Causes of hyponatremia
advertisement

Fluid and Electrolytes
F . Mamdouhi M . D
Mashhad University of Medical
Sciences
اسمواللیته:غلظت ذره یا ماده محلول در یک مایع
اسمواللیته طبیعی پالسما290-275:
اختالالت هموستاز آب :هیپوناترمی یا هیپرناترمی
اختالالت هموستاز سدیم :ادم یا هیپوولمی
The major ECF particles are Na+ and its
accompanying anions Cl– and HCO3–.
The predominant ICF osmoles are K+ and
organic phosphate esters (ATP, creatine
phosphate, and phospholipids).
The normal plasma osmolality (Posm ) is 280
to 295 mosmol/kg.
It usually is held within narrow limits as
variations of only 1 to 2 percent initiate
mechanisms to return the Posm to normal.
These alterations in osmolality are sensed by
receptor cells in the hypothalamus which affect
water intake (via thirst) and water excretion (via
ADH, which increases water reabsorption in
the collecting tubules).
The osmolality of human body fluid is
between 280 and 295 mosmol/kg and
regulated by :
– Vasopressin secretion
– water ingestion, and
– renal water transport.
Hypoosmolality and hyperosmolality can produce serious
neurologic symptoms and death, primarily due to water
movement into and out of the brain, respectively.
To prevent this, the plasma osmolality (Posm ), which is
primarily determined by the plasma Na+ concentration, is
normally maintained within narrow limits by appropriate
variations in water intake and water excretion.
This regulatory system is governed by osmoreceptors in the
hypothalamus that influence both thirst and the secretion of
antidiuretic hormone (ADH).
Vasopressin (AVP) is synthesized in the
hypothalamus.
the distal axons of those neurons project
to the posterior pituitary or
neurohypophysis, from which AVP is
released into the circulation.
AVP has a half-life in the circulation of
only 10–20 min.
AVP secretion is stimulated as systemic
osmolality increases above a threshold
level of 285 mosmol/kg,
Thirst sensation and thus water ingestion
also are activated at 285 mosmol/kg.
Changes in blood volume and blood
pressure are also direct stimuli for AVP
release and thirst.
Water intake
Obligatory water output
هیپوولمی
علل:
از دست دادن اب ازطریق GI
از دست دادن اب از طریق کلیوی
از دست دادن اب از طریق پوست
سکستراسیون به فضای سوم
از دست دادن ازطریق :GI
استفراغ
NG tube
اسهال
فیستول
Only small amounts of water are normally lost in
the stool, averaging 100 to 200 mL/day.
However, gastrointestinal losses are increased to
a variable degree in patients with vomiting or
diarrhea.
The effect of these losses on the plasma Na+
concentration depends on the sum of the Na+
and K+ concentrations in the fluid that is lost.
:از دست دادن از طریق کلیوی
اتالف کلیوی آب
دیابت بیمزه(مرکزی یا نفروژنیک)
اتالف کلیوی آب و سدیم
دیورتیک
دیورز اسموتیک
هیپوآلدوسترونیسم
نفروپاتی از دست دهنده سدیم
The obligatory renal water loss is directly related
to solute excretion.
If a subject has to excrete 800 mosmol of solute
per day (mostly Na+ and K+ salts and urea) to
remain in the steady state, and the maximum
Uosm is 1200 mosmol/kg, then the excretion of the
800 mosmol will require a minimum urine volume
of 670 mL/day.
از دست دادن از طریق پوست:
اتالف نامحسوس
تعریق
سوختگی
The evaporative losses play an important role in
thermoregulation; the heat required for evaporation,
0.58 kcal/1.0 mL of water, normally accounts for 20
to 25 percent of the heat lost from the body, with the
remainder occurring by radiation and convection.
The net effect is the elimination of the heat
produced by body metabolism, thereby preventing
the development of hyperthermia.
Sweat is a hypotonic fluid (Na+ concentration equals
30 to 65 meq/L)
It also contributes to thermoregulation, as the
secretion and subsequent evaporation of sweat result
in the loss of heat from the body.
In the basal state, sweat production is low, but it can
increase markedly in the presence of high external
temperatures or when endogenous heat production is
enhanced, as with exercise, fever, or hyperthyroidism.
As an example, a subject exercising in a hot, dry
climate can lose as much as 1500 mL/h as sweat
سکستراسیون به فضای سوم:
هیپوآلبومینمی
سیروز
سندرم نفروتیک
نشت مویرگی
پانکراتیت حاد
روده ایسکمیک
رابدومیولیز
عالیم هیپوولمی:
خستگی پذیری-ضعف-کرامپ-تشنگی-گیجی
ایسکمی اعضای انتهایی:اولیگوری-سیانوز-درد
شکم-آنژین قلبی-خواب آلودگی
کاهش تورگور پوستی-خشکی غشاهای مخاطی
کاهش فشار ورید ژوگولر-هیپوتانسیون وضعیتی-
تاکیکاردی وضعیتی
تعادل سدیم
%90-85سدیم در بخش خارج سلولی
قرار دارد.
تغییرات غلظت سدیم منعکس کننده بر هم
خوردن هموستاز اب است.
تغییرات مقدار تام سدیم به صورت کاهش
یا افزایش حجم ECFتظاهر می یابد.
دریافت سدیم 150 :میلی مول
دفع سدیم :بستگی به GFRو بازجذب توبولی دارد.
بازجذب سدیم 2/3 :در لوله پروگزیمال – %30-25در
هنله %5 -توبول دیستال -بقیه در مجاری جمع کننده
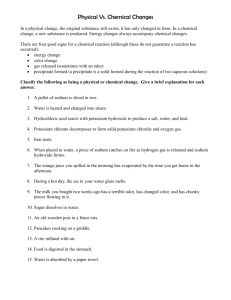
هیپوناترمی
تعریف:سدیم کمتر از 135
علل:
-1هیپوناترمی کاذب
-2هیپوناترمی هیپواسموالر
Hyponatremia
In almost all cases, hyponatremia results from the
intake and subsequent retention of water.
