Fluoroscopy Safety
advertisement

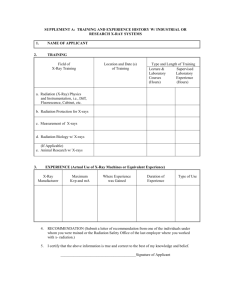
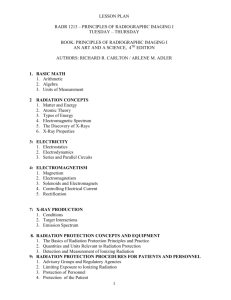
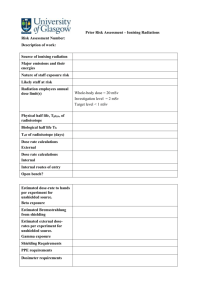
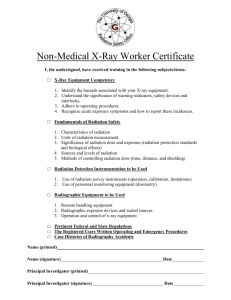
Fluoroscopy Safety Robert Metzger, Ph.D. Introduction On September 9th, 1994, the FDA issued an advisory for facilities that use fluoroscopy for invasive procedures. Recommendations…. Appropriate credentials and training for physicians performing fluoroscopy Operators be trained and understand system operation, and implications of radiation exposure for each mode of operation Physicians be educated in assessing risks and benefits on a case-by-case basis for patients Patients be counseled regarding the symptoms and risks of large radiation exposures Physicians justify and limit use of high dose rate modes of operation Who Can Perform Fluoroscopy and Associated Radiography? Most states have regulations regarding the operation of radiation producing equipment and these regulations vary from state to state. However, the fact is that many physicians who use fluoroscopy have essentially no training in this area. In some states, it may be illegal for an untrained person to operate an x-ray machine even under the direct orders of a physician. What should an operator know? How to operate the machine How to properly position the patient How to minimize the use of radiation How the radiation is distributed in the room How to control the factors that optimize image quality (kVp, mA etc.) How to control factors that reduce radiation levels (collimation) How to properly use shielding devices and personnel monitoring devices What an operator should know Two professionals trained in specific aspects of fluoroscopy are the radiological technologist and medical physicist Physician is ultimately responsible for assuring that the x-rays are safely and properly applied and that appropriate radiation protection measures are followed Nurses or physician assistants should be trained in its safe and proper operation if asked to operate x-ray equipment Skin Injuries During the application of x-rays, the patient has no sensation of temperature rise in the skin, even if the patient is fully conscious and even for all but the most massive doses of radiation Chronic exposure to low doses can also result in gradual erosion of tissue Small doses from modern equipment might induce cancer, but the frequency of induction would be too low to detect a direct relationship with x-rays Potential Effects in Skin in Fluoroscopy c.f. Wagner and Archer. Minimizing Risks from Fluoroscopic X-rays. 1996. Skin Injuries – Case Reports Three weeks post rf cardiac catheter ablation Ischemic dermal necrosis 5 months post procedure Exposed to 20 minutes fluoro with elbow 2025 cm from focal spot. Note circular pattern coinciding with x-ray beamport Suggesting that the 18 Gy threshold was passed during the procedure c.f. Koenig TR, et al. Skin Injuries from Fluoroscopically Guided Procedures: Part 1, Characteristics of Radiation Injury. AJR 2001, 177, pp. 3-11. Skin Injuries – Case Reports Skin Injuries – Case Reports Deep ulceration with exposure of the humerus at 6.5 months post-procedure Some radiation ulcers never heal completely, but break down intermittently. Progression of the ulcer may ensue and can be extensive, exposing deep tissues such as tendons, muscles or bones. c.f. Koenig TR, et al. Skin Injuries from Fluoroscopically Guided Procedures: Part 1, Characteristics of Radiation Injury. AJR 2001, 177, pp. 3-11. Skin Injuries – Case Reports Three transjugular intrahepatic portosystemic shunt placements within a week Non-healing deep tissue necrotic ulcer with exposure of deep tissues, including spinous processes of vertebra at 22 mos. Injuries that are advanced to this stage require surgical excision and grafting. At 23 months, musculocutaneous skin grafting was performed. Disfigurement is permanent. c.f. Koenig TR, et al. Skin Injuries from Fluoroscopically Guided Procedures: Part 1, Characteristics of Radiation Injury. AJR 2001, 177, pp. 3-11. Radiation Injuries of the Skin Many articles in literature about skin injuries (see Koenig manuscript) Some case reports teach us two important lessons: Radiation dermatitis is delayed, from weeks to years after the exposure Several procedures can result in very high cumulative doses to the same area if the skin A conscientious effort should be made to avoid prolonged exposure to the same area of the skin Documentation of certain conditions will help physicians if future procedures are needed A careful record identifying the location of the exposed skin will alert other physicians about the need to avoid irradiation of the same area A record of the estimated skin dose is also helpful Controlling Image Quality, Dose, and Dose Rate The following ten factors are the principal determinants of image quality, radiation dose rate and total radiation dose to the patient and to personnel during fluoroscopy → “the Ten Commandments” patient size tube current (mA) and kVp proximity of the x-ray tube to the patient proximity