Note 1 Reproduction
advertisement

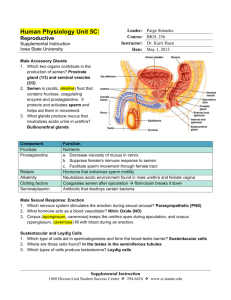
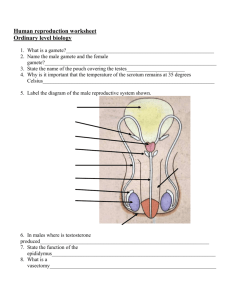
Reproduction The structure and function of reproductive organs and gametes and their role in fertilisation. Gamete production in the testes. The roles of seminiferous tubules, interstitial cells, testosterone, prostate gland and seminal vesicle Gametes are produced from germline cells. Testes produce sperm in the seminiferous tubules and testosterone in the interstitial cells. The prostate gland and seminal vesicles secrete fluids that maintain the mobility and viability of the sperm. Male reproductive system The diagram shows the male reproductive system Sperm cells are produced from germline cells in the seminiferous tubules in the testes. Sperm duct testis Seminiferous tubule The male sex hormone testosterone is produced by cells, called interstitial cells, in the tissue between the seminiferous tubules Structure Function Seminiferous Produce sperm Seminiferous tubules tubules Germline cell Interstitial cell Interstitial cells Seminal vesicles Prostate gland Produce testosterone Secretion contains fructose, which provides energy for movement of the sperm and substances that stimulate contraction of the female reproductive tract allowing sperm to reach the oviduct more quickly Secretion has enzymes that maintain the correct viscosity of the liquid in which the sperms swim Seminal vesicles and prostate gland The liquid released by the male is called semen, it contains sperm and secretions from the seminal vesicles and prostate gland. The seminal vesicles release a liquid containing fructose, which provides energy for the sperm to move and also substances that stimulate contractions of the female reproductive tract allowing the sperm to reach the oviduct more quickly. The secretion of the prostate gland contains enzymes that keep the fluid at the correct viscosity for sperm to swim. Gamete production in the ovaries to include maturation of ova and the development of a follicle. Each ovum is surrounded by a follicle that protects the developing ovum and secretes hormones. Female reproductive system Eggs are formed from germline cells in the ovaries. Ovaries contain immature eggs at various stages of development. Each egg is surrounded by a follicle that protects the egg and secretes the hormone oestrogen. After ovulation (release of an egg), the follicle develops into the corpus luteum, which secretes the hormone progesterone. The diagram shows the female reproductive system (oviduct) egg Corpus luteum follicle after ovulation Site of fertilisation in the oviduct and zygote formation. Mature ova are released into the oviduct where they may be fertilised by sperm to form a zygote. If fertilisation (fusion of a sperm and egg nucleus) occurs following ovulation, it takes place in the oviduct Follicle secretes the hormone oestrogen Corpus luteum secretes the hormone progesterone Hormones control the onset of puberty, sperm production and the menstrual cycle. Pituitary gland releases follicle stimulating hormone (FSH),luteinising hormone (LH) or interstitial cell stimulating hormone (ICSH) The pituitary gland is stimulated to release follicle stimulating hormone (FSH) and luteinising hormone (LH)/interstitial cell stimulating hormone (ICSH) by a releaser hormone produced in the hypothalamus Hormones Hormones are chemical messengers released into the blood by endocrine glands. Hormones travel around the body in the blood but have an effect only on the target tissue of the hormone. Hormones control the onset of puberty, sperm production in males and the menstrual cycle in females. Control of onset of puberty At puberty, the hypothalamus secretes a releaser hormone which stimulates the pituitary gland to produce follicle stimulating hormone (FSH) and a second hormone known as luteinising hormone (LH) in females and interstitial cell stimulating hormone (ICSH) in males. Diagrams indicate position of hypothalamus and pituitary gland and need not be memorised The release of these hormones begins sperm production in males and the menstrual cycle in females. Hormonal control of sperm production. FSH promotes sperm production and ICSH stimulates the production of testosterone. Testosterone also stimulates sperm production and activates the prostate gland and seminal vesicles. Negative feedback control of testosterone by FSH and ICSH. Hormonal control of sperm production FSH promotes sperm production in the seminiferous tubules. ICSH promotes production of testosterone by the interstitial cells. Testosterone stimulates sperm production by the seminiferous tubules and activates the seminal vesicles and prostate gland to produce their secretions. Negative feedback control of testosterone production High concentration of testosterone inhibits secretion of ICSH (and FSH) resulting in decreased testosterone production – this is negative feedback Pituitary Gland Produces ICSH