A water load will be rapidly excreted as the dilutional
fall in plasma osmolality suppresses the release of
antidiuretic hormone (ADH), thereby allowing the
excretion of a dilute urine.
The maximum rate of water excretion on a regular
diet is over 10 liters per day.
هیپوناترمی کاذب:
-1اسمواللیته نرمال:
هیپرلپیدمی
هیپرپروتئینمی
پروستاتکتومی
-2اسمواللیته باال:
هیپرگلیسمی
مانیتول
Pseudohyponatremia
Is associated with a normal plasma osmolality,
refers to those disorders in which marked
elevations of substances, such as lipids and
proteins, result in a reduction in the fraction of
plasma that is water.
In normal subjects, the plasma water is
approximately 93 percent of the plasma volume.
A normal plasma sodium concentration of 142
meq/L (measured per liter of plasma) actually
represents a concentration in the physiologically
important plasma water of 154 meq/L (142 ÷
0.93 = 154).
Ion-selective electrodes have been used to
directly measure the plasma water sodium
concentration in this setting but have variable
accuracy.
HYPONATREMIA WITH A HIGH
PLASMA OSMOLALITY
Hyponatremia with a high plasma osmolality is most
often due to hyperglycemia.
A less common cause is the administration and retention
of hypertonic mannitol.
The rise in plasma osmolality induced by glucose or
mannitol pulls water out of the cells, thereby lowering the
plasma sodium concentration by dilution.
Physiologic calculations suggest that the plasma
sodium concentration should fall by 1 meq/L for
every 62 rmg/dL rise in the plasma concentration
of glucose or mannitol (which have the same
molecular weight).
The 1:62 ratio applied when the plasma glucose
concentration was less than 400 mg/dL.
At higher glucose concentrations, the ratio of
1:42 provided a better estimate of this association
than the usual 1:62 ratio
Normal Plasma Osmolality
Isosmotic hyponatremia can be produced by the
addition of an isosmotic (or near isosmotic) but
non-sodium-containing fluid to the extracellular
space.
This problem primarily occurs with the use of
nonconductive glycine or sorbitol flushing
solutions during transurethral resection of the
prostate or bladder or irrigation during
laparoscopic surgery, since variable quantities of
this solution are absorbed.
DISORDERS IN WHICH ADH LEVELS
ARE ELEVATED
The two most common causes of hyponatremia
are:
– effective circulating volume depletion and
– the syndrome of inappropriate ADH
secretion, disorders in which ADH secretion
is not suppressed.
Effective Circulating Volume
Depletion
Significantly decreased tissue perfusion is a
potent stimulus to ADH release.
This response is mediated by baroreceptors in the
carotid sinus and can overcome the inhibitory
effect of hyponatremia on ADH secretion.
Heart Failure and Cirrhosis
Even though the plasma volume may be markedly
increased in these disorders, the pressure sensed at the
carotid sinus baroreceptors is reduced due to the fall in
cardiac output in heart failure and to peripheral
vasodilatation in cirrhosis.
The rise in ADH levels tend to vary with the severity of
the disease, making the development of hyponatremia an
important prognostic sign.
Syndrome of Inappropriate ADH
Secretion
Persistent ADH release and water retention can
also be seen in a variety of disorders that are
not associated with hypovolemia.
These patients have a stable plasma sodium
concentration between 125 and 135 meq/L.
Hormonal Changes
Hyponatremia can occur in patients with adrenal
insufficiency (in which it is lack of cortisol that is
responsible for the hyponatremia) and with
hypothyroidism.
The release of HCG during pregnancy may be
responsible for the mild resetting of the osmostat
downward, leading to a fall in the plasma sodium
concentration of about 5 meq/L.
DISORDERS IN WHICH ADH LEVELS MAY
BE APPROPRIATELY SUPPRESSED
There are two disorders in which hyponatremia
can occur despite suppression of ADH release:
– advanced renal failure
– primary polydipsia
Advanced Renal Failure
The relative ability to excrete free water (free water
excretion divided by the glomerular filtration rate)
is maintained in patients with mild to moderate
renal failure.
Thus, normonatremia is usually maintained in the
absence of oliguria or advanced renal failure.
Advanced Renal Failure
In the latter setting, the minimum urine
osmolality rises to as high as 200 to 250
mosmol/kg despite the appropriate suppression of
ADH.
The osmotic diuresis induced by increased solute
excretion per functioning nephron is thought to be
responsible for the inability to dilute the urine.
Primary Polydipsia
Is a disorder in which there is a primary
stimulation of thirst.
It is most often seen in anxious and in patients
with psychiatric illnesses, particularly those
taking antipsychotic drugs in whom the common
side effect of a dry mouth leads to increased water
intake.
Polydipsia can also occur with hypothalamic
lesions (as with infiltrative diseases such as
sarcoidosis) which directly affect the thirst
centers
Primary Polydipsia
The plasma sodium concentration is usually
normal or only slightly reduced in primary
polydipsia, since the excess water is readily
excreted.
These patients may feel asymptomatic or may
present with complaints of polydipsia and
polyuria.
In rare cases water intake exceeds 10 to 15 L/day
and fatal hyponatremia may ensue.
Symptomatic hyponatremia can also be induced
with an acute 3 to 4 liter water load (as may
rarely be seen in anxious patients preparing for a
radiologic examination or for urinary drug
testing)
Symptomatic and potentially fatal hyponatremia
has also been described after ingestion of the
designer amphetamine ecstasy
(methylenedioxymethamphetamine or MDMA)
Both a marked increase in water intake and
inappropriate secretion of ADH may contribute.
Low ِDietary Solute Intake
Beer drinkers or other malnourished patients may
have a marked reduction in water excretory
capacity.
