Chapter Four
advertisement

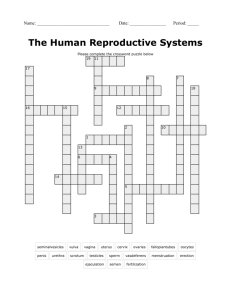
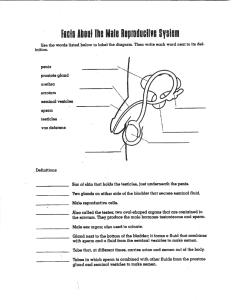
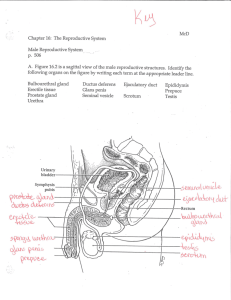
Chapter Four Male Sexual Anatomy and Physiology Agenda Discuss Male Sexual & Reproductive System Describe Male Maturation Cycle Discuss Male Reproductive and Sexual Health What do you think about the penis? On a blank sheet of paper, respond to the following: “The penis is…” Do not put your name on the paper, but turn it in. The Male Sexual and Reproductive System External Sex Organs Internal Sex Organs Other Sex Organs External Sex Organs Boys are typically more comfortable with their genitalia than girls Testes are visible (ovaries are internal) Penis is typically held during urination External sex organs Penis Scrotum The Penis Contains urethra for urine and semen transport Becomes erect to better penetrate the vagina and deposit sperm near the os No bone, little muscle Composed of 3 cylinders of erectile tissue Corpora cavernosa (2) Corpus spongiosum (contains the urethra) Internal structure of the penis (side view) The Glans Penis The conelike end of the penis Corona Frenulum Meatus Sensitive to stimulation The Glans Penis Foreskin is a fold of skin that can cover part or all of the glans; retracts over the corona during an erection Circumcision – surgical removal of the foreskin; most common male surgery in the U.S. Religious/cultural ritual Health reasons Medical value is questionable Women report greater sexual satisfaction with partner’s who have not been circumcised (O’Hara & O’Hara, 1999) Class Discussion Male Circumcision is the most common male surgical procedure in the U.S. but it doesn’t seem to be medically necessary. Why do you think it remains so common? Discuss the finding from O’Hara & Hara (1999) which reported that women experience greater sexual satisfaction with men who have not been circumcised. The Root of the Penis Extends into the body below the pubic bone Attached to internal pelvic muscles and can be felt in the perineum The male reproductive organs. Erection Any type of stimulation perceived as sexual can cause an erection; spinal reflex Erection also occurs during REM, possibly to keep the penis supplied with blood Nerve fibers open the arteries of the penis to allow blood to flow into the 3 cylinders Veins compress to prevent exit of blood Flaccid state returns when arteries constrict and the veins open to allow blood to flow out The Scrotum Loose, wrinkled pouch beneath the penis containing the testicles Lightly covered with pubic hair Functions to keep the testicles 3°C cooler than the body’s temperature to keep sperm viable Contains sweat glands Cremaster muscle moves the scrotum closer to or farther from the body (protects) Internal Sex Organs Testes Epididymis Vas deferens Seminal vesicles Prostate gland Cowper’s glands The male reproductive organs. The Testicles Two egg-shaped glands in the scrotum 2 inches long, 1 inch diameter Typically one (usually the left) hangs a bit lower to allow sliding past rather than compression 2 primary functions: Testosterone production Spermatogenesis (a/k/a sperm production) Testosterone Production Testosterone is the most important male hormone Interstitial, or Leydig, cells in the testicles produce testosterone out of cholesterol Spermatogenesis Seminiferous tubules produce and store sperm Sertoli cells (in the tubules) provide nutrition for the development of sperm Sperm production takes 72 days, but is constant and each male produces about 300 million sperm a day The Ejaculatory Pathway Ejaculation – physiological process where seminal fluid is powerfully expelled from the penis Pathway organs: Vas deferens Seminal vesicles Prostate gland Cowper’s glands The Ejaculatory Pathway Vas deferens – 18-inch tube that carries sperm from the testicles, combines fluids from other glands, and propels the sperm Seminal vesicles – next to the ampulla of the vas deferens; secretes a nutritional bath for traveling sperm; 60-70% of the ejaculate volume; joins the vas deferens to form the ejaculatory duct that passes into the prostate and then forms the urethra The Ejaculatory Pathway Prostate gland – walnut-sized gland beneath the bladder; secretes a fluid that neutralizes the acidity of the vagina that would be lethal to sperm; 25-30% of the ejaculate’s volume Cowper’s (bulbourethral) glands – 2 peasized glands next to the urethra, under the prostate; contributes fluid that cleans the urethra of lethal acidic urine; comprises the majority of the pre-ejaculatory fluid Ejaculation Once the threshold is reached: Epididymis, seminal vesicles, and prostate empty their fluids into the urethral bulb A sphincter closes off the bladder 5-15 