Headache Management
advertisement

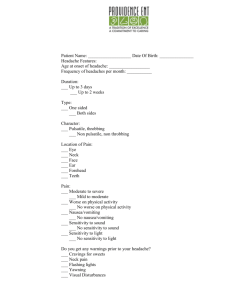
HEADACHE MANAGEMENT Elizabeth Treiber, MSN, CRRN, CNP NEONP Conference April 24, 2015 Disclaimers • Opinions contained in this presentation are the views of the author and do not necessarily reflect the views of the Department of Veterans Affairs • No conflicts of interest • Off label uses of several medications will be discussed (Thanks, Dr. Ronald Riechers, for your assistance with this presentation) OBJECTIVES Describe the difference between abortive and prophylactic headache medications. Apply pharmacodynamics of headache medications to case studies. Key Facts • Headache disorders are among the most common disorders of the nervous system. • It has been estimated that 47% of the adult population had at least one headache within the last year. • Accounts for 13 million office/ED visits per year • Approximately 1 in 30 people have a headache more days than not, for more than 6 months Approach to Headaches • Begins with proper identification of headache type • Classification is based on history and examination • Primary • Secondary Evaluation of Headaches • Quality of pain • Location of pain • Time of day pain occurs • Warning symptoms/aura • Precipitating factors • Symptoms associated with headaches • History of chronic or recurring headaches • Family history of headaches Clinical Evaluation – Examination • Vitals signs • Head and neck palpation • Neurologic examination • Signs of elevated ICP • Focal abnormalities of motor/sensory function • Cerebellar function • Reflexes Red Flag Symptoms (SNOOP) • Systemic Symptoms (fever, weight loss) • Secondary Risk Factors (underlying disease) • Neurologic Symptoms (confusion, focal exam) • Onset (sudden, abrupt—first, worst) • Older Age Onset (>50, giant cell arteritis) • Pattern Change (first headache or different) • Previous Headache History (frequency, severity) (Dodick, 2003) Types of Headaches Primary • Lack an underlying pathologic cause Secondary • Have an underlying systemic or local cause • Exceedingly rare cause of headache presentation—high level of patient anxiety Primary Headache Disorders Headache Type Characteristics Associated Symptoms Duration Epidemiology Migraine Uni/Bilateral Throbbing pain Worsened with physical activity Severe intensity Nausea/Emesis Photo/phonophobia 4-72 hours 10-15% of population, 3:1 F:M ratio TensionType Bilateral Pressure or band like pain Mild intensity Typically none 30 min – several hours 60-70% of primary headaches, equal M:F ratio Cluster Unilateral orbital or temporal Short duration severe pain Multiple attacks Lacrimation, rhinorrhea, congestion, ptosis, miosis, conjunctival injection 15-180 min, 1-8 attacks per day, lasting week to months <5% of primary headache disorders, 6:1 M:F Ratio Chronic Headache Medication Overuse Headache (Rebound) • overuse of analgesic meds>3/week • >15 headaches/month Chronic Migraine • > 8 HA days/month for at least 3 months • Not MOH or secondary cause Chronic Tension Type • >15/month • bilateral, non-throbbing, mild, able to continue activity Headache Episodic Headache Chronic Daily Headache •Characterize type •Abortive therapy •> 15 HA days per month •Analgesic rebound •Prophylaxis is key •Maximum 3 doses/week Avoid narcotics & Benzos Prophylaxis Abortive NSAIDs •GI side effects Ibuprofen Naproxen Sodium Aspirin Triptans •Contraindicated in patients with CAD Onset of action ~ 4 wks Combination Medications Alternatives Promethazine Metoclopramide •Cognitive side effects Prochloroperazine •Risk of W/D Tizanidine Non-medication Fioricet Trigger point injection Fiorinal Occipital nerve block Midrin Physical therapy Anti-depressants •May improve mood •Improves sleep AEDS Nortriptylline Amitryptilline Paroxetine Fluoxetine gabapentin •Mood lability valproic acid topirimate •Neuropathic pain Beta-blockers •Non-selective may have benefit on autonomic effects of PTSD Propranolol Tension Headache Medications Abortive Preventive • NSAIDS • TCA • Muscle Relaxants • SNRI • SSRI • Physical Therapy Migraine Headache Medications Abortive • Triptans • Antiemetics • NSAIDS • Dihydroergotamine Preventive • TCAs • (Amitriptyline, Nortriptyline) • Topiramate • Gabapentin • Betablockers • (propranolol) • Promethazine • Verapamil • Divalproex • Botox • Physical Therapy Cluster Headache Medications Abortive Preventive • Sumatriptan • Steroids • Zolmitriptan • Verapamil • Oxygen • Lithium Headache - Abortive • Fundamental principle #1- Limit frequency of abortives due to analgesic rebound headache • Ibuprofen, alleve, tylenol all may cause rebound headache (MOH) • Do not use more than 3 times/week • Fundamental principle #2- Avoid narcotics due to dependence risk, rebound headaches, cognitive/mood effects Abortive Therapies - Migraine • OTC preparations • Excedrin, Goody’s powders, tylenol, advil • May work for limited population • High risk of rebound headaches Abortive Therapies - Migraine • NSAIDs • Prescription agents may offer some benefit over OTCs • Naproxen is usually agent of choice • Long acting preferred over short acting Abortive Therapies - Migraine • Triptans • Migraine Designer drug • 5HT1B/1D agonists • Key is early dosing • No dependence risk but risk of analgesic rebound headache exists • Risk of vasospasm – CONTRAINDICATED IN PATIENTS WITH CAD/STROKE Triptans for Migraine • Sumatriptan (Imitrex) • Multiple preparations • Oldest • Zomig/Maxalt • ODT preparations • Frovatriptan • Long acting agent Triptans (Sumatriptan, zolmitriptan) • Pharm Category—Serotonin 5-HT Receptor Agonist • Use—acute treatment of migraine or cluster HA • Mechanism of action—causes vasoconstriction in cranial arteries • • • • and reduces neurogenic inflammation Contraindications—ischemic heart disease, cerebrovascular syndromes, peripheral vascular syndromes, uncontrolled HTN, hepatic impairment, use within 2 weeks of MAO inhibitor Caution—Sulfa allergies, seizure history **Serotonin Syndrome** see next slide Dosage—Sumatriptan 50mg at onset of severe headache, may repeat in 1-2 hours if needed—if needs to repeat every HA, increase to 100mg at onset Serotonin Syndrome • American Headache Society published a position paper in 2010 which states: “the available evidence does not support limiting the use of triptans with SSRIs or SNRS due to concerns for serotonin syndrome. Based upon their pharmacology, the involvement of triptans in contributing to a serotonin syndrome, either alone or in combination with other medications, seems implausible.” http://www.headachejournal.org/SpringboardWebApp/userfiles/h eadache/file/fda.pdf Combination Therapies (old and cheap) • Fioricet/Fiorinal • Caffeine + barbiturate + acetaminophen or ASA (butalbital) • Dependence risk/High risk of analgesic rebound • MAJOR RISK OF SEIZURE/DEATH WITH ABRUPT CESSATION IN DAILY USER • Midrin (acetaminophen, dichloralphenazone, isometheptene) • Treximet (sumatriptan 85 and naproxen 500) Abortive Therapies - Migraine • Anti-Nausea agents • Promethazine, Metoclopramide, Prochloperazine, Theoretical mechanism based on dopaminergic theory of migraine • NO RISK OF ANALGESIC REBOUND • Caution in chronic use (EPS) (Extrapyramidal symptoms (EPSs), such as akathisia, dystonia, psuedoparkinsonism, and dyskinesia, are drug-induced side effects that can be problematic for persons who receive antipsychotic medications (APMs) or other dopamine-blocking agents.) Promethazine • Pharm Category—Anti-emetic • Use—anti-emetic • Mechanism of action—blocks dopaminergic receptors in the brain, alpha adrenergic blocker • Contraindications—hypersensitivity • Caution—can be sedating, can lower seizure threshold, can elevate prolactin levels so caution in breast cancer, may alter cardiac conduction, has anti-cholinergic effects • Dosing—12.5mg at for nausea associated with migraine HA, may take every 6 hours until HA relieved Headache - Prophylaxis • Typical onset of action is 4 weeks on prophylaxis • Abortive agents should not be used on a daily basis or for prophylaxis • Prophylactics: • Tricyclic Antidepressants (TCAs) • Anti-epileptics (AEDs) • Beta Blockers • Anti-emetics • Prazosin TCA’s (Amitriptyline, nortriptyline) • Pharm Category—tricyclic antidepressant • Use—antidepressant • Unlabeled/Investigational—analgesic for certain chronic and • • • • neuropathic pain, prophylaxis against migraine headaches Mechanism of action—increases synaptic concentration