Normal subjects excrete 600 to 900 mosmol/kg of
solute per day (primarily Na, K salts and urea);
thus, if the minimum urine osmolality is 60
mosmol/kg, the maximum urine output will be 10
to 15 L/day .
Beer contains little or no Na, K , or protein, and
the carbohydrate load will suppress endogenous
protein breakdown and therefore urea excretion.
Diagnosis of Hyponatremia
Hyponatremia in virtually all patients reflects
water retention due to an inability to excrete
ingested water.
In most cases, this defect represents the persistent
secretion of ADH, although free water excretion
can also be limited in advanced renal failure
independent of ADH.
In the absence of renal failure, the differential
diagnosis begins with the history and physical
examination, looking for one of the causes of
excess ADH secretion:
effective circulating volume depletion (including
gastrointestinal or renal losses, congestive
heart failure, and cirrhosis);
the syndrome of inappropriate ADH secretion
(SIADH);
adrenal insufficiency or hypothyroidism.
DIAGNOSIS
Three laboratory findings also may provide
important information in the differential
diagnosis of hyponatremia:
the plasma osmolality;
the urine osmolality;
the urine sodium concentration.
Plasma Osmolality
The plasma osmolality is reduced in most
hyponatremic patients, because it is primarily
determined by the plasma sodium
concentration and accompanying anions.
In some cases the plasma osmolality is either
normal or elevated.
Since there is no hypoosmolality and
therefore no risk of cerebral edema due to
water movement into the brain, therapy
directed at the hyponatremia is not indicated
in any of these disorders with the exception
of glycine administration.
In this setting, the plasma osmolality may fall
with time as the glycine is metabolized.
Urine Osmolality
The normal response to hyponatremia (which is
maintained in primary polydipsia) is to completely
suppress ADH secretion, resulting in the excretion
of a maximally dilute urine with an osmolality below
100 mosmol/kg and a specific gravity < or =1003.
Values above this level indicate an inability to
normally excrete free water that is generally due to
continued secretion of ADH.
اسمواللیته پالسما
طبیعی
پایین
هیپرپروتئینمی
ادرار بسیار حجیم
هیپرلپیدمی
و بسیار رقیق
تحریک مثانه
>100
بله
پرنوشی اولیه
کاهش
< 20
نفروپاتی اتالف
Na
نه
حجم ECF
طبیعی
غلظت Naادرار
باال
هیپرگلیسمی
مانیتول
SIADH
هیپوتیرویئدی
نارسایی آدرنال
>10
دفع خارج کلیوی Na
مصرف طوالنی دیورتیک
افزایش
نارسایی قلبی
سیروز کبدی
سندرم کلیوی
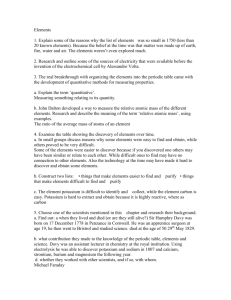
علل :SIADH
بیماریهای عصبی
روانی
ریوی
تومورهای بدخیم
جراحی بزرگ
داروها
hyponatremia due to the SIADH is characterized by the
following set of findings:
– • A fall in the plasma osmolality
– • An inappropriately elevated urine osmolality
(above 100 mosmol/kg and usually above 300
mosmol/kg)
– • A urine sodium concentration usually above 40
meq/L.
– • A relatively normal plasma creatinine concentration
– • Normal adrenal and thyroid function.
عالئم :SIADH
هیپوناترمی +هیپواسمواللیتی
100>Uosm
40>UNa
نرموولمی
فانکشن کلیه – آدرنال -تیرویید نرمال
اسید – باز – پتاسیم نرمال
هیپواوریسمی
Plasma Uric Acid and Urea
Concentrations
The initial water retention and volume expansion
in the SIADH leads to another frequent finding
that is the opposite of that typically seen with
volume depletion: hypouricemia (plasma uric
acid concentration less than 4 mg/dL ) due to
increased uric acid excretion in the urine.
It is presumed that the early volume expansion
diminishes proximal sodium reabsorption,
leading to a secondary decline in the net
reabsorption of uric acid.
Cerebral Salt Wasting
All of the changes in electrolyte balance observed
in the SIADH have also been described in the
putative syndrome of cerebral salt-wasting.
This disorder is characterized by a high urine
sodium concentration that is due to defective
tubular reabsorption (mediated by the release of
a natriuretic hormone, perhaps brain natriuretic
peptide) and an elevation in ADH and the
subsequent development of hyponatremia due to
the associated volume depletion.
Symptoms of Hyponatremia
The symptoms that may be seen with
hyponatremia or hypernatremia are
primarily neurologic and are related both
to the severity and in particular to the
rapidity of onset of the change in the
plasma sodium concentration.
Symptoms of Hyponatremia
The symptoms directly attributable to
hyponatremia primarily occur with acute and
marked reductions in the plasma sodium
concentration and reflect neurologic
dysfunction induced by cerebral edema .
In this setting, the associated fall in plasma
osmolality creates an osmolal gradient that
favors water movement into the cells,
leading in particular to brain edema.
The presence of cerebral overhydration
generally correlates closely with the severity
of the symptoms.
Nausea and malaise are the earliest
findings, and may be seen when the plasma
sodium concentration falls below 125 to 130
meq/L.
This may be followed by headache, lethargy,
and obtundation and eventually seizures,
coma and respiratory arrest if the plasma
sodium concentration falls below 115 to 120
meq/L.
Hyponatremic encephalopathy may be
reversible, although permanent neurologic
damage or death can occur, particularly in
premenopausal women.
Overly rapid correction also may be
deleterious, especially in patients with
chronic asymptomatic hyponatremia.