contractions at the base of the penis squeeze the urethral bulb Ejaculate is expelled Orgasm Return to flaccid state Ejaculate/Semen 2-5 milliliters of fluid 50-150 million sperm per milliliter Few sperm reach the ovum Sperm work together in order to fertilize the egg Semen coagulates upon ejaculation; this helps it remain in the vagina and travel into the uterus 5-20 minutes later it thins out Other Sex Organs Breasts – mostly muscle and no functional purpose; some men are sexually pleased when the nipples are stimulated Erogenous zones – scrotum, testicles, anus Stimulation perceived as sexually exciting can determine what is erogenous to each person The Male Maturation Cycle Male Puberty Andropause Class Discussion Do you think most men are concerned with the size of their penis? Why or why not? Do you think there is a correlation between penis size and masculinity? If penis enlargement surgery was 100% effective, what percentage of men do you think would have the surgery? Male Puberty Around 10 years of age, the hypothalamus starts to release gonadotropin releasing hormone (GnRH) which signals the pituitary to release FSH and LH At the testes, LH stimulates testosterone production; the two combined and FSH stimulate sperm production (around 12 years) Negative feedback loop Male Puberty Many organs and glands increase in size: testicles, penis, epididymis, prostate, seminal vesicles, Cowper’s glands Growth spurt initiated by testosterone levels Testosterone and DHT develop the secondary sex characteristics: larger muscles and bones, pubic hair, thick and tough skin, deep voice, facial and chest hair, increased sex drive Andropause Testosterone levels decrease about 1% per year after 40 years of age In the 70s and 80s, andropause occurs Andropause symptoms: decreased spermatogenesis, thinner ejaculate, less ejaculatory force, libido decreases, fatigue, mood disturbances, decreased strength Controversy over hormone treatments Male Reproductive and Sexual Health Diseases of the male reproductive organs Other conditions that affect the male reproductive organs Cancer of the male reproductive organs Diseases of the Male Reproductive Organs: Cryptorchidism Testes do not descend into the scrotum Surgery necessary to correct Although the testicles of a fetus begin high in the abdomen, they must descend into the scrotum during fetal development. If they do not, the male may become infertile. Diseases of the Male Reproductive Organs: Testicular torsion testis is twisted on its spermatic cord; many causes (sex, exercise, sleep); symptoms are pain and swelling; immediate surgery is required to maintain the testicle Testicular torsion can occur after exercise, sexual intercourse, and even while sleeping. Diseases of the Male Reproductive Organs: Priapism persistent, painful erection not related to sexual excitement; blood is trapped in erectile tissue; common causes are drug use and unknown; treatment is cessation of drug use and, possibly, surgery Diseases of the Male Reproductive Organs: Peyronie’s Disease painful curvature of the penis making penetration impossible; cause is unknown; may disappear within 2 years, or require drugs or surgery Other Conditions that Affect the Male Reproductive Organs Anabolic-androgenic steroid use synthetic testosterone can increase muscle mass and endurance; there are also numerous physical, psychological, and emotional side effects, including erectile problems Inguinal hernia intestine goes through an abdominal opening into the scrotum, creating a bulge; can be due to heavy lifting and straining; surgery may be required Hydrocele – fluid accrues & forms a scrotal mass Cancer of the Male Reproductive Organs Testicular Penile Prostate Testicular Cancer Most common cancer in men 15-44 years Few early symptoms, early detection important; testicular self-exam Symptoms: painless mass or hardness in the testes; pain or increase in size of the testes, lower back pain, gynecomastia, shortness of breath, urethral obstruction High cure rate: radiation, chemotherapy, removal of testicle Penile Cancer Lesions on the penis may be benign or malignant and are usually treatable; may also be a STI Penile cancer is not common Prostate Cancer Prostate glands enlarge with age and this is typically unproblematic, other than interfering with urination Prostate cancer is one of the most common in American men, typically in men over 50 years Risk factors: age, high fat diet, race, genetics Symptoms: pain in the lower back, pelvis, or upper thigh, and urinary abnormalities Detected through rectal exam and blood test Prostate Cancer Treatments: “watchful waiting”, radical prostatectomy, radiation, cryosurgery, drugs that attack cancerous cells