of the II to the patient image magnification x-ray field collimation and use of a grid shielding and position of personnel relative to patient and equipment beam-on time Commandment #1: Patient Size Keep in mind that dose rates are greater and dose accumulates quicker for larger patients Commandment #2: Tube Current (mA) Keep the tube current as low as possible Commandment #3: Tube Kilovoltage (kVp) Keep the kVp as high as possible to achieve the appropriate compromise between image quality and low patient dose Commandment #4: Proximity of x-ray tube to patient Keep the x-ray tube at the maximal “reasonable” distance from the patient Commandment #5: Proximity of the Image Intensifier to the Patient Keep the image intensifier as close to the patient as possible To optimize image quality and reduce radiation dose Optimize image quality distortion of anatomy and image blur decreases Radiation Dose decrease x-ray intensity required to produce a bright image (automatic brightness control) decreases Commandment #6: Image Magnification Don’t overuse the magnification mode of operation Magnification can be achieved in 2 ways: magnification option on the image intensifier geometric magnification (#6) Magnification Magnification options of the image intensifier This is achieved by making the x-ray field smaller and displaying the smaller field over the full viewing area of the monitor The mode of least magnification (largest field) usually delivers the lowest dose rate Sometimes the dose rate does not change with magnification but frequently, the dose rate increases with magnification To optimize overall radiation management, use the lowest level of magnification consistent with the goals of the procedure and reduce the irradiated volume of the patient by employing narrow collimation (#6) Magnification Geometric Magnification Achieved by increasing the distance between the patient and the image intensifier (contrary to dose reduction method) Geometric magnification can be used with isocentric systems Dose typically increases with the square of the magnification i.e., if magnification increases by 2x, dose rate goes up by 4x Maximum dose rates in this configuration may exceed 10 R/min (legal entrance exposure limit) this is because compliance dose rates are tested under conditions of least geometric magnification (patient closest to image intensifier) Again, the minimum magnification consistent with the goals of the procedure should be used to manage radiation properly Commandment #7: the Grid Remove the grid during procedures on small patients, thin body parts or when the image intensifier cannot be placed close to the patient Commandment #8: X-ray field Collimation Always use tight collimation Commandment #9: Distance Shielding Personnel must wear protective aprons, use shielding, monitor their doses, and know how to position themselves and the imaging equipment for minimum dose (#9) Shielding and Distance The principal source of radiation for the patient is the x-ray tube (#9) Shielding and Distance The principal source of radiation for the operator and other personnel is scatter from the patient (#9) Shielding and Distance One of the most important means by which personnel can reduce dose to themselves is by using shielding and properly positioning themselves relative to the patient and the fluoroscopic equipment All personnel who are not positioned behind a radiation barrier must wear a lead apron during a procedure (#9) Shielding and Distance Lead aprons lead equivalency: 0.25 mm to 0.50 mm 0.25 mm: absorbs > 90% of scatter 0.35 - 0.50 mm: absorbs 95 - 99% of scatter (but heavier) Lead aprons should be properly stored on a hanger when not in use Aprons should be checked annually for holes, cracks or other forms of deterioration x-ray (#9) Shielding and Distance Aprons do not protect the thyroid gland or the eyes. Thyroid shields and leaded glass can be used Leaded glass attenuates 30%-70% depending on the content of lead in glass Protective gloves of 0.5 mm lead of greater should be worn if hands are going to be near the primary beam (false sense of protection) Protection of a Physician’s Hands Dermal atrophy of the forearm and hands were observed in physician who performed fluoroscopy for years Convinced some physicians to wear special radiation-attenuating surgical gloves or hand shields Such devices are not likely to protect hands if placed fully into the beam The automatic brightness control (ABC) detect the reduction in brightness due to the attenuation by the gloves and boost the radiation output to penetrate the “protective” gear Protective hand gear can be relied on only to protect against radiation outside the field of view of the ABC Protection of Physician’s Hands To protect hands during fluoroscopy, it is recommended: Keep hands out of and away from the x-ray field when the beam is on unless physician control of invasive devices is requires for patient care during fluoroscopy Work on the exit-beam side of the patient whenever possible x-ray tube should be below table for vertical orientations for oblique and lateral projections, stand on the side of the patient where the image intensifier is located for adult abdomen, exit radiation is only about 1% the intensity of the entrance radiation extra care must be exercised in situations where physician must work on the x-ray tube side of the patient Protection of Physician’s Hands To protect hands during fluoroscopy, it is recommended to: wear a ring badge to measure your hand exposure monthly ring monitors dose only at the base of the finger dose at the finger tips may be significantly higher c.f. Wagner and Archer. Minimizing Risks from Fluoroscopic X-rays – Supplement 1. 