خصوصیات بالینی :
عالیم عصبی :
بی عالمت
تهوع و بیحالی:سدیم کمتر از 125
سردرد – خواب آلودگی –گیجی :سدیم 120-115
ا ستوپور – تشنج – کما :سدیم کمتر از 115
-1هیپوناترمی بدون عالمت +کاهش حجم :
نرمال سالین
-2هیپوناترمی +ادم :
محدودیت سدیم و آب
تصحیح هیپوکالمی
دیورتیک لوپ +جایگزین کردن سدیم
-3پرنوشی اولیه – نارسایی کلیه و :SIADH
محدودیت آب
محاسبه کمبود سدیم
:ODS
فلج شل – دیزآرتری –دیسفازی
بیشتر در هیپوناترمی مزمن
مورتالیته باال
سایر عوامل خطر ساز :ODS
• آنوکسی
• هیپوکالمی
• سوتغذیه
Na deficit (mmol) = 0.6 x wt(kg) x (desired [Na] - actual [Na])
60 kg women, serum Na 107, seizure recalcitrant to benzodiazepines.
Na defecit = 0.6 x (60) x (120 – 107) = 468 mEq
Want to correct at rate 1.5 mEq/L/h: 13/1.5 = 8.7h
468 mEq / 8.7h = 54 mEq/h
3% NaCl has 513 mEq/L of Na
54 mEq/h = x
513 mEq
1L
x = rate of 3% NaCl = 105 cc/h over 8.7h to correct serum Na to 120 mEq/h
Note: Calculations are always at best estimates, and anyone getting
hyponatremia corrected by IV saline (0.9% or 3%) needs frequent
serum electrolyte monitoring (q1h if on 3% NS).
هیپرناترمی
تعریف :سدیم > 145
هیپرناترمی = هیپراسموالریتی
پاسخ مناسب به هیپرناترمی:
افزایش دریافت اب
دفع کمترین حجم ادرار
Causes of Hypernatremia
Hypernatremia is a relatively common problem
that can be produced either by the administration
of hypertonic sodium solutions or, in almost all
cases, by the loss of free water.
It should be emphasized that persistent
hypernatremia does not occur in normal subjects,
because the ensuing rise in plasma tonicity
stimulates both the release of ADH and, more
importantly, thirst.
The net effect is that hypernatremia primarily occurs
in those patients who cannot express thirst normally:
infants and adults with impaired mental status.
The latter most often occurs in the elderly , who also
appear to have diminished osmotic stimulation of
thirst.
Hospitalized persons, whether old or young, can
become hypernatremic iatrogenically as a result of
inadequate fluid prescription or impaired thirst.
Hypernatremia due to water loss is called
dehydration.
This is different from hypovolemia in
which both salt and water are lost.
UNREPLACED WATER LOSS
The loss of solute-free water will, if unreplaced,
lead to an elevation in the plasma sodium
concentration.
It is important to recognize that the plasma sodium
concentration and plasma tonicity are determined
by the ratio between total body solutes and the
total body water.
Thus, it is the sum of the sodium and potassium
concentrations that determines the effect that loss
of a given amount of fluid will have.
Patients with secretory diarrheas (cholera,
vipoma) have a sodium plus potassium
concentration in the diarrheal fluid that is
similar to that in the plasma.
Loss of this fluid will lead to volume and
potassium depletion, but will not directly
affect the plasma sodium concentration.
In contrast, many viral and bacterial
enteritides and the osmotic diarrhea induced
by lactulose (to treat hepatic encephalopathy)
or charcoal-sorbitol (to treat a drug
overdose).
Similar considerations apply to urinary
losses during an osmotic diuresis induced by
glucose, mannitol, or urea.
With these considerations in mind, the
sources of free water loss that can lead to
hypernatremia if intake is not increased
include:
Insensible and Sweat Losses
Insensible water loss from the skin and
respiratory tract by evaporation and sweat
are dilute fluids, the loss of which is
increased by fever, exercise, and
exposure to high temperatures.
Gastrointestinal losses
As mentioned above, some
gastrointestinal losses, particularly
osmotic diarrheas, will promote the
development of hypernatremia because
the sodium plus potassium concentration
is less than that in the plasma.
Central or Nephrogenic DiabetesInsipidus
Decreased release of ADH or renal resistance to
its effect cause the excretion of a relatively dilute
urine.
Most of these patients have a normal thirst
mechanism . As a result, they typically present
with polyuria and polydipsia.
However, marked and symptomatic
hypernatremia can occur if a central lesion
impairs both ADH release and thirst.
Osmotic Diuresis
An osmotic diuresis due to glucose, mannitol, or
urea causes an increase in urine output in which
the sodium plus potassium concentration is well
below that in the plasma because of the presence
of the nonreabsorbed organic solute.
Patients with diabetic ketoacidosis or nonketotic
hyperglycemia typically present with marked
hypertonicity, although the plasma Na
concentration may not be elevated due to
hyperglycemia-induced water movement out of
the cells.
Hypothalamic Lesions Affecting
Thirst or Osmoreceptor Function
Hypernatremia can also occur in the absence of
increased water losses if there is primary
hypothalamic disease impairing thirst (hypodipsia).
Two different mechanisms have been described,
which in adults, are most often due to tumors,
granulomatous diseases (eg, sarcoidosis), or
vascular disease.
SODIUM OVERLOAD
Acute and often marked hypernatremia (in
which the plasma sodium concentration can
exceed 175 to 200 meq/L) can also be
induced by the administration of hypertonic
sodium-containing solutions.
Examples include accidental or
nonaccidental salt poisoning in infants and
young children, the infusion of hypertonic
sodium bicarbonate to treat metabolic
acidosis, hypertonic saline irrigation of
hydatid cysts.
The hypernatremia in this setting will correct
spontaneously if renal function is normal, since
the excess sodium will be rapidly excreted in the
urine.
Too rapid correction should be avoided if the
patient is asymptomatic; these patients, however,
are less likely to develop cerebral edema during
correction, since the hypernatremia is generally
very acute with little time for cerebral adaptation.
علل هیپرناترمی:
دریافت اولیه سدیم
دفع اب:
خارج کلیوی:
• پوست :تعریق – تب -سوختگی
• تنفس :تهویه مکانیکی
کلیوی:
• دیورز اسموتیک
• دیورز دارویی
• DI
Even with optimal therapy, the mortality rate is
extremely high in adults with a plasma sodium
concentration that has acutely risen to above
180 meq/L.