Interstitial Cells Produce testosterone Seminiferous Tubules Produce sperm The pituitary gland releases ICSH and FSH ICSH stimulates release of testosterone from the interstitial cells Increased concentration of testosterone in the blood inhibits production of ICSH and FSH from the pituitary gland This in turn decreases production of testosterone (this is an example of negative feedback) Hormonal control of the menstrual cycle. Development of a follicle and the endometrium in the uterus. Roles of FSH, LH, oestrogen and progesterone in the menstrual cycle. Development of a follicle, the corpus luteum and the endometrium. Hormonal control of the menstrual cycle FSH stimulates development of the follicle and stimulates the ovaries to secrete the hormone oestrogen. LH causes ovulation (egg release) and development of the corpus luteum from the follicle, it then stimulates the corpus luteum to secrete the hormone progesterone. Oestrogen and progesterone are called ovarian hormones. Effects pf ovarian hormones Oestrogen Stimulates cell division in the endometrium (uterus lining) repairing it following menstruation and preparing it for implantation. Stimulates secretion of LH by the pituitary gland. Progesterone Causes thickening and vascularisation (development of blood vessels) of the endometrium. Inhibits secretion of FSH and LH by the pituitary gland. The menstrual cycle takes approximately 28 days with the first day of menstruation regarded as day one of the cycle. The menstrual cycle The diagram shows changes occurring during the menstrual cycle Change in thickness of the endometrium (uterus lining) during the menstrual cycle Corpus luteum develops from the follicle Spike in LH causes ovulation High level of oestrogen during the first half of the cycle (follicular phase) and of progesterone during the second half (luteal phase) Increase in body temperature at ovulation Follicular and luteal phases. FSH stimulates the development of a follicle and the production of oestrogen by the follicle in the follicular phase. Oestrogen stimulates proliferation of the endometrium preparing it for implantation Peak levels of oestrogen stimulate a surge in the secretion of LH which triggers ovulation. In the luteal phase the follicle develops into a corpus luteum and secretes progesterone. Progesterone promotes further development and vascularisation of the endometrium preparing it to receive a blastocyst if fertilisation occurs. Menstrual cycle The first half of the cycle (before ovulation) is called the follicular phase. The second half (after ovulation) is the luteal phase. Follicular phase FSH stimulates Development of the follicle Release of oestrogen from the ovary Oestrogen causes thickening of the endometrium then at about day 14 of the cycle peak levels of oestrogen cause a surge in LH from the pituitary gland. This surge in LH causes ovulation. Luteal phase LH stimulates the follicle to develop into the corpus luteum. The corpus luteum produces the hormone progesterone. Progesterone stimulates further thickening and vascularisation of the endometrium preparing it to receive a blastocyst (early embryo stage) if fertilisation occurs. The negative feedback effect of the ovarian hormones on the pituitary gland and the secretion of FSH and LH prevent further follicles from developing. The lack of LH leads to degeneration of the corpus luteum with a subsequent drop in progesterone levels leading to menstruation. Negative feedback High levels of ovarian hormones during the luteal phase inhibit the release of FSH and LH from the pituitary gland so preventing development of any more follicles. Degeneration of the corpus luteum If fertilisation does not occur, lack of LH leads to degeneration of the corpus luteum, the resulting drop in progesterone triggers menstruation Oestrogen affects the consistency of cervical mucus making it more easily penetrated by sperm. Blastocyst implantation. Cervical mucus The cells lining the cervix at the opening of the uterus produce mucus. High levels of oestrogen lead to the production of a watery mucus that sperm swim through easily. Since the highest levels of oestrogen occur just before ovulation, producing watery mucus increases the chances of fertilisation. High levels of progesterone lead to production of thick mucus that sperm cannot easily pass through. Blastocyst implantation If an egg is fertilised by a sperm, the process occurs in the oviduct. A fertilised egg is called a zygote. The zygote divides as it moves down the oviduct to produce a ball of cells called a blastocyst. When it reaches the uterus, the blastocyst becomes embedded in the thickened uterus lining – this is called implantation. Fertile periods. Cyclical fertility in females leading to a fertile period. Continuous fertility in males. Calculation of fertile periods and their use. Fertile periods Males are continuously fertile, females show cyclical fertility, their fertile