1997. (#9) Shielding and Distance All personnel who perform fluoroscopic procedures are required to wear a radiation monitoring device, usually a film badge Personnel potentially exposed to 10% of the occupational annual limit (50 mGy or 5000 mrem) need a radiation badge It is recommended that personnel wear their badges anteriorly on their collar outside of lead apron Badge readings are monitored by the radiation safety office (RSO) (#9) Distance Radiation Dose to personnel can be significantly reduced by increasing their distance from the radiation source Inverse-square law: the dose rate drops significantly as the distance from the source increases Given: Exposure Rate at 2 ft = 90 mR/hr. (#9) Distance 3 ft 2 ft 1 ft 1 ft 2 ft 3 ft 2 ft 4 ft 6 ft D1 E2 E1 D2 2 Exposure Rate at 4 ft = (90 mR/hr)(2ft/4ft)2 = 22.5 mR/hr. Exposure Rate at 6 ft = (90 mR/hr)(2ft/6ft)2 = 10 mR/hr. (#9) Radiation at 1 Meter From Patient About 0.1% of patient entrance radiation exposure reaches 1 meter from patient 1m x-ray 100% 0.1% The NCRP recommends that personnel stand at least 2 meters from the x-ray tube, whenever possible. (6 feet = 1.82 m) (#9) C-Arm Fluoroscopy Shielding With the C-arm oriented vertically, the x-ray tube should be located beneath the patient with the II above In a lateral or oblique orientation, the x-ray tube should be positioned opposite the area where the operator and other personnel are working In other words, the operator and II should be located on the same side of the patient This orientation takes advantage of the patient as a protective shield (#9) The Separator Device (or Spacer Cone) The FDA requires that fluoroscopic x-ray machines be designed so that the patient’s skin is at least a specified fixed distance from the X-ray source The purpose of this regulation is to prevent the dangerous situation in which the intense beam emerging from the x-ray source is too close to the patient’s skin To provide flexibility for some procedures, the FDA permits machines to be designed with removable spacers For Dx procedures, the device is to remain attached to the x-ray source For modern machines fixed in room, this distance is 38 cm For mobile machines, this distance is 30 cm For “special surgical procedures” the device may be removed and the minimum distance can be as short as 20 cm (potentially dangerous) (#9) The Separator Device (or Spacer Cone) c.f. Wagner and Archer. Minimizing Risks from Fluoroscopic X-rays – Supplement 1. 1997. Commandment #10: Beam OnTime Keep beam-on time to an absolute minimum! - The Golden Rule Control over beam on-time is almost always the most important aspect of radiation management It is essential practice to disengage fluoroscopic exposure when the image on the monitor is not being used Absentmindedly leaving the x-rays on while viewing other factors associated with the procedure, such as direct observation of the patient or communication with other personnel in the room, must be strictly avoided Fluoroscopic Timer A 5-minute cumulative timer is required on all fluoroscopic units to remind the operator audibly of each 5-minute time interval and to allow the technologist to keep track of the total amount of fluoro time for the exam Good Vs. Bad Geometry: Patient Dose and the Position of the Fluoroscope the Good c.f. Wagner and Archer. Minimizing Risks from Fluoroscopic X-rays – Supplement 1. 1997. the Bad Good Vs. Bad Geometry: Patient Dose and the Position of the Fluoroscope the Ugly c.f. Wagner and Archer. Minimizing Risks from Fluoroscopic X-rays – Supplement 1. 1997. even Uglier Good Vs. Bad Geometry: Summary Differences in geometry of as little as a few centimeters can have a major impact on dose to a patient’s skin c.f. Wagner and Archer. Minimizing Risks from Fluoroscopic X-rays – Supplement 1. 1997. Good Vs. Bad Geometry: Patient Dose and Physician Height No invasive devices present c.f. Wagner and Archer. Minimizing Risks from Fluoroscopic X-rays – Supplement 1. 1997. Invasive devices present Good Vs. Bad Geometry: Patient Dose and Physician Height 30% dose reduction c.f. Wagner and Archer. Minimizing Risks from Fluoroscopic X-rays – Supplement 1. 