For reasons that are not well understood,
severe hypernatremia is often better tolerated
in young children.
Diagnosis of Hypernatremia
Hypernatremia represents a relative deficit of
water in relation to solute.
Although it can be induced by the administration
of Na in excess of water (as with hypertonic
sodium bicarbonate during a cardiac arrest), a
high plasma Na concentration most often results
from free water loss.
DIAGNOSIS
The cause of the hypernatremia is usually evident
from the history.
If, however, the etiology is unclear, the correct
diagnosis can usually be established by
evaluation of the integrity of ADH-renal axis via
measurement of the urine osmolality.
A rise in the plasma sodium concentration is a
potent stimulus to ADH release as well as to
thirst; furthermore, a plasma osmolality above 295
mosmol/kg (which represents a plasma sodium
concentration above 145 to 147 meq/L) generally
leads to sufficient ADH secretion to maximally
stimulate urinary concentration.
Thus, if both hypothalamic and renal function are
intact, the urine osmolality in the presence of
hypernatremia will be above 700 to 800 mosmol/kg.
In this setting:
– unreplaced insensible or
– gastrointestinal losses,
– sodium overload, or
– rarely a primary defect in thirst
is likely to be responsible for the hypernatremia.
Measurement of the urine sodium
concentration may help to distinguish
between these disorders.
it should be less than 25 meq/L when water
loss and volume depletion are the primary
problems, but is typically well above 100
meq/L following the ingestion or infusion or a
hypertonic sodium solution.
The urine osmolality is lower than that of the
plasma, then either central (ADH-deficient) or
nephrogenic (ADH-resistant) diabetes insipidus is
present.
These conditions can be distinguished simply by
administering exogenous ADH.
The urine osmolality will rise, usually by 50 percent
or more, in central DI but will have little or no effect
in nephrogenic DI.
The history is also often helpful in this setting,
since severe nephrogenic DI in adults is uncommon
in the absence of chronic lithium use or
hypercalcemia.
حجم ECF
افزایش نیافته
ادرار کم حجم – غلیظ
افزایش یافته
تجویز NACLیا
NAHCO3
نه
بله
دفع خارج کلیوی اسموالریته ادرار> 750
بله
دیورز اسموتیک
عدم تغییر اسموالریته
NDI
نه
پاسخ به DDAVP
افزایش اسموالریته
CDI
درمان:
تجویز اب
دسموپرسین
غذای کم نمک
دوز کم تیازید
کلرپروپامید
کلوفیبرات
کاربامازپین
NSAIDs
Treatment of DI
AVP, Aqueous vasopressin (Pitressin)
Only parenteral form, 5-10 U SC q2-4h
Lasts 2-6h
Can cause HTN, coronary vasospasm
Chlorpropamide
(OHA which stimulates AVP secretion)
100-500 mg po OD-bid
Only useful for partial DI, can cause hypoglycemia
HTCZ
(induces volume contraction which diminishes free water
excretion)
50-100 mg OD-bid
Mainstay of Rx for chronic NDI
Amiloride
(blunts Lithium uptake in distal tubules & collecting ducts)
5-20 mg po OD-bid
Drug of choice for Lithium induced DI
Indomethacin 100-150 mg po bid-tid (PGs antagonize AVP
action)
Clofibrate 500 mg po qid (augments AVP release in partial CDI)
Clinical Manifestations of
Hypernatremia
The rise in the plasma sodium concentration and
osmolality causes acute water movement out of
the brain; this decrease in brain volume can
cause rupture of the cerebral veins, leading to
focal intracerebral and subarachnoid
hemorrhages and possible irreversible
neurologic damage.
The clinical manifestations of this disorder
begin with lethargy, weakness, and
irritability, and can progress to twitching,
seizures, and coma.
Values above 180 meq/L are associated
with a high mortality rate, particularly in
adults.
Correction of chronic hypernatremia must occur
slowly to prevent rapid fluid movement into the
brain and cerebral edema, changes that can lead
to seizures and coma.
Although the brain cells can rapidly lose potassium
and sodium in response to this cell swelling, the
loss of accumulated osmolytes occurs more slowly,
a phenomenon that acts to hold water within the
cells.
The delayed clearance of osmolytes from
the cell can predispose to cerebral edema if
the plasma sodium concentration is lowered
too rapidly.
As a result, the rate of correction in
asymptomatic patients should not exceed 12
meq/L per day, which represents an average
of 0.5 meq/L per hour.
free-water deficit=
0.4(0.5) x w x{ (Na p – 140) ÷ 140}
50-kg woman with a plasma Na+ concentration
of 160 mmol/L has an estimated free-water
deficit of 2.9 L {[(160 – 140) ÷ 140] x (0.4 x 50)}
160-140= 20
20 x 0.5 = 40 h
2900 ÷ 40= 73
پتاسیم
:تعادل پتاسیم
غلظت پالسمایی 3/5 :تا 5
غلظت داخل سلولی 150:
پمپ Na-K-ATPase
دریافت پتاسیم40:تا 120میلی مول در روز
دفع روده ای پتاسیم10:تا%60-50
دفع کلیوی پتاسیم:
%90توسط لوله پروگزیمال و هنله بازجذب می شود.
تنظیم ترشح در لوله دیستال و CCDدر principal cellاست
تحت کنترل :الدسترون و پتاسیم و میزان جریان دیستال
اثرات الدسترون :افزایش جذب سدیم
تحریک پمپ Na –K-ATPase
افزایش کانالهای پتاسیم لومینال
هیپوکالمی
Causes of Hypokalemia
Hypokalemia is a common clinical problem.
Potassium enters the body largely stored in the
cells, and then excreted in the urine.
Decreased intake, increased translocation into
the cells, or, most often, increased losses in the
urine (or gastrointestinal tract or sweat) all can
lead to potassium depletion.