of serotonin and/or norepinephrine in the CNS by inhibition of their reuptake by the presynaptic membrane Contraindications—use of MAO inhibitors within past 14 days, acute recovery phase after MI, pregnancy Precautions—may cause drowsiness, do not abruptly discontinue Dosage—Amitriptyline—10mg at bedtime for one week, then 20mg at bedtime Headache Prophylaxis • Amitriptyline or Nortriptyline • Tricyclic antidepressant • Helpful if impaired sleep is also an issue • Useful if also having tension headache • Check for history of cardiac arrythmias or seizures • Check for suicide risk—warn about possible risk of suicide—be sure has suicide prevention number • Start 10mg at hs for 7 days, then increase to 20mg at hs Anti-Epileptics: Topiramate (TPM), valproate (VPA), gabapentin (GBP) • Pharm Category—Anticonvulsant • Use—TPM and PVA are FDA approved for prevention of • • • • • episodic migraines, GBP is useful in migraine prevention based on a few clinical trials Unlabled/Investigational—neuropathic pain, migraine, cluster headaches Mechanism of action—thought to block sodium channels in neurons, enhancing GABA activity and by blocking glutamate activity Contraindications—history of kidney stones for TPM Precautions—avoid abrupt withdrawal due to increased risk of seizures, caution in hepatic/renal/pregnancy Adverse reactions—somnolence, dizziness, nausea Headache - Prophylaxis • Topiramate • • • • • • Anticonvulsant Great migraine headache data Memory impairment/word finding difficulty possible side effects Weight loss Renal stones in 1% of patients on higher doses Start 25 mg qhs or bid titrate to NMT 100 mg bid Headache - Prophylaxis • Valproic Acid ▫ Good headache data ▫ Beneficial for mood lability/aggression ▫ Cons- teratogenicity, poor side effect profile, drug interactions, hepatotoxicity ▫ ER version preferable, start 500 mg daily titrate to 1500-2000 mg daily, follow labs Gabapentin • Pharm Category—anti-convulsant • Use—adjunct for treatment of seizures • Unlabeled—chronic pain • Mechanism of action—exact mechanism unknown • Contraindications—hypersensitivity • Caution—renal disease, may cause sedation, avoid abrupt withdrawal • Dosage—titrate to 300mg three times daily Headache - Prophylaxis • Gabapentin • Data not as robust as other AEDs • Benefit for neuropathic pain, anxiety, ?sleep • Pros- tolerable side effect profile, minimal drug interactions • Start 300 mg qhs, titrate up to 600-900 mg tid Beta Blockers (Propranolol) • Pharm Category—Beta Blocker • Use—HTN, tachycardia, arrythmias, migraine headaches • Mechanism of action—non-selective beta-adrenergic blocker • Contraindications—CHF, bradycardia, asthma, COPD, pregnancy • Caution—hepatic dysfunction, PVD • Dosage—Propranolol 10 mg twice daily—if helping, change to 60mg LA daily Headache - Prophylaxis • Propranolol • Non-selective, lipid soluble Beta blocker • Pros- Effect on agitation, autonomic symptoms of PTSD • Cons- Impact exercise tolerance, possible ED • Caution with use of prazosin and in patients with asthma • Do not use in 2nd and 3rd trimesters • Start 10 mg bid, titrate as tolerated • Transition to 60mg LA for once daily dosing Prazosin—More Bang for Your Buck • Pharm Category—Alpha blocker • Use—treatment of HTN • Unlabeled—management of nightmares, headache prophylaxis • Mechanism of action—inhibits postsynaptic alpha-adranergic receptors (Alpha Blocker) • Contraindications—hypersensitivity to quinazolines • Caution—may cause orthostatic hypotension and syncope • Dose—1mg at bedtime for one week, then 2mg at bedtime for one week—titrate to 4 to 6mg—may increase dose to 10-15 mg http://www.ncbi.nlm.nih.gov/pubmed/12562588 http://www.medscape.com/viewarticle/760070 Botox • For adults with Chronic Migraine—15 or more headache days a month, each lasting 4 hours or more—FDA-approved, preventive treatment. • Not approved for adults with migraine who have 14 or fewer headache days a month. • Receive injections into multiple facial muscles every 3 months http://www.ncbi.nlm.nih.gov/pubmed/20487038 http://onlinelibrary.wiley.com/doi/10.1111/j.1526-4610.2010.01678.x/full Drug Interactions Headache Drug PTSD Drug Interaction Tricyclic Antidepressants SSRIs Inc TCA levels 