Postmortem Forensic Toxicology
advertisement

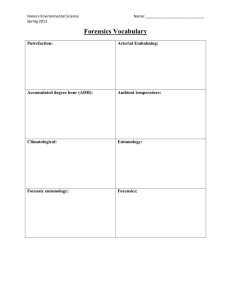
Postmortem Forensic Toxicology Teri Martin teri.martin@jus.gov.on.ca September 23, 2003 Outline • • • • • Definitions and purpose of postmortem tox Samples of forensic interest Handling and storage of samples Pitfalls in postmortem toxicology Interpretation of results Postmortem Forensic Toxicology • Qualitative and quantitative analysis of drugs or poisons in biological specimens collected at autopsy • Interpretation of findings in terms of: • Physiological effect at time of death • Behavioural effect at time of death Quantitative vs. Qualitative • Qualitative analysis – determines the presence or absence of a drug or poison in a submitted sample • Quantitative analysis – determines the amount of drug or poison that is present in the submitted sample Postmortem Forensic Toxicology Types of cases: • Suspected drug intoxication cases • Fire deaths • Homicides • Driver and pilot fatalities • Therapeutic drug monitoring • Sudden infant death (SIDS) Samples of Forensic Interest Issues in Specimen Collection • Selection • Multiple, varied sites of collection • Collection • Appropriate method of collection • Adequate volumes for analysis • Storage and handling Important to ensure analytical results are accurate and interpretations are sound Typical autopsy specimens • • • • • • • Blood Urine Stomach contents Bile Liver Hair Vitreous humor Blood • Antemortem ideal blood sample • Postmortem blood is not truly “blood” • Anatomical site of collection at autopsy should be noted Subclavian • Central sites • Heart Heart • Peripheral sites Iliac • Femoral • Iliac • Subclavian Femoral • Other sites • Head blood • Hematoma blood Hematoma • Extravascular blood clot • Protected from metabolism • Analysis will indicate what drugs were present in the blood at the time of formation Hematoma case example • A 26 year old man was found dead at the bottom of a staircase. Death was due to physical injuries. • Question as to alcohol use prior to fall down stairs • No urine available at autopsy • Alcohol not detected in femoral blood • Alcohol in hematoma blood 150 mg/100 mL • The deceased had been drinking prior to receiving the head trauma. • The deceased had survived for several hours after the injury. Hematoma • Caution: There may be a delay between the incident which resulted in hematoma and the actual formation of the hematoma • Therefore, this alcohol concentration does not necessarily indicate the BAC at the time of the fall down the stairs. Urine • Produced by the kidneys • Blood filtered by the kidneys • Stored in the bladder until voided • Qualitative - the presence of a drug in the urine of an individual indicates that some time prior to death the drug or poison was present in the blood of the individual Stomach contents • Visual examination may reveal tablets • Drugs that have been orally ingested may be detected in stomach contents • Caution: drugs administered by other routes may also diffuse into stomach contents from the blood • Generally qualitative: • Stomach contents are not homogeneous • Only a portion of stomach contents collected (unmixed?) • Useful for directing further analysis Case Example • A 26 year old woman is found dead in bed • Numerous medications in her home: • Amitriptyline, Oxycodone, Morphine, Paroxetine, Diphenhydramine, Pseudoephedrine, Phenobarbital, Codeine, Temazepam, Diazepam • Only 3 mL of blood collected at autopsy • Qualitative analysis of stomach contents: • Amitriptyline: detected • Nortriptyline: detected • Quantitation can now be performed in blood Liver • Drug metabolism occurs in the liver • Both parent compounds and metabolites may be present in higher concentrations in the liver than in the blood ease of detection • Limitation is that drugs are not uniformly distributed throughout the liver confounds interpretation Bile • Digestive secretion • Continuously produced by the liver • Stored in the gallbladder • Qualitative - the presence of a drug in the bile of an individual indicates that sometime prior to death, the individual was exposed to the drug Vitreous humor • Fluid that occupies the space between the lens and the retina of the eye. • Sequestered from putrefaction, charring and trauma, microorganisms. • Useful in cases where decomposition is advanced, body is exhumed or in fire deaths • Limitation is blood:vitreous ratio may not be known Hair • Recent specimen of interest • Metabolism does not occur in hair • Can provide a historical record of drug or poison exposure • Pros and cons of hair analysis still being uncovered racial variability? Case Example Poklis, A. 2002. Abstract SOFT, Dearborn, Michigan. • • • • • • 30 year