کاهش دریافت :روزه داری
خاک خوری
DECREASED POTASSIUM
INTAKE
The normal range of potassium intake is 40 to
120 meq per day, most of which is then excreted
in the urine.
The kidney is able to lower potassium excretion
to a minimum of 5 to 25 meq per day in the
presence of potassium depletion.
INCREASED ENTRY INTO
CELLS
The normal distribution of potassium between the
cells (which contains approximately 98 percent
of exchangeable potassium) and the extra cellular
fluid is maintained by the Na-K-ATPase pump in
the cell membrane.
In some cases, however, there is increased
potassium entry into cells, resulting in transient
hypokalemia.
Elevation in Extracellular pH
Either metabolic or respiratory alkalosis can
promote potassium entry into cells.
Hydrogen ions leave the cells to minimize the
change in extracellular pH; the necessity to
maintain electro neutrality then requires the entry
of some K (and Na) into the cells.
This direct effect is relatively small, as the
plasma potassium concentration falls less then 0.4
meq/L for every 0.1-unit rise in pH .
Increased Availability of Insulin
Insulin promotes the entry of K into skeletal
muscle and hepatic cells, apparently by
increasing the activity of the Na-K-ATPase
pump.
The plasma potassium concentration can also
be reduced by a carbohydrate load.
Elevated Adrenergic Activity
Catecholamines, acting via the B-adrenergic
receptors , can promote potassium entry into
the cells, primarily by increasing Na-KATPase activity.
As a result, transient hypokalemia can be
caused in any setting in which there is stressinduced release of epinephrine, as with acute
illness, coronary ischemia, or theophylline
intoxication.
lower Gastrointestinal Losses
Hypokalemia is most common when the
losses occur over a prolonged period as
with a villous adenoma or a vasoactive
intestinal peptide secreting tumor
(VIPoma).
INCREASED URINARY LOSSES
Urinary potassium excretion is mostly derived
from potassium secretion in the distal nephron,
particularly by the principal cells in the cortical
collecting tubule.
This process is primarily influenced by two
factors: aldosterone and the distal delivery of
sodium and water.
Thus, urinary potassium wasting generally
requires increases in either aldosterone or distal
flow, while the other parameter is at least normal
or increased.
Diuretics
Any diuretic that acts proximal to the potassium
secretory site – acetazolamide, loop diuretics,
and thiazide-type diuretics – will both increase
distal delivery and, via the induction of volume
depletion, activate the renin-angiotensinaldosterone system.
As a result, urinary potassium excretion will
increase, leading to hypokalemia if these losses
are greater than intake.
Primary Mineralocorticoid Excess
Urinary potassium wasting is also
characteristic of any condition associated with
primary hypersecretion of a mineralocorticoid,
as with an aldosterone-producing adrenal
adenoma.
These patients are almost always hypertensive.
Loss of Gastric Secretions
This problem is usually suggested from the
history.
If, however, the history is not helpful, the
differential diagnosis of a normotensive patient
with hypokalemia, urinary potassium wasting,
and metabolic alkalosis includes: surreptitious
vomiting or diuretic use and Bartter's.
Hypokalemic Periodic Paralysis
Is a rare disorder of uncertain cause characterized
by potentially fatal episodes of muscle weakness
or paralysis which can affect the respiratory
muscles .
Acute attacks, in which the sudden movement of
potassium into the cells can lower the plasma
potassium concentration to as low as 1.5 to 2.5
meq/L.
Hypokalemic Periodic Paralysis
The recurrent attacks with normal plasma
potassium levels between attacks distinguish
periodic paralysis.
Hypokalemic periodic paralysis are often
precipitated by rest after exercise, stress, or a
carbohydrate meal, events that are often
associated with increased release of epinephrine
or insulin.
Hypokalemic Periodic Paralysis
The hypokalemia is often accompanied by
hypophosphatemia and hypomagnesemia.
May be familial with autosomal dominant
inheritance (in which the penetrance may be
only partial) or may be acquired in patients
with thyrotoxicosis.
The oral administration of 60 to 120 meq of
potassium chloride usually aborts acute attacks
of hypokalemic periodic paralysis within 15 to
20 minutes.
Another 60 meq can be given if no
improvement is noted.
However, the presence of hypokalemia must
be confirmed prior to therapy, since potassium
can worsen episodes due to the normokalemic
or hyperkalemic forms of periodic paralysis.
Prevention of hypokalemic episodes consists of
the restoration of euthyroidism in thyrotoxic
patients and the administration of a B blocker in
either familial or thyrotoxic periodic paralysis.
B blockers can minimize the number and
severity of attacks.
A nonselective B blocker (such as propranolol)
should be given; B1-selective agents are less
likely to inhibit the B2 receptor-mediated
hypokalemic effect of epinephrine.
Other modalities that may be effective for
prevention include:
K+ supplementation,
K+-sparing diuretics,
a low-carbohydrate diet,
and the carbonic anhydrase inhibitor.
(Acetazolamide)
Marked Increase in Blood Cell
Production
An acute increase in hematopoietic cell production
is associated with potassium uptake by the new
cells and possible hypokalemia.
This most often occurs after the administration of
vitamin B12 or folic acid to treat a megaloblastic
anemia or of granulocyte-macrophage colony-
stimulating factor (GM-CSF) to treat neutropenia .
Metabolically active cells can also take up
potassium after blood has been drawn. This has
been described in patients with acute myeloid
leukemia.
In this setting, the measured plasma potassium
concentration may be below 1 meq/L (without
symptoms) if the blood is allowed to stand at room
temperature.
This can be prevented by rapid separation of the
plasma from the cells or storage of the blood at 4°C
Hypothermia
Accidental or induced hypothermia can
drive potassium into the cells and lower
the plasma potassium concentration to
below 3.0 to 3.5 meq/L.