2) Serotonin syndrome Triptans SSRIs Serotonin Syndrome* Prazosin Additive lowering of BP, orthostasis Benzodiazepine Additive increase in sedation Propranolol Tricyclic Antidepressants 1) Deciding which medication to use (Liz’s Pearls) • Be sure not MOH headache (Rebound headache) • Hx kidney stones—NOT topiramate • Hx cardiac issues—NOT amitriptyline • Hx suicidal ideation—NOT amitriptyline • Bradycardic—NOT propranolol • Neuropathic pain—gabapentin or topiramate • Frequent migraines—topiramate • Sleep issues—amitriptyline • Weight issues—topiramate • Try PRAZOSIN! Education • Education is the single most important step in helping patients manage their headaches. • Hand-outs from American Headache Society • Medication Overuse Headaches • Triggers • Non-pharmacologic Management Headache Journal • Date • Time • Intensity • Preceding Symptoms • Triggers • Medication • Relief http://www.achenet.org/assets/1/7/Monthly_Headache_Diary.pdf http://www.headaches.org/pdf/Headache_Diary.pdf Triggers • Stress • Bright lights • Lack of sleep • Foods—nitrites, nitrates, aged cheese, MSG, raw onions, chocolate, caffeine (see National Headache Foundation Low Tyramine Headache Diet) https://www.headaches.org/pdf/Diet.pdf Interdisciplinary Team Approach • Behavioral Psychologist • Headache medication education • Triggers • Headache diary • Sleep hygiene • Relaxation techniques • Biofeedback • SootheAway Machine • Physical Therapy • Neck exercises/stretches • Dry needling • Trigger Point Injections Case Study # 1 – Cody • 22 y/o male c/o headaches 3-4 days/week • Hx brief LOC in high school baseball game and brief LOC after IED explosion in Afghanistan 2011 • What do you want to know? • Gets HA 3-4 days/week—some mild, some severe • HAs occur randomly throughout the day • Takes tylenol 2-3 times/week—helps mild HA but • • • • • just dulls pain for severe HA Pain—throbbing, center of forehead Feels like he “hears his heartbeat” in his head Phonophobia with severe HA, no photophobia Gets nauseated with severe HA Severe HA lasts a couple of hours, stops activities, lays in dark room with cold cloth on head • What else do you want to know? • PM Hx: • PTSD (sleeps 3-4 hours/night) • Hematuria twice in past—work-up was negative— intermittent right flank pain continues and is sometimes quite severe • Meds: • Sertraline 50mg daily • Trazodone 100mg at hs prn sleep • Tylenol prn headache • Soc Hx: • ETOH—2-3 beers/night • ½ PPD • Caffeine—one cup coffee in am, energy daily prior to working out • Physical Exam: • BP 134/78, P 100 • Neurologic exam is normal • What type of headache? • What meds would be appropriate or not appropriate? • What instructions should be given to patient? • Type of headache • Episodic Migraine • Appropriate Meds • Abortive: • Triptan for migraine—caution about frequency of use • Promethazine—nausea and helps with HA pain • Preventive: • TCA (interaction with SSRI) • Topiramate (hematuria, flank pain) • Propranolol (patient is tachycardic, good for tension HA) • Prazosin (helps with sleep) • Instructions • Caution about MOH headache • Decrease caffeine intake • Non-pharm mgmt—thermal, trigger foods, HA diary Case Study # 2 – David • 28 y/o male, gets daily headaches • Hx concussion without LOC in 10/2005 after IED explosion, concussion with LOC 11/2005 after IED explosion • What do you want to know? • HAs occur daily—50% are mild (3/10) with pain located in forehead—50% are severe with pain behind right eye • HAs last 4-6 hours--takes tylenol and it helps except for the really bad headaches • Phonophobia and photophobia • Occasionally nauseated • Must go lay down in quiet, dark room • Has not tried cold cloth • PM Hx: • Intermittent chest pain for last 6 weeks—ECG wnl, to see GI next week • Constant low back and hip pain—occasional numbness/tingling in left leg—waken at night due to back pain • Meds: • Vitamin D • Nexium • Tylenol several times/day for HA and back pain • Social History: • No etoh, no tobacco, one soda/day with lunch • PE: • BP 124/86 P 74 • Neuro exam wnl except for back pain with heel walk • What type of headache? • What meds would be appropriate or not appropriate? • What instructions should be given to patient? • Type of