period occurring 1-2 days after each ovulation Calculating the fertile period Body temperature and thickness of cervical mucus can be used as indicators of the fertile period. This information is useful to those wanting to conceive and wishing to know when this is most likely to occur. Temperature Approximately 1 day after the LH surge that results in ovulation, the body temperature of a female rises by about 0.2 – 0.5oC due to the effect of progesterone and remains elevated during the luteal phase. Fertile period lasts 1 to 2 days, the infertile period resuming, on average, the third days after recording of the higher temperature. Cervical mucus Cervical mucus produced during the fertile period is thin and watery, allowing sperm to pass through it more easily. After ovulation the mucus becomes more viscous due to the action of progesterone. Treatments for infertility. Stimulating ovulation. Ovulation stimulated by drugs that prevent the negative feedback effect of oestrogen on FSH secretion. Other ovulatory drugs mimic the action of FSH and LH. These drugs can cause super ovulation that can result in multiple births or be used to collect ova for in vitro fertilisation (IVF) programmes. Artificial insemination. Several samples of semen are collected over a period of time. If a partner is sterile a donor may be used Artificial insemination is particularly useful where the male has a low sperm count. Intra-cytoplasmic sperm injection (ICSI). If mature sperm are defective or very low in number ICSI can be used — the head of the sperm is drawn into a needle and injected directly into the egg to achieve fertilisation. Infertility treatments Stimulating ovulation Infertility can be due to failure to ovulate. Ovulation can be stimulated by Drugs that prevent the negative feedback effect of oestrogen on FSH during the luteal phase of the menstrual cycle Drugs that mimic the effect of FSH and LH These drugs can sometimes cause super-ovulation resulting in multiple births. They can also be used to collect eggs for IVF treatment. Artificial insemination Involves artificially injecting sperm into the female. Can be used to counter low sperm counts in males, either by collecting and freezing several sperm samples and releasing them together into the female or by using donor sperm from another male. Intra-cytoplasmic sperm injection (ICSI) This involves fertilising an egg by directly injecting the part of the sperm containing the nucleus into it. The resulting embryo is then implanted into the female uterus. This technique can be used where sperm are defective or the sperm count is very low. In vitro fertilisation (IVF). Surgical removal of eggs from ovaries after hormone stimulation. Incubation of zygotes and uterine implantation. Pre-implantation genetic screening to identify genetic disorders and chromosome abnormalities The eggs are mixed with sperm in a culture dish. The fertilised eggs are incubated until they have formed at least eight cells and are then transferred to the uterus for implantation In vitro fertilisation (IVF) Used to overcome infertility as a result of blockage of the oviducts .Fertilisation occurs outside the body and a developing embryo is inserted into the womb. Stages in IVF 1. Female given hormone treatment to stimulate multiple ovulation 2. Eggs removed and mixed with sperm in a culture dish to allow fertilisation 3. Fertilised eggs incubated in the culture dish containing nutrient medium to allow fertilised eggs to divide to at least the 8 cell stage 4. 2 or 3 embryos are transferred to the uterus for implantation 5. Remaining embryos stored frozen in case implantation has to be repeated. Pre-implantation genetic screening and diagnosis Before embryos are transferred to the womb for implantation, a few cells may be tested for genetic abnormalities Pre-implantation genetic screening (PGS) – Non-specific testing for common chromosomal abnormalities and single gene disorders in general Pre-implantation genetic diagnosis (PGD) – Used to check specifically for a particular condition These tests allow a decision to be made on which embryos should and should not be used for implantation. Contraception — physical and chemical methods of contraception. Biological basis of physical methods. Physical methods such as barrier methods, avoiding fertile periods, intra uterine devices and sterilisation procedures. Contraception Intentional prevention of conception or pregnancy. Physical methods of contraception Barrier methods e.g. condoms, Diaphragm – dome shaped rubber cap that is inserted into the vagina to block the cervix before intercourse Cervical cap – rubber structure that fits tightly round the cervix and can be left in place for a few days Intra-uterine devices T shaped plastic structure that is inserted into the uterus. Works by Causes release of white blood cells that attack sperm Prevents sperm reaching the egg Prevents implantation of the embryo Can cause