old woman, previously in good health Nausea, vomiting, diarrhea, rash, fever Weakness in hands and feet Guillian Barre? Hospitalized with hypotension, seizures Misplaced laboratory result Arsenic! Sequential hair analysis for arsenic showed chronic arsenic poisoning over 8 month period Non-biological submissions • Used to direct analysis of biologicals • May indicate the nature of substances that may have been ingested, inhaled or injected • Examples: • Containers found at the scene • Syringes • Unidentified tablets or liquids Autopsy specimens of limited value • • • • • Pleural fluid Chest cavity blood Gutter blood Samples taken after embalming Samples taken after transfusion in hospital • “Spleen squeezings” • “Esophageal scrapings” Chest Cavity Fluid • Not readily definable • Most likely to be collected if: • Traumatic injury to the chest • Advanced decomposition • A “contaminated” blood sample, chest cavity fluid may contain fluids from stomach, heart, lungs etc. Samples taken after embalming • Methanol is a typical component of embalming fluid • Most drugs are soluble in methanol • Embalming process will essentially “wash” the vasculature and tissues • Qualitative analysis can be performed on body tissues Case Example A 72 year old woman, given meperidine to control pain following surgery, later died in hospital. The woman was in poor health and it is possible that death was due to natural causes. However, coroner requests toxicology to rule out inappropriate meperidine levels. BUT: • Body had been embalmed • Liver and spleen submitted Storage and Handling Proper specimen handling • Identification of samples • Continuity • Contents • Specimens delivered to lab without delay • Specimens should be analyzed as soon as possible • Storage areas should be secure Storage and Handling • • • • • Not feasible to analyze specimens immediately Sample should be in well-sealed container Sample containers must be sterile Use of preservatives and anti-coagulants Refrigeration vs. Freezing • Both inhibit bacterial action; esp. freezing • Freezing results in prep time • Freeze-thaw cycle may promote breakdown Storage of Samples • Preservative • Sodium fluoride • Anti-coagulants • • • • • Sodium citrate Potassium oxalate EDTA Heparin Not imperative for postmortem blood samples Determining analyses • Case history • Medical history • Autopsy findings • Symptomatology • • • • Experience of the toxicologist Amount of specimen available Nature of specimens available Policies of the organization Pitfalls in Postmortem Forensic Toxicology Decomposition • Autolysis • The breakdown of cellular material by enzymes • Putrefaction • A septic/infectious process • The destruction of soft tissues by the action of bacteria and enzymes • Traumatic deaths may demonstrate putrefaction Decomposition • Fewer samples available for collection • Quality of samples is diminished • Putrefaction produces alcohols • • • • Ethanol Isopropanol Acetaldehyde n-propanol Postmortem redistribution • A phenomenon whereby increased concentrations of some drugs are observed in postmortem samples and/or site dependent differences in drug concentrations may be observed • Typically central blood samples are more prone to postmortem changes (will have greater drug concentrations than peripheral blood samples) Possible mechanisms of postmortem redistribution • Diffusion from specific tissue sites of higher concentration (e.g. liver, myocardium, lung) to central vessels in close proximity • Diffusion of unabsorbed drug in the stomach to the heart and inferior vena cava • Diffusion of drugs from the trachea, associated with agonal aspiration of vomitus Case Example • 37 year old man found dead in his home • Cause of death identified at autopsy as asphyxia due to choking; white pasty material lodged in throat • Heart blood • Morphine: 20 000 ng/mL • Amitriptyline: 0.36 mg/dL • Femoral blood • Morphine: 442 ng/mL • Amitriptyline: 0.01 mg/dL • Examination of esophageal and tracheal contents revealed presence of both morphine and amitriptyline Susceptible Drugs Drugs most commonly associated with postmortem redistribution: 1. are chemically basic 2. have large volumes of distribution Volume of distribution • Review from last lecture: • Volume of distribution is the amount of drug in the whole body (compared to the amount of drug in the blood) • If a drug has a large volume of distribution, it is stored in other fluids and tissues in the body Susceptible Drugs • Tricyclic antidepressants • • • • Amitriptyline Nortriptyline Imipramine Desipramine • Antihistamines • Diphenhydramine • Narcotic Analgesics • Codeine • Oxycodone • Propoxyphene • Doxepin • Digoxin Example: Digoxin p. 60, Principles of Forensic