headache: • Medication overuse headache (rebound) • Episodic migraine • Medications: • Abortive: • Triptans (caution on overuse) • Prophylactic: • Propranolol (pulse 74) • Topiramate (no hx kidney stones) • Amitriptyline (recent chest pain) • Gabapentin (helps with back pain & sleep) • Prazosin (not having PTSD sxs) • STOP DAILY TYLENOL USE Case Study #3 – Nancy • 42 y/o female • Mild headaches 3-4 times/week • Severe headache once/month • Mild headaches start in her neck and progress upward into head • Usually occur in the afternoon and evening • No N/V or photophobia/phonophobia • Able to continue with her activities • Severe HA occurs approx once/month around the time of her menses— photophobia—must lay in dark room with cold cloth on head • PM Hx: • Was in MVA 5 years ago—cervical strain • Meds: • Vitamin D • MVI • Synthroid 50mcg • Social History • Glass of wine with dinner • No tobacco • 5-6 cups of coffee/day • 3 school age children, elderly parents, works full time, recently returned to school • PE • BP 130/74, P 76 • Neuro exam wnl • What type(s) of headache? • What meds would be appropriate or not appropriate? • What instructions should be given to patient? • What type of headache? • Tension or cervicogenic • Menstrual migraine • What meds would be appropriate or not appropriate? • Tension • Tizanidine (muscle relaxant) (abortive) • NSAIDS (abortive) • (caution rebound HA) • Amitriptyline (prophylactic if frequency increases) • Menstrual Migraine • Naproxen 500mg BID starting 3-5 days prior to menses • Triptan • What instructions should be given to patient? • Decrease caffeine intake Case Study #4 -- Aaron • 36 y/o Army veteran with history of mild TBI/concussion--involved in fire fight in Iraq in 2004--received blow to head possibly from Humvee door-could not see or hear for several minutes--felt dazed--unable to carry out his duties for several minutes. • Veteran gets migrainous type headaches approximately 2-3 times/month—pain left side of head—photophobic— phonophobic—blurred vision—must go lay down in dark room. • Veteran describes the worst headache of his life occurring approximately one month ago--3 days prior to this headache veteran had significant difficulty operating a machine at work that he was normally proficient in operating--his headache has waxed and waned in intensity since then but has not ever completely resolved. His dizziness with position change has increased during this time. • Neuro exam is wnl except for MOCA exam which is 25/30 (normal is 26/30). • Meds: fluoxetine 60mg daily • Veteran is currently taking alleve or motrin on a daily basis for this headache. • Veteran is otherwise functioning quite well--he is maintaining full time employment, engaged with his family, and in general good spirits. What do you do now? • What type of headache? • Concerns? • Ideas for treatment? • What instructions should be given to patient? Plan: • MRA/MRI of head ordered to be done asap • (worst headache red flag, neuro symptoms of forgetfulness) • Stop daily use of any pain medications, including alleve and motrin--these may cause rebound headaches • Start promethazine 12.5mg prn for current daily headache-may take with alleve, but again, do not use alleve more than 2-3 times/week or rebound headaches may occur • Start sumatriptan 50mg at onset of severe headache--do not take more than twice/week or rebound headaches may occur. • Follow up with neurology after MRA/MRI has been completed. Follow Up • MRI/MRA wnl • Continue sumatriptan and promethazine—both are working well • Abbreviated Neuro-Psyche eval wnl • Consult Behavioral Medicine for education and SootheAway machine • Encourage continued f/u with mental health Case Study # 5 -- Brandon • 22 y/o OIF/OEF National Guardsman--sustained a mild TBI/concussion while deployed to Afghanistan in 2013--exposed to multiple explosions while doing route clearance--on one occasion he felt dazed/dizzy/confused immediately afterward and "out of it" the rest of the day--no LOC--after several other explosions he felt dazed for very short period of time. • Daily headaches--occasionally last all day long— continues with activities—5/10 pain • Bad headache occurs every 3-4 days—must go in