Hypomagnesemia
Hypomagnesemia is present in up to 40 percent of
patients with hypokalemia.
In many cases, as with diuretic therapy, vomiting,
or diarrhea, there are concurrent potassium and
magnesium losses.
In addition, hypomagnesemia of any cause can
lead to increased urinary potassium losses via an
uncertain mechanism.
Hypomagnesemia
Documenting the presence of hypomagnesemia
is particularly important because the
hypokalemia often cannot be corrected until the
magnesium deficit is repaired.
The concurrent presence of hypocalcemia (due
both to decreased release of parathyroid
hormone and resistance to its calcemic effect) is
often a clue to underlying magnesium depletion.
Polyuria
Normal subjects can, in the presence of the
potassium depletion, lower the urine potassium
concentration to a minimum of 5 to 10 meq/L.
If, however, the urine output is over 5 to 10
L/day, then obligatory potassium losses can
exceed 50 to 100 meq per day.
This problem is most likely to occur in primary
(often psychogenic) polydipsia.
خصوصیات بالینی:-1خستگی پذیری – درد ماهیچه ای – ضعف عضالت اندام تحتانی -ضعف عضالت
تنفسی
-2فلج کامل
-3رابدومیولیز
-4ایلئوس
-5تغییرات :EKG
صاف شدن یا معکوس شدن موج T
موج U
افت قطعه ST
طوالنی شدن QU
طوالنی شدن فاصله PR
پهن شدن QRS
-6افزایش خطر اریتمی بطنی
-7افزایش مسمومیت با دیگوکسین
-8الکالوز متابولیک
DI-9
GTT-10مختل
Diagnosis of Hypokalemia
Hypokalemia is a common clinical problem, the
cause of which can usually be determined from
the history (as with diuretic use, vomiting, or
diarrhea).
Measurement of the blood pressure and urinary
potassium excretion and assessment of acid-base
balance are often helpful.
URINARY RESPONSE
A normal subject can, in the presence of
potassium depletion, lower urinary potassium
excretion below 25 to 30 meq per day.
Random measurement of the urine potassium
concentration can also be used, but may be less
accurate than a 24-hour collection.
It is likely that extrarenal losses are present if the
urine potassium concentration is less than 15
meq/L (unless the patient is markedly polyuric).
Higher values, however, do not necessarily
indicated potassium wasting if the urine volume is
reduced.
DIAGNOSIS
Metabolic acidosis with a low rate of potassium
excretion is, in an asymptomatic patient,
suggestive of lower gastrointestinal losses due to
laxative abuse or a villous adenoma
Metabolic acidosis with potassium wasting is
most often due to diabetic ketoacidosis or to type
1 (distal) or type 2 (proximal) renal tubular
acidosis.
Metabolic alkalosis with a low rate of
potassium excretion is due to surreptitious
vomiting (often in bulimia in an attempt to lose
weight) or diuretic use (in which the urinary
collection is obtained after the diuretic effect
has worn off).
Metabolic alkalosis with potassium wasting and
a normal blood pressure is most often due to
surreptitious vomiting or diuretic use or to
Bartter's syndrome.
In this setting, measurement of the urine
chloride concentration is often helpful, being
low in vomiting.
Metabolic alkalosis with potassium wasting and
hypertension is suggestive of :
– surreptitious diuretic therapy in a patient with
underlying hypertension,
– renovascular disease,
– or one of the causes of primary
mineralocorticoid excess.
درمان:
اصالح کمبود پتاسیم
کلرید پتاسیم
سیترات پتاسیم
هیپرکالمی
تعریف :پتاسیم>5
پسودوهیپرکالمی
علل:
-1نارسایی کلیه
-2کاهش جریان دیستال
-3کاهش ترشح پتاسیم
الف-اختالل در بازجذب سدیم
هیپوالدوسترونیسم اولیه :نارسایی ادرنال – کمبود انزیمهای
ادرنال
هیپوالدرونیسم ثانویه :هیپورنینمی -داروها
مقاومت به الدرونیسم :هیپوالدرونیسم کاذب – بیماری توبولو
اینتراستیشیال –داروها
-4افزایش بازجذب یون کلر
سندرم گوردون
سیکلوسپورین
Causes of Hyperkalemia
The plasma potassium concentration is
determined by the relationship between
potassium intake, the distribution of potassium
between the cells and the extracellular fluid, and
urinary potassium excretion.
In normal subjects, dietary potassium is largely
excreted in the urine.
The degree of potassium secretion is primarily
stimulated by three factors:
– an increase in the plasma potassium
concentration;
– a rise in the plasma aldosterone concentration;
– enhanced delivery of sodium and water to the
distal secretory site.
Ingestion of a K load leads initially to the
uptake of most of the excess K by the cells, a
process that is facilitated by insulin and the B2adrenergic receptors, both of which increase the
activity of the Na-K-ATPase pump in the cell
membrane.
This is then followed by the excretion of the
excess K in the urine within six to eight hours .
POTASSIUM ADAPTATION
Hyperkalemia is a rare occurrence in normal
subjects, because the cellular and urinary
adaptations prevent significant potassium
accumulation in the extracellular fluid.
This phenomenon, called potassium adaptation,
is mostly due to more rapid potassium excretion
in the urine.
INCREASED POTASSIUM RELEASE
FROM CELLS
Pseudohyperkalemia
Refers to those conditions in which the
elevation in the measured plasma potassium
concentration is due to potassium movement
out of the cells during of after the blood
specimen has been drawn.
Pseudohyperkalemia
The major cause of this problem is mechanical
trauma during venipuncture, resulting in the
release of potassium from red cells .
It can also occur in hereditary spherocytosis and in
familial pseudohyperkalemia in which there is
increased temperature-dependent leakage of
potassium out of red blood cells after the specimen
is collected.
Pseudohyperkalemia
Potassium also moves out of white cells and
platelets after clotting has occurred.
Thus, the serum potassium concentration
normally exceeds the true value in the plasma
by 0.1 to as much as 0.5 meq/L.
Although this difference in normals is not
clinically important, the measured serum
potassium concentration may be as high as 9
meq/L in patients with marked leukocytosis or
thrombocytosis.
Metabolic Acidosis
The buffering of excess hydrogen ions in the
cells can lead to potassium movement into the
extracellular fluid; this transcellular shift is
obligated in part by the need to maintain
electroneutrality.
Insulin deficiency, Hyperglycemia, and
Hyperosmolality
The combination of insulin deficiency and the
hyperosmolality induced by hyperglycemia
frequently leads to hyperkalemia in uncontrolled
diabetes mellitus, even though the patient may be
markedly potassium depleted due primarily to
potassium losses in the urine.
An elevation in plasma osmolality results in
osmotic water movement from the cells into the
extracellular fluid. This is accompanied by
potassium movement out of the cells.
Increased Tissue Catabolism
Any cause of increase tissue breakdown result
in the release of potassium into the extracellular
fluid.
Clinical examples include trauma, the
administration of cytotoxic or radiation therapy
to patients with lymphoma or leukemia.
Beta-adrenergic Blockade
Nonselective B-adrenergic blockers interfere with
the B2-adrenergic facilitation of K uptake by the
cells.
This effect is associated with only a minor
elevation in the plasma potassium concentration in
normal subjects (less than 0.5 meq/L), since the
excess potassium can be easily excreted in the
urine.
Exercise
K is normally released from muscle cells during
exercise. This response may be mediated by two
factors:
A delay between potassium exit during
depolarization and subsequent reuptake by the
Na-K-ATPase pump.
With severe exercise, an increased number of
open K channels in the cell membrane. These
channels are inhibited by ATP, an effect that is
removed by the exercise-induced decline in
ATP levels which.
The release of potassium during exercise may
have a physiologically important role.
The local increase in the plasma potassium
concentration has a vasodilator effect, thereby
increasing blood flow and energy delivery to the
exercising muscle.
The degree of elevation in the systemic plasma
potassium concentration is less pronounced
and is related to the degree of exercise:
0.3 to 0.4 meq/L with slow walking;
0.7 to 1.2 meq/L with moderate exertion
(including prolonged aerobic exercise
with marathon running);
and as much as 2 meq/L following
exercise to exhaustion.
The rise in the plasma K concentration is reversed
after several minutes of rest, and is typically
associated with a mild rebound hypokalemia
(averaging 0.4 to 0.5 meq/L below the baseline
level) that may be arrhythmogenic in susceptible
subjects.
The degree of K release is attenuated by prior
physical conditioning , but may be exacerbated
by the administration of nonselective B-blockers
and, for uncertain reasons, in patients with CHF.
REDUCED URINARY
POTASSIUM EXCRETION
Impaired urinary potassium excretion
generally requires an abnormality in one or
both of the two major factors required for
adequate renal potassium handling:
aldosterone and
distal sodium and water delivery.
Hypoaldosteronism
Any cause of decreased aldosterone release or
effect, such as that induced by hyporeninemic
hypoaldosteronism or certain drugs, can diminish
the efficiency of K secretion.
Rise in the plasma K concentration directly
stimulates K secretion, partially overcoming the
relative absence of aldosterone.
The net effect is that the rise in the plasma K
concentration is generally small in patients with
normal renal function.
Renal Failure
The ability to maintain K excretion at near
normal levels is generally maintained in patients
with renal disease as long as both aldosterone
secretion and distal flow are maintained.
Hyperkalemia generally develops in the patient
who is oliguric or who has an additional
problem such as a high K diet, increased tissue
breakdown, hypoaldosteronism, or fasting in
dialysis patients (which may both lower insulin
levels and cause resistance to B-adrenergic ).
Effective Circulating Volume
Depletion
Decreased distal flow due to marked effective
volume depletion (as in heart failure, cirrhosis,
or a salt-wasting nephropathy) can also lead to
hyperkalemia.
Transtubular Potassium
Concentration Gradient
The differential diagnosis of persistent
hyperkalemia consists of those disorders in
which urinary potassium excretion is impaired.
The three most common causes of this
problem are advanced renal failure, marked
effective volume depletion (as with severe
heart failure), and one of the causes of
hypoaldosteronism.
TTKG is dependent upon two assumptions:
1: that the urine osmolality at the end of the
cortical collecting tubule is similar to that of the
plasma, since equilibration with the isosmotic
interstitium will occur in the presence of
antidiuretic hormone;
2: little or no potassium secretion or
reabsorption takes place in the medullary
collecting tubule.
Thus, the TTKG between the tubular fluid
at the end of the cortical collecting tubule
and the plasma can be estimated from:
TTKG = [Urine K ÷ (Urine osmolality
/ Plasma osmolality)] ÷ Plasma K
The TTKG in normal subjects on a regular
diet is 8 to 9, and rises to above 11 with a
potassium load, indicating increased
potassium secretion .
Thus, a value below 7 and particularly
below 5 in a hyperkalemic patient is highly
suggestive of hypoaldosteronism .
for example, the urine potassium
concentration is 30 meq/L, the plasma
potassium concentration is 6.5 meq/L, and
the urine and plasma osmolality are 560
mosmol/kg and 280 mosmol/kg,
respectively, then:
TTKG =
[30 ÷ (560/280)] ÷ 6.5
= 2.3
:خصوصیات بالینی
ضعف عضالنی – فلج شل – کاهش تهویه –
اسیدوز متابولیک
تغییرات EKG
T Tall
افزایش فاصله PRو مدت QRS
تاخیر هدایت دهلیزی بطنی – از بین رفتن موج P
پهن شدن موج QRSوادغام با موج ( Tطرح موج
سینوسی )
فیبریالسیون یا اسیستول بطنی
:درمان
گلوکونات کلسیم
انسولین +دکستروز
بیکربنات سدیم
Bاگونیست
سولفونات پلی استیرن سدیم
همودیالیز