1997. Good Vs. Bad Geometry: Patient Dose and Invasive Devices In many invasive procedures, syringes, catheters, or other devices may be protruding from the patient With the patient prone on the procedure table, some distance must be maintained between the patient and the image intensifier to provide adequate working space In oblique orientations it is necessary to move the image intensifier to a position that avoids collisions with the patient and the invasive devices This may place severe constraint on how far the x-ray tube can be positioned from the patient For larger patients, the port of the x-ray tube may actually come into contact with the patient’s skin Extreme caution is advised in these situations to reduce the potential of inducing skin burns Good Vs. Bad Geometry: Invasive Devices and Personnel vs. Patient Dose c.f. Wagner and Archer. Minimizing Risks from Fluoroscopic X-rays – Supplement 1. 1997. Good vs. Bad Geometry: Recommendations on Managing Risks from Geometry Attach the separator cone to the port if at all possible Move the x-ray tube away from the skin as far as practicable Move the image intensifier as close to the patient as possible Keep the beam-on time of the study as short as possible If the image contrast is not affected, remove the grid Routinely keep hands away from the imaged area and outside the housing of the image intensifier Use collimation to control image quality and reduce scatter Monitor hand dose Step back from the patient before engaging fluoroscopy Use a transparent shield for the head and neck if the x-ray tube is above the patient Have assistants use extra shielding or stand well back from the patient if tube is above patient Good vs. Bad Geometry: Where Do Stand When Using a C-Arm? When using lateral and oblique projections, the scatter radiation and the primary beam are least intense on the exit beam side (image intensifier side) of the patient For example, in the lateral orientation scatter is about 3 to 10x greater on the x-ray tube side than on the image intensifier side, depending on patient size and section of body irradiated In many situations, it is required that the physician work on the x-ray tube side For example, cardiologists work in a bi-plane configuration and stand next to the laterally projecting x-ray tube located on the right side of the patient, left side of cardiologist exposed lead aprons and ceiling suspended radiation shields should be used to reduce exposure to the head and neck radiation badge should be worn on the left side Cataracts Cataracts are a potential risk for patients undergoing high-dose interventional procedures in the head The threshold for radiation-induced cataract is about 1 Gy To reduce the potential for cataracts: for lateral orientation of the tube, the eyes can be shielded on the lateral side by using tight collimation to shield a large portion of the orbit that is closest to the x-ray tube the frontal view should be performed with the x-ray tube posterior to the head and the image intensifier anterior. This ensures that the eyes receive only the much reduced exit beam dose and not the much higher entrance dose http://www.optometry.co.uk/articles/20010406/brown.pdf Thoracic Fluoroscopy in Women Breast cancer has been induced in women who underwent thoracic fluoroscopic evaluation for the treatment of tuberculosis These women, for the most part, were positioned with their breasts facing the x-ray tube This might occur with today’s procedures if the xray c-arm is oriented for an oblique view through the thorax, perhaps to view the spine breast could get exposed to high x-ray intensities It may be reasonable to turn the c-arm over so that the x-ray tube is above the back of the prone patient breast would receive only the reduced exit dose Position the beam so that the breast is not in direct line with the x-rays or consider using tape or bandages to move some of the breast out of the direct x-ray beam http://www.xray.hmc.psu.edu/rci/ss1/ss1_4.html Dose Reduction by Heavy Filtration Some modern fluoroscopy units now provide options for heavy x-ray beam filtration under some conditions (e.g., Philips ‘Spectrabeam’) this filtration more effectively removes non-penetrating, doseenhancing, low-energy x-rays than does conventional filtration this results in reduced patient x-ray exposure this heavy filtration typically consists of thin plates of copper inserted at the window of the x-ray source To be effective, the tube current must be set very high The physician should be aware that the equipment has this special feature and know when it is engaged so that unnecessary concerns over high tube currents can be avoided Other Factors Use modes of operation such as pulsed fluoro (30, 15, 7.5 and 3.75 pulses per second) which reduce dose dramatically over continuous fluoro techniques Try to avoid long exposure time to same skin area Don’t allow any extraneous body parts in the beam Real-time dose monitoring is now standard on most newer fluoroscopic/angio/interventional systems Try to avoid high skin dose modes of operation such as cine, highlevel control if possible Conclusions Be smart about radiation and use common sense Keep the beam-on time to a minimum Consciously and conscientiously practice ALARA Apply the risk-reducing factors (“the Ten Commandments”) discussed herein for the patient’s safety as well as your own