dark/quiet room—9/10 pain • Nauseated • Neck also hurts • Photophobic/phonophobic • Cold water on face helps • Takes tylenol or ibuprofen on almost daily basis • Pain sometimes starts in neck and works its way up • Difficulty with sleep initiation--wakes at slightest noise-- nightmares almost every night--irritable--hyperalert--does not like to go into crowds. • Neuro exam is wnl except for fine tremor in bil UE--right more than left--numb area in lateral aspect of right calf--and MOCA score of 18/30 (normal is 26 and above). • Only prescribed medication is etodolac 400mg every 6 hours as needed for pain • VS are wnl • No history of kidney stones or heart disease What do you do? • What type of headache? • Instructions to patient? • Treatment ideas? Plan • Stop daily use of any analgesic including tylenol, ibuprofen, etodalac as these may be causing rebound headaches--use no more than 3 times/week. • Start prazosin for nightmares/restless sleep/headache prophylaxis. Take 1mg at bedtime for one week, then 2mg at bedtime for one week, then 3 mg at bedtime for one week, then 4mg at bedtime. Be careful when getting out of bed because you might feel dizzy. • Start sumatriptan 50mg at onset of migrainous type headaches. May repeat in two hours if not effective. Do not take more than twice/week or rebound headaches may occur. • Consult Behavioral Medicine, Neuro-psyche testing, physical therapy Follow Up One Month Later • Veteran is currently sleeping better--he is not as wakeful and nightmares are slightly less frequent-he is now sleeping 6-7 hours/night instead of 4 hours/night. • Mental health prescribed sertraline 50mg daily. • Headaches are better with use of sumatriptan, however veteran is taking the sumatriptan approx 3 times/week. • Now What? Add Prophylactic Medication • Which one? • Any other medication adjustments? • What instructions should be given to patient? Next step • Start topiramate for headache prophylaxis. Take 25mg at bedtime for one week, then take 50mg at bedtime. • Increase sumatriptan to 100mg at onset of severe headache-- may repeat in 2 hours if needed. Do not take more that twice/week or rebound headaches may occur. • In 2 weeks, after topiramate dose has been titrated to 50mg, then increase the prazosin to 5mg at bedtime for one week, then 6mg at bedtime in an effort to continue to improve sleep and decrease nightmares. Wait two weeks to initiate increase in prazosin so increase in prazosin does not occur at the same time as initiation of topiramate. • Continue f/u with mental health providers. Case Study #6 – D.R. • 43 y/o male injured during football game while training with National Guard in Virginia in 2011—had C2-C7 posterior cervical laminectomy—is currently able to ambulate without a device—good control of bowel/bladder—has ongoing neck and upper back pain, headaches. Case Study #6 (continued) • Headaches—pain shoots up from neck or chin area-- occurs without warning several times/day--electrical and squeezing pain--occurs on both right and left side--eyes occasionally tear during these episodes--these shooting HAs have been increasing in frequency--also gets throbbing headache 3-4 times/week--photophobic--last 30 minutes to 60 minutes--must occasionally go into dark room and rest. Has seen PT for dry needling--is doing neck stretches and HEP on daily basis. Currently has throbbing headache. Neck and shoulder pain--takes oxycodone for neck and shoulder pain approx once/week-takes ibuprofen twice/day--occasionally skips the middle of the day dose of gabapentin unless needed--Pulse 82100. • What type of headache? • What instructions to patient? • What meds would be appropriate? Plan • Instructed veteran to try to decrease ibuprofen to not more than 3 times/week--concern that ibuprofen may be causing rebound headaches-possible consideration of naproxen instead of ibuprofen for longer effect with less doses. • Take gabapentin 900mg every 8 hours as ordered—this will help with pain management and also headache prophylaxis. • Start propanolol 10mg twice daily for headache prophylaxis. Follow Up • Good results with propranolol 10mg twice daily—changed to propranolol SA 60mg once daily • Better pain control with use