complications like inflammation of the uterus or ectopic pregnancies (where embryo implants at a site other than the uterus) Sterilisation Cutting and tying sperm ducts in males (vasectomy), cutting and tying oviducts in females Chemical contraceptives are based on combinations of synthetic hormones that mimic negative feedback preventing the release of FSH/LH. Some prevent implantation (‘morning-after pills’) or cause thickening of cervical mucus (‘progesterone- only p Chemical methods of contraception Pills containing combinations of synthetic hormones Oral pills contain synthetic progesterone and synthetic oestrogen. Taken daily for 3 weeks following menstruation, the progesterone and oestrogen exert negative feedback control inhibiting release of FSH and LH from the pituitary and so preventing follicle maturation and ovulation. Placebo pills are taken in the fourth week so oestrogen and progesterone levels fall allowing menstruation to occur. Morning after pills Contain higher levels of oestrogen and progesterone than normal oral contraceptive pills and are taken to prevent implantation from occurring. Mini pills Progesterone-only pills that thicken cervical mucus preventing sperm reaching the egg. Antenatal screening. Ultrasound imaging. Anomaly scans may detect serious physical problems. Dating scans, for pregnancy stage and due date, are used with tests for marker chemicals which vary normally during pregnancy Antenatal and postnatal screening Antenatal care During pregnancy, the mother’s blood pressure is monitored, her blood group is identified and blood and urine tests carried out. Ultrasound imaging An ultrasound scanner held to the abdomen of the pregnant woman picks up high frequency sounds that have bounced off the foetus. These are converted to an ultrasound image on a computer screen Dating scan Carried out at 8-14 weeks to determine the stage of pregnancy and calculate the date when the baby is due to be born. Dating scans are used with tests for marker chemicals that vary normally during pregnancy. Timing of tests is important in avoiding false results. The presence of a particular chemical in high concentration may indicate an abnormality at one stage of a pregnancy but have no significance at another stage. Anomaly scan Carried out at 18 – 20 weeks to heck for any serious physical abnormalities in the foetus. Biochemical tests to detect the normal physiological changes during pregnancy Medical conditions can be detected by a range of marker chemicals that indicate a condition but need not necessarily be part of the condition. Biochemical tests Biochemical tests detect normal changes associated with pregnancy, e.g. Human chorionic gonadotrophin (HCG) Presence of this hormone, secreted by the embryo, in the blood and urine is used as a test to confirm early pregnancy But other biochemical tests can indicate medical conditions, e.g. Pre-eclampsia This condition can cause dangerous complications during pregnancy. Some of the symptoms that may be displayed are High blood pressure Excess protein in blood plasma High urea in blood plasma Lower calcium concentration in urine In serious cases, the baby may be induced early to avoid endangering the mother’s life. Alpha-fetoprotein (AFP) This protein is produced by the foetus. Low levels during pregnancy are found in cases of Down’s syndrome and Edward’s syndrome. However this is a screening test (not a diagnostic test) and a low level does not mean the foetus has one of these conditions. Diagnostic testing Amniocentesis and chorionic villus sampling (CVS) and the advantages and disadvantages of their use. Cells from samples can be cultured to obtain sufficient cells to produce a karyotype to diagnose a range of conditions. Diagnostic tests A screening test indicates that a foetus may have a condition but a diagnostic test will show definitely whether the foetus has the condition. It is carried out when Screening tests indicate a potential abnormality There is a family history of genetic disorders The woman’s age puts her in a high risk category (the incidence of Down’s syndrome babies increases in older mothers). Karyotypes A karyotype shows a person’s complete chromosome complement arranged in pairs, e.g. Normal female karyotype Amniocentesis and chorionic villus sampling are diagnostic tests that use karyotypes obtained from the foetus. Amniocentesis Chorionic villus sampling (CVS) Involves taking a sample of cells from the placenta. The sample can be taken through the abdomen (trans-abdominal) or through the female reproductive tract (trans-cervical). The cells are cultured and used to produce a karyotype. Carried out at about 14-16 weeks. Involves withdrawal of a little amniotic fluid containing foetal cells. These are cultured (grown) to get enough cells to produce a karyotype. This takes about 2 weeks. Amniocentesis carries a slightly increased risk of miscarriage. An advantage of this technique is