Toxicology • A 33 year old white female is admitted to hospital after taking 60 digoxin tablets • An antemortem blood sample collected 1 hour prior to her death indicates a blood digoxin level of 18 ng/mL • Heart blood digoxin concentration obtained at autopsy is 36 ng/mL Example: Digoxin • Postmortem increase in blood digoxin concentrations is suspected to be due to the release of the drug from the myocardium • Postmortem levels > Antemortem levels • Heart blood levels > Femoral blood levels Postmortem redistribution • Coping with the problem of postmortem redistribution: • Analysis of both central blood and peripheral blood in cases where postmortem redistribution may be a factor • Compilation of tables to determine average and range of postmortem redistribution factors for drugs Incomplete Distribution • Site dependent differences in drug levels due to differential distribution of drugs at death • Has been noted in rapid iv drug deaths • Example: • Intravenous injection of morphine between the toes • Fatal amount of drug reaches the brain • Full distribution of the morphine throughout the body has not occurred • Femoral concentration > Heart concentration Drug Stability • Knowledge of a drug’s stability is necessary to facilitate interpretation of concentrations • Breakdown of drugs may occur after death and during storage via non-enzymatic mechanisms • Cocaine Benzoylecgonine (Hydrolysis) • LSD degradation due to light sensitivity • Others ? Example: Bupropion • Bupropion, an antidepressant, was identified and confirmed during a GC drug screen • Blood analyzed using a quantitative analysis: • Bupropion not detected • Review of the literature: • Laizure and DeVane, 1985. Ther. Drug. Monit. • “Bupropion showed a log linear degradation that was both temperature and pH dependent…” Evaporation of volatiles • • • • • Ethanol Carbon monoxide Cyanide Toluene Other alcohols Example: Carbon Monoxide Ocak et al. 1985. J. Analytical Toxicology. 9: 202-206 • Effects of storage conditions on stability of CO • No significant change in % CO saturation in capped samples stored at room temperature or 4oC • Significant losses in % CO saturation in uncapped samples stored at room temperature and at 4oC • Mechanism for loss diffusion Interpretation Interpretation Therapeutic, toxic or fatal? How do you know? • Compare measured blood concentrations with concentrations reported in the literature: • Clinical pharmacology studies • Incidental drug findings • Plasma blood • Consider case history: • Symptoms observed by witnesses? • Tolerance of the individual to the drug Blood:plasma ratios • Knowledge of the blood:plasma ratio can be very important when applying information from clinical studies to postmortem forensic tox • • • • Cocaine, blood:plasma ratio is 1.0 Phenytoin, blood:plasma ratio is 0.4 Ketamine, blood:plasma ratio is 1.7 Hydroxychloroquine, blood:plasma ratio is 7.2 Example: THC • Six healthy male volunteers recruited for a study of the pharmacokinetics of THC in humans • Smoked a “high-dose” THC cigarette • 15 minutes after cessation of smoking, plasma THC concentrations averaged 94.8 ng/mL • The plasma:blood ratio for THC is 1.8 • Plasma contains 1.8x as much THC as whole blood • The results of this study correspond to a blood THC concentration averaging 53 ng/mL Importance of History: Tolerance • Drug concentrations in non-drug related deaths may overlap with reported drug concentrations in fatal drug intoxications • Methadone example: • Naïve users - deaths due to methadone are associated with blood levels > 0.02 mg/100 mL • Patients on methadone maintenance – peak blood concentrations may range up to 0.09 mg/100 mL Interpretation Acute vs. Chronic Ingestion: Can you tell? • Parent:metabolite drug concentration ratio may be of assistance in differentiating between acute and chronic ingestion of a drug Example: Amitriptyline Case 1 Amitriptyline: 0.4 mg% Nortriptyline: 0.02 mg% Parent >> Metabolite Suggestive of acute overdose and rapid death Case 2 Amitriptyline: 0.04 mg% Nortriptyline: 0.08 mg% Parent < Metabolite Slow death and/or chronic administration Interpretation Metabolites are produced when drugs are biotransformed (converted) into other chemicals, more easily excreted from the body Metabolite drug concentrations may be the more useful measure of exposure or toxicity Metabolites: Exposure The parent compound may be a prodrug or may have a shorter t1/2 than the metabolite: • Clorazepate nordiazepam • Flurazepam N-desalkylflurazepam • Heroin morphine Metabolites: Toxicity The metabolite may have toxicity over the parent compound: • Acetaminophen N-Acetylbenzoquinoneimine • Meperidine normeperidine • Methanol formic acid • Ethylene glycol oