Breast Ultrasound Portfolio PowerPoint
advertisement

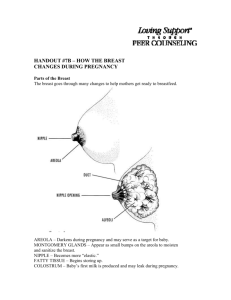
BREAST ULTRASOUND PORTFOLIO Calum Grimwood (17556082) Superficial Parts and Pediatric Sonography (MIRA5001) This PowerPoint aims illustrate my competency in examination technique, appropriate patient communication, management and duty of care as well as ability to identify and investigate pathology based on clinical and sonographic evidence. BREAST ULTRASOUND? INDICATIONS APPLICATIONS Development of new high-frequency Palpable +/- symptomatic breast linear transducers: or axilla lumps Mammographic abnormality Breast inflammation Breast ultrasound aids the assessment of abnormalities +/detected by mammography. Determine vascularity characteristics of lesions. Better characterize location, dimensions and characteristics of lesions > +/-biopsy. Candelaria et al. (2013) Nipple changes +/- discharge Augmented breast Follow-up Strong family history of Ca. Rumack et al. (2011) ANATOMY OF THE BREAST General Anatomy Ultrasound Anatomy Breast = modified sweat gland Between 2nd and 6th ribs 12-20 ducts exist and their lobules, along with fat and stroma – make up parenchyma/lobes of breast. 2) Skin Premammary layer = Subcutaneous fat of varied 3) Mammary layer = Glandular (functional) tissue 4) Retromammary layer = Contains deep fascia and 5) Muscle layer = Pectoralis major is posterior to 6) Chest wall 1) Ducts converge at nipple at one end and branch to terminate in lobules at other end. Rumack et al. (2011) Sonographically there are 6 layers of tissue identified. levels. containing epithelial and stromal tissue. Contain the TDLU’s, ducts, coopers ligaments. varied levels of fat , allows for breast motion over chest wall retromammary layer. Pec minor is posterior to Pec major Dense fibroglandular tissue Jesinger (2014) Fatty tissue > Age > Obesity + Pregnancy PATIENT COMMUNICATION – BEFORE, DURING AND AFTER BEFORE > …breast ultrasound can be a touchy subject Explain the procedure thoroughly I like to tell my patient that I will firstly be conducting a scout scan through the breast, taking pictures around the breast over the nipple and in the armpit region. I assure them that we will look at their ROI in depth after for further documentation. I also state that we show all of our cases to the doctor to ensure they are happy and that some Radiologists like to come in purely as a second pair of eyes so there is no need to be alarmed (I feel this puts their mind at rest). 2) Before starting, be sure to get consent – the patient must first say they are happy to proceed after the procedure is explained. DURING > During the scout scan I like to instigate the reason for the patients attendance. I then ensure I obtain an adequate history including previous breast surgery/conditions, any family history of breast cancer, and the use of any medication or hormone drugs. +++ time efficiency if you ask this during the scout scan. AFTER > Let the patient know that the doctor will be reviewing the images immediately and that they will be correlated with any previous mammogram/ultrasound. Any necessary follow up scans or biopsies should be explained. Follow up scans should be for keeping an eye on things as they should remain stable or in some cases remise. Biopsies allow us to better categorize lesions – IT DOES NOT HAVE TO BE Ca. Ensure the patient has fully understood what is being explained. I like to reaffirm what the Radiologist has told them and ask if they understand why we are doing something and what we are doing it for. Inform patient as to results delivery/collection protocol. 1) *Breast ultrasound can be stressful for patients – I believe that adequate communication is everything and if they understand the exact reasons for why we do something they are more calm - they are informed. Answer any questions or concerns they have. APPROPRIATE SCANNING TECHNIQUE Get female breast ultrasound patients changed into a easy to remove gown. Male patients are generally happy to remove their shirt Ensure the room is warm and preferably warm gel is used for both patient comfort and nipple evaluation. Position the patient supine with the ipsilateral arm raised above their head so that the breast tissue is generally flat/even/symmetrical… this may require using multiple positions and the use of a wedge sponge. Use a high frequency >7MHz linear transducer. Conduct a scout scan of the entire breast including the axilla region and over the nipple, ensuring all breast anatomy is visualized with adequate depth to the chest wall. Take appropriate workplace protocol images – this generally involves 12 breast images (each o’clock), 2 images over the nipple (long and trans), 2 images in the axillary region (long oblique and trans). *It is important to vary the amount of probe pressure when scanning the breast. Minimal/no pressure should be used when identifying cystic lesions and vascularity in lesions as small blood vessels can be easily compressed. Similarly more pressure should be applied when attempting to adequately flatten breast tissue or when attempting to overcome artefacts such as those caused by coopers ligaments. APPROPRIATE SCANNING TECHNIQUE If the patient has felt a lump or area of pain > annotate as ROI (region of interest). Proceed to take specific images 90 degrees to each other, even if no obvious lump is seen. I find that additional images confirm to the Radiologist that you have thoroughly looked over the area and are confident that no concerning pathology is seen on ultrasound. In addition to this, spending extra time over the region of interest reassures the patient that you have taken their concerns seriously. Additional views of pathology Measurements Optimize w/ zoom, gain and focal zone. Color/power doppler on both solid and cystic lesions I personally like to use twin view when documenting my breast pathology in two planes. This allows a dual screen both in real time allowing one image to adequately illustrate pathology clearly and use calipers to measure size, and the second image demonstrates the vascularity of lesion using either color/power doppler. I like to use both power and color doppler to exclude low flow. Distance from nipple for suspicious or solid lesions I like to use body markers and calipers on the screen to demonstrate plane of image and accurate distace from nipple. +/- Vocal fremitus I was taught to use vocal fremitus to help try and distinguish between cysts and solids. Use a stand off pad for superficial pathologies. WORKPLACE PROTOCOL 1) SCOUT SCAN Adequate scout scan of the breast (AT LEAST 2 PLANES) For my scout scan I firstly scan the breast longitudinally starting from the sternum and moving laterally to the axilla, moving the probe down slowly once at the axilla and then scanning back laterally to medially so the transducer always has contact with the patient and adequate overlapping can occur during the scout. This is Followed by scanning transverse from superior to inferior. 2) IMAGE SERIES i) Breast = Utilising the clock method, at least 12 images of the breast parenchyma at each “hour” of a clock illustrating all breast ultrasound anatomy. I orientate the probe so that the nipple is always to the Rt of the screen. Between each of 12, 3, 6 and 9 o’clock positions I sweep back over the breast so that you are essentially conducting a scout scan in 3 planes in total. ii) Nipple = Long at Trans of nipple. Iii) Axilla = Long oblique and/or trans. However, I prefer to take numerous axilla images illustrating each level of anatomy in at least 2 planes. *Note further images are necessary to document breast/nipple pathology and lymph nodes NECESSARY IMAGES Following an adequate scout scan in at least 2 planes. Images 1-4 illustrate normal female breast images from 12-3o’clock in the Rt breast. NECESSARY IMAGES Images 5-8 illustrate normal female breast images from 4- 7o’clock in the Rt breast. NECESSARY IMAGES Images 9-12 illustrate normal female breast images from 8-11o’clock in the Rt breast. NECESSARY IMAGES Images 13-16 demonstrate longitudinal and transverse nipple images and axillary images depicting lymph node AP measurements. PATHOLOGY DOCUMENTATION Example of pathology documentation. The solid hypoechoic lesion (proven to be a fibroadenoma following a core biopsy) is documented in 2 planes 90 degrees to eachother with calipers and a body marker showing orientation, color doppler with minimal/no probe pressure and caliper measurements to obtain accurate distance from the nipple. IMPLANTS Silicone Prosthesis used to change the size, form, and/or texture of the breast. Treat the scan as a 2-fold examination 1) Breast tissue protocol. 2) Deeper implant to check integrity – this may require lower frequency or a curved probe to investigate. Saline Shell filled with viscous gel. Sterile salt water. Pre-filled or filled w/ valve Leaking wont collapse implant. Molded contours/shapes. Extracapsular silicone can spread to LN’s. ?anaplastic cell lymphoma Absorbs by patient body if leaks. Smaller incisional line. More prone to rupture. Feel less natural For imaging of implants I like to complete my normal breast protocol first then move onto the implants lastly. I firstly conduct a scout scan around the whole peripheral border of the implant taking images at 12, 3, 6 and 9 o’clock if in tact. I also check the integrity of the implant at its deepest in the middle of the breast ensuring adequate depth to the posterior chest wall, taking two images in two planes. Additional images are taken to document any rupture or implant abnormality. Ask the patient important questions such as: How long have they had the implants? Any prior imaging? Are they silicone, saline, ‘gummy bear’ or double lumen? Are the implants submuscular, subglandular, subfascial or dual plane? Is the patient experiencing any problems related to the implant? Common implant ultrasound indications include rupture (intracapsular – look for linguini sign, or extracapsular), implant herniation, or capsular contracture. Stachs et al. (2015) PATHOLOGY Breast ultrasound of pathology: Reasonable sensitivity but poor specifity Allows the differentiation of solid and cystic lesions Complements clinical examination and mammo Biopsy suspicious lesions Clinically palpable lumps either by the doctor or patient should be palpated by the sonographer after gaining patient permission… It may provide some insight Single smooth mobile palpable lump - ?cyst, ?benign finding, ?other Single tough non mobile palpable lump - ?Breast Ca, ?other General area of lumpiness - ?dense fibroglandular ridge, ?polycystic breasts, ?other. Correlate patient complaints, clinical history, and clinical presentation with sonographic appearance. Bosch et al. (2014). PATHOLOGY Benign vs.. malignant ultrasound appearance. Benign Malignant Shape Oval/ellipsoid Variable Alignment Wider than tall; aligned parallel to tissue planes Taller than wide Margins Smooth/thin Echogenic capsule with 2-3 gentle lobulations Irregular or spiculated border; echogenic ‘halo’ Echotexture Variable to intense hyperechogenicity Low-level, marked hypoechogenicity. Homogeneity of internal echoes Uniform Non-uniform Lateral shadowing Present Absent Posterior effect Minimum attenuation/posterior enhancement Attenuation with obscured posterior margin Other signs --- Calcification, microlobulation, intraductal extension, infiltration across tissue planes. Rumack et al. (2011) REFERENCES Bosch AM, Kessels AG, Beets GL. 2014. ”Interexamination variation of whole breast ultrasound”. Br J Radiol. 76(905): 328-331 Candelaria, Rosalind P., Lindsay Hwang, Richard R. Bouchard, and Gary J. Whitman. 2013. "Breast ultrasound: current concepts." In Seminars in Ultrasound, CT and MRI. 34(3): 213-225. Jesinger, Robert A. 2014. "Breast anatomy for the interventionalist." Techniques in vascular and interventional radiology.17(1): 3-9. Rumack, Carol M., Stephanie R. Wilson, William Charboneau and Deborah Levine. 2011. Diagnostic Ultrasound. 4th ed: Elsevier Mosby. Stachs, Angrit, Max Dieterich, Steffi Hartmann, Johannes Stubert, Toralf Reimer, and Bernd Gerber. 2015. "Diagnosis of Ruptured Breast Implants Through High-Resolution Ultrasound Combined With Real-Time Elastography." Aesthetic Surgery Journal. 35(4): 410-418.