that it can be carried out as early as 8 weeks into the pregnancy when a termination, if chosen, might be less traumatic. CVS has a higher risk of miscarriage than amniocentesis The karyotype obtained may diagnose a condition in the foetus, e.g. Down’s syndrome (three chromosome 21 (trisomy 21) rather than a pair) Rhesus antibody testing. Anti-rhesus antibodies are given to rhesus- negative mothers after a sensitising event or after birth Rhesus antibody testing When a Rhesus-negative mother is pregnant with a Rhesus-positive baby, antigens on the surfaces of the baby’s red blood cells are regarded as “foreign” by the mother’s immune system if it comes into contact with them during the birth process. After the birth, the mother is given anti-Rhesus antibodies to destroy any of the Rhesus antigens left behind, before the mother’s immune system makes its own antibodies against them (making her “sensitised”). If she became sensitised, her immune system would treat any future Rhesus-positive foetuses as “foreign” and attack it. It is therefore important that medical staff test the mother’s blood to establish its type. Postnatal screening. Diagnostic testing for metabolic disorders, including phenylketonuria (PKU), an inborn error of metabolism. Individuals with high levels of phenylalanine are placed on a restricted diet. Postnatal (after birth) diagnostic testing New-born babies are tested for metabolic disorders including phenylketonuria. Phenylketonuria (PKU) The amino acid phenylalanine is converted by an enzyme to a different amino acid, tyrosine. Tyrosine continues along metabolic pathways, for example the one producing the skin pigment melanin. Phenylketonuria results from a mutation in the gene coding for this enzyme. Phenylketonuria is an example of an inborn error of metabolism. Phenylalanine cannot be converted to tyrosine and instead is changed to toxins that affect brain development resulting in severe learning difficulties. New-born babies are screened for PKU using a blood test and if they have the condition are treated using a diet very low in phenylalanine. The use of pedigree charts to analyse patterns of inheritance in genetic screening and counselling. Patterns of inheritance in autosomal recessive, autosomal dominant, incomplete dominance and sex-linked recessive single gene disorders. Draw, analyse and interpret pedigree charts over three generations to follow patterns of inheritance in genetic disorders using standardised human pedigree nomenclature and symbols (sex, matings, siblings, affected individuals, twins, heterozygotes, carrier of sex-linked allele and deceased). Pedigree charts symbols used male Unaffected male Affected male Unaffected female Autosomal recessive pedigree Affected female Carrier female of sex linked gene Deceased twins female mating descent Autosomal refers to a gene carried on an autosome, i.e. a chromosome that is not a sex chromosome. The diagram shows an example of an autosomal pedigree chart If the dominant gene is A and the recessive a, can you give genotypes of: grandfather, grandmother, father, mother, granddaughter, father’s brother? Grandfather (Aa) grandmother (aa) father (Aa) mother (Aa) granddaughter (aa) father’s brother Aa Autosomal dominant pedigree (e.g. Huntington’s chorea The diagram shows an example of an autosomal dominant pedigree chart If the dominant gene is H and the recessive h, can you give genotypes of: grandfather, grandmother, father, mother, granddaughter, father’s brother? Grandfather (Hh) grandmother (hh) father (Hh) mother (hh) granddaughter (Hh) father’s brother (hh) Sex-linked recessive condition, e.g. haemophilia A sex-linked gene is one that occurs on the X chromosome. A male having this gene will always express it in his phenotype even if it is recessive since he only has one X chromosome and therefore only one gene for this characteristic. These genes are represented as a superscript letter on an X, e.g. Xh the gene for haemophilia. The diagram shows an example of a sex-linked pedigree chart, e.g. for haemophilia If the recessive haemophilia gene h, can you give genotypes of: grandfather, grandmother, father, mother, grandson, father’s brother? Grandfather (XY) grandmother (X Xh ) father (XY) mother (X Xh ) grandson (XhY) father’s brother (XhY) Pre-implantation genetic diagnosis (PGD). The use of IVF in conjunction with PGD to identify single gene disorders and chromosomal abnormalities. In vitro fertilisation (IVF) This is a fertility treatment where eggs are collected from the female and fertilised with the male sperm outside the body. Embryos develop from the fertilised eggs and are placed back into the female womb to develop. Pre-implantation diagnosis involves examining cells from the embryo to check for chromosome abnormalities or single gene disorders before it is placed back into the womb. Some people object to this procedure seeing it as a step towards so-called designer babies.