of gabapentin every 8 hours (Can also help with headache prophylaxis) RESOURCES Prazosin—Results of One Study • Ruff et al. • Nonrandomized, controlled trial of 80 OIF vets • Headaches, cognitive function, daytime sleepiness Ruff RL et al. JRRD 2009;46:1071-84 For the Entire Study Group, Prazosin Improved Performance Table 1: Impact of Intervention consisting of sleep hygiene counseling & prazosin on daytime sleepiness (ESS), cognitive function (MOCA) & headaches Performance of veterans at baseline and after intervention (N=74) ESS Scores (0-24) MOCA Score (0-30) Headache Pain Intensity (0-10) Headache Frequency (#/month) Baseline 16.1 + 0.28 24.5 + 0.49 7.28 + 0.27 12.4 + 0.94 After Sleep Hygiene & Prazosin 7.28 + 0.34 (p<0.001) 28.6 + 0.59 (p<0.001) 4.08 + 0.19 (p<0.001) 4.77 + 0.34 (p<0.001) The Benefits of Prazosin Lasted Table 3: Comparison of the veterans who were or were not taking prazosin 6 months after completion of the study period. Performance of veterans 6 months after the study period ESS Scores (0-24) MOCA Score (0-30) Headache Pain Intensity (0-10) Headache Frequency (#/month) Taking Prazosin (64) 3.97+ 0.18 29.0 + 0.13 2.39 + 0.12 1.88 + 0.14 Not Taking Prazosin (10) 10.5 + 0.58 24.8 + 0.51 5.80 + 0.29 7.00 + 0.54 (p<0.001)* (p<0.001)* (p<0.001)* (p<0.001)* 4.85+ 0.31 28.4 + 0.21 2.85 + 0.17 2.57 + 0.25 All subjects (74) * comparison of veterans taking vs. not taking prazosin Indications for Neuro-Imaging Evans RW. CONTINUUM: Lifelong Learning in Neurology 2006;12:213-234 Secondary Headache – Etiology • CNS causes • Non-CNS Causes • Mass Lesion • Vasculitis/GCA • Aneurysm • Infection • Venous sinus thrombosis • Glaucoma • Arterial dissection • Cervicogenic headache • Chronic menigitis • Malignant HTN • CSF hypotension • Drugs (illicit and prescribed) Secondary Headache Posttraumatic Headache • Start within 7 days of trauma, milder, neck trauma Vascular Headache • Ischemia, vasculitis, hemorrhage, giant cell arteritis Remember Red Flags • Neuroimage: new neuro signs, new sudden onset severe HA, HIV + with new HA, > 50 y/o with new type HA VA Pharmacy Newsletter June 2013 • • • • • • • • • • • Risk of Serotonin Syndrome with Triptans and SSRIs/SNRIs Prepared by Roland Rovito, PharmD – Inpatient Pharmacist The concurrent prescribing of 5-hydroxytryptamine receptor agonists (“triptans”) and either selective serotonin reuptake inhibitors (SSRIs) or serotonin/norepinephrine reuptake inhibitors (SNRIs) is a controversial clinical topic due to concerns regarding serotonin syndrome (SS), an adverse drug reaction that results from increased synaptic serotonin levels. Clinical features include mental status changes, dysautonomia, and neuromuscular dysfunction; severity can range from mild to lifethreatening. Cases usually occur within 24 hours of serotonergic medication changes and are thought to be underreported due to their sudden onset, transient nature, and low level of harm perceived by patients. Based upon case reports, the Food and Drug Administration issued an alert regarding potential “life-threatening” SS in patients on both a triptan and SSRI or SNRI in 2006. The quality of the reports used has been debated, as many cases fail to meet diagnostic criteria for SS; however, it must be noted that these criteria have not been validated for use in post-marketing safety reports. The mechanism for SS secondary to triptan use has also been debated, as animal models implicate 5-HT2A and possibly 5-HT1A receptors in SS; at common doses, triptans have high affinity for 5-HT1B, 5-HT1D, and 5-HT1F receptors, low affinity for 5-HT1A receptors, and no activity at 5-HT2A receptors. While chronic high-dose triptan use has shown increased serotonin synthesis in animal models, acute triptan use has contrarily shown autoreceptor activation and decreased serotonin synthesis and release, possibly preventing SS. Given the high comorbidity of migraine with certain psychiatric disorders, it is not surprising that 20-25% of patients treated with triptans also take an SSRI or SNRI. The concurrent use of these medications may be needed for effective treatment, and avoiding co-prescription due to potential SS may lead to unnecessary morbidity and decreased quality of life. Therefore, while the number of patients experiencing SS due to concurrent triptan and SSRI or SNRI use remains unknown and further study into this adverse drug reaction is needed, it is difficult to use current evidence to rationalize the avoidance of this combination. For select patients, the benefits of clinically-appropriate concurrent therapy likely outweigh the risk of SS, and as such, these medications may cautiously be used together. Patients should be educated on SS and it would be advised for providers to document that the risks versus benefits were evaluated and discussed with the patient. References: Evans RW, Tepper SJ, Shapiro RE, Sun-Edelstein C, Tietjien GE. The FDA alert on serotonin syndrome with use of triptans combined with selective serotonin reuptake inhibitors or selective serotonin-norepinephrine reuptake inhibitors: American Headache Society Position Paper. Headache. 2010;50(6):1089-1099. Fine A, Bastings E. Triptans and serotonin syndrome [letter]. Headache. 2012;52(7):1184-1185. Sclar DA, Robison LM, Castillo LV, et al. Concomitant use of triptan, and SSRI or SNRI after the US Food and Drug Administration alert on serotonin syndrome. Headache. 2012;52(2):198-203. Tepper SJ, Shapiro RE, Sun-Edelstein C, Evans RW, Tietjen GE. Triptans and serotonin syndrome – a response [letter]. Headache. 2012;52(7):1185-1188. Wenzel RG, Tepper S, Korab WE, Freitag F. Serotonin syndrome risks when combining SSRI/SNRI drugs and triptans: Is the FDA’s alert warranted? Ann Pharmacother. 2008;42(11):1692-1696. Triptans for Migraine Loder E. NEJM 2010;363:63-70. Prophylaxis - Evidence Loj J, Solomon GD. Clev Clin J Med 2006;73:793-816 References/Resources • Evans, R. W., Tepper, S. J., Shapiro, R. E., Sun-Edelstein, C., Tietjen, G. E. (2010). The FDA alert on serotonin syndrome with use of triptans combined with selective serotonin reuptake inhibitors or selective serotonin-norepinephrine reuptake inhibitors: American Headache Society position paper. Headache 2010; 50: 1089-1099. • http://www.americanheadachesociety.org/professional_resourc es/headache_fact_sheets/ (Chronic daily headache, Concussion and post-traumatic headache, Generalized anxiety, PTSD & migraine, How to choose a preventive medication for migraine, Triptan therapy for acute migraine, Migraine overuse headache) • http://www.americanheadachesociety.org/professional_resourc es/headache_journal_toolboxes/ (Headache after sportsrelated concussion, Post-traumatic headache in veterans, Triptans SSRIs/SNRIs and serotonin syndrome) References/Resources (Continued) • Lipton, R. B., Serrano, D., Nicholson, R. A., Buse, D. C., Runken, M. C., & Reed, M. L. (2013). Impact of NSAID and triptan use on developing chronic migraine: Results from the American migraine prevalence and prevention (AMPP) study. Headache 2013; 53: 1548-1563. • Loder, E., Weizenbaum, E., Frishberg, B., & Silberstein, S. (2013). Choosing wisely in headache management: The American Headache Society’s list of five things physicians and Patients should question. Headache, 2013; 53:1651-1659. • Marshall, R. S., & Mayer, S. A. (2007). On call neurology. Philadelphia, PA: Saunders Elsevier. • Ruff, R. L., Riechers, R. G., & Ruff, S. S. (2010) Relationship between mild traumatic brain injury sustained in combat and post-traumatic stress disorder. F1000 Med Rep.2010: 2:64. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2990449/ References/Resources (Continued) • Ruff, R.L, Ruff, S.S., Wang, X. (2009) Improving sleep: • • • • Initial headache treatment in OIF/OEF veterans with blast induced mild traumatic brain injury. JRRD 2009;46:1071-84 Tepper, S. J., & Tepper, D. E. (Eds.). (2012). The Cleveland Clinic manual of headache therapy. New York, NY: Springer. Turkowski, B. B., Lance, B. R., Bonfiglio, M. F. (2005). Drug information handbook for advanced practice nursing. Hudson, OH: Lexicomp. Westover, M. B., Choi, E., Awad, K. M., Greer, D. M. (Eds.). (2010) Pocket neurology. Philadelphia, PA: Lippincott Williams & Williams. Whyte, C. A., Tepper, S. J. (2010). Pearls & Oy-sters: Trigeminal autonomic cephalalgias. Neurology, 2010:74: e40-e42. • Headache Disorders, WHO Fact Sheet N277, October 2012