions for the administration of all contrast agents * Check the date on the bottle, ensure correct contrast is chosen * Do not throw bottles away until after exam Contraindications: Glucophage – med for diabetes mellitus. When combined with contrast increases the risk of renal failure. Recommended to be withheld 48 hrs prior to and following contrast administration Multiple myeloma - Malignancy of bone that leads to renal failure, and increases the risk of contrast reactions. Azotemia (uremia)- High levels of nitrogen waste in blood. Laboratory tests BUN (blood urea nitrogen) should be 8 – 25 mg/100 ml. Another test for nitrogen waste, Creatinine levels, should be .6 to 1.5 mg/dl. Contraindications continued: Hypersensitivity to iodine Anuria – no excretion of urine Severe renal disease or failure Congestive heart disease (CHF) Sickle cell anemia Pheochromocytoma – tumor of the kidney In certain cases, an IVU may be performed despite contraindications. Patients should be well hydrated to lessen the risks. Informed Consent What to watch for Reactions can develop quickly, and patients should not be left alone. From Patient Care in Radiography, 5th edition. pg.271. Potential Contrast Reactions (and treatments for) Though the incidence is lessened, reactions to nonionic contrast injections are the same as for ionic agents. Most reactions occur within 5 minutes of injection. Staying calm and reassuring is imperative to the patient’s well being. Mild: metallic taste flushing (slow, deep breathing) nausea vomiting (emesis basin) Moderate: urticaria (benadryl) facial edema transient hypotension headache dizziness diaphoresis chills (blanket warmer) vasovagal (fear of needles) swelling of parotids transient bronchospasm delayed skin reaction (keep patients 20 min) tachycardia Severe: prolonged hypotension/circulatory collapse (Adrenaline [epinephrine] improves cardiac output and relaxes bronchial smooth muscles). pulmonary edema angina (nitroglycerine) severe bronchospasm (adrenaline) cardiac arrest (sodium bicarbonate) arrhythmias (Inderal) convulsions coma paralysis death Radiographic Positioning of the IVU The IVU Procedure Materials Venipuncture contrast (amount dependent on body weight, typically around 100cc) syringes butterfly needles (19 or 21 gauge) venipuncture arm board alcohol wipes tourniquet Reaction supplies emesis basin towels emergency drugs/crash cart Filming lead marker set compression device 10” x 12” & 14” x 17” cassettes gonadal shields positioning sponges The IVU Procedure Because the time it takes for the kidney to excrete the contrast is integral to the diagnosis of function, the IVU exam is timed, and marked on every film. A hypertensive IVU includes films (often tomograms) done at 1, 2, & 3 minutes, or even 30 second intervals. This study is done to determine if hypertension is caused by the kidneys secreting excess renin. Prior to injection a KUB (scout film) is taken to check for technique, the position of the kidneys for the cone down views, the success of the bowel prep, (which is similar to that of a barium enema), and to identify calcifications that might otherwise be obscured by the contrast. Routines are determined by department protocol, but a typical sequence is: 1 min. nephrogram, or nephrotomograms (cone down 10” x 12”) 5 min. supine KUB (or 10” x 12” cone down of kidneys) 10 and/or 15 min. supine KUB 20 min. LPO & RPO obliques Upright postvoid The IVU Procedure The good news is... The scout film is exactly the same as a plain film KUB: The obliques are like colon obliques, except 300, and they include the pubic symphysis (bladder) like a KUB. The upright postvoid is like the upright abdomen, except it is centered like a KUB to also include the bladder. The only unique film is the 10” x 12” cone down of the kidneys for the nephrogram, or more commonly, the tomograms. Routine IVU Positioning Preparation 1. Evaluate the order 2. Greet the patient 3. Take History 4. Have patient void What is pertinent Hx? urinary tract infection, mass, oliguria, renovascular hypertension, renal calculi, elevated creatinine or BUN, hematuria, bladder CA, prostate enlargement, trauma to kidneys, polycystic kidney, malrotation, ectopic kidney 5. Remove jewelry, check attire, snaps, pins, NG tubes, etc. 6. Explain the exam in layman’s terms 7. Questions? 8. Set technique before positioning Centering the Kidneys on a 10” x 12” Sponge, big help for IVUs CR midway between xiphoid tip and iliac crest. Note proximity of the lower pole of the rt. kidney to the iliac crest. Sometimes it is a couple of inches above it, and sometimes it is even lower Lt. Upper pole, T11-12 interspace Lt. Lower pole, L3 (crest is L4-L5 interspace) Note pyloric bulb fulcrum – Physical pivot point objective (focal) plane – plane in space that corresponds to the fulcrum, where the x-ray pivots Linear tomography is routinely used in IVUs. Cut thickness is typically 1 cm. Three levels are required to demonstrate the entire kidney in focus. cut level – distance from the image receptor to the objective plane exposure angle (arc) – The distance the tube travels, measured in degrees. section (cut) thickness – the thickness of the anatomy being imaged that is in the focal plane, and thus in focus. amplitude – the distance the tube travels during its excursion through the exposure angle. Does not effect the cut thickness, only the exposure time. Linear Tomography Finish Vertical Start Start Vertical Finish Localizing the Kidneys (level) for Tomography Divide the measurement of abdomen at the level of the kidneys by three. Start at that cut level and work up. For example, a 27 cm patient would have “tomos” at 9, 10, and 11 cm. 11 cm 10 cm 9 cm Critique criteria for tomographic series 1. The upper and lower poles of both kidneys must be included. 2. Between the three tomographic levels, each kidney should be in focus, in its entirety 11 cm 10 cm 9 cm 11 cm 10 cm 9 cm 11 cm 10 cm 9 cm Perfect Lower pole not in focal plane (started to low) Upper pole not in focal plane (started too high) Focus is approximately here Various focal planes in different patients: Even more evident than the focus of the kidney, is the appearance of the vertebra. These are arranged posterior (1) to anterior (4). 1 2 3 4 LPO and RPO obliques 300 obliques are done to lay the kidney of interest out in profile. In an AP projection the hilum is angled anteriorly. An LPO position best demonstrates the internal collecting system of the rt kidney LPO position Note that the spine is further from the left ureter than the right ureter Right Right Left Left LPO and RPO obliques An RPO is seen here. Note the appearance of the ala of the ilium, and the lt. SI joint. The left kidney is seen in a PA view, but its ureter may be obscured by the spine. The right kidney is obliqued 600 to the film, but its ureter will be free of the spine, and if filled with contrast, well demonstrated. The compression technique (not routine) If the internal collecting system empties too rapidly to be well visualized, the radiologist may request ureteral compression to obstruct the flow of contrast to the bladder. Compression is applied by wrapping a band around the abdomen, securing a set of inflatable balloons over the ureters, and applying enough pressure to create an artificial hydronephrosis. Ureter Balloons The compression technique: Equipment Retention band: wrapped around abdomen, secures the plate and sponge over the balloons. Rigid plate (plexiglass) to apply equalized pressure on sponge Sponge, placed over the balloons Inflation ballons, placed on the abdomen, centered on the ureters. Y Inflation bulb The compression technique There are usually two balloons, though some models have one that is the size of two. With either model the top of the balloons are placed at the level of the iliac crest, and close to touching at the midline. Bontrager p. 371. Contraindications to compression include recent surgery, known abdominal mass, renal calculi, and aortic aneurysm. A 15% trendelenburg is used instead. The compression technique The top of the balloons are placed at the iliac crest, close to touching at midline. The sponge is positioned over the balloons and the plexiglass plate is centered over the sponge. The compression band secures all the parts and is fastened with velcro. The balloons are blown up to compress the ureters. Post void or upright post void The postvoid is typically done as the last film of a routine. It is a standard KUB. It is most often done supine, but may be prone. In addition to the residual contrast that the recumbant film demonstrates, the upright position shows the change in position of the bladder and kidneys, organs that are most susceptable to ptosis In addition to these routine views cone down views of the bladder and obliques may be requested. They will be covered in the unit on cystography. Exposure Factors Techniques for an IVU are the same as for plain films of the abdomen except it is especially important to keep the kVp low to enhance the k-shell characteristic of iodine as much as possible. 70-75 kVp is recommended. Probability of Absorbtion K Shell Binding Energy of 33 keV Iodine 34 keV 32 keV 33 keV Bone Muscle keV The End 30. 31. 32. 33. 34. 35. 36. Name one consequence of the osmotic effect (1 EC) 37. Name a second consequence of the osmotic effect (1EC) 30. Cortex 31. Renal pyramids (medulla) 32. Minor calyces (calices) 33. Upper pole rt. kidney 34. Hilum 35. Lateral border 36. Name one consequence of the osmotic effect (1 EC) 37. Name a second consequence of the osmotic effect (1EC) The Osmotic Effect 1. As contrast is injected osmolality increases 2. Blood entering the capillary bed is hypertonic to the fluid in the surrounding tissues. 6. Flexibility of vessels walls allow vasodilation to accomodate hypervolemia. 3. Extravascular fluid crosses the semipermeable membrane of the capillary to achieve isotonicity, causing hypervolemia 4. Fluid drawn from RBCs, causes sickling. 5. Epithelial cells lining the intimal wall are similarly effected, and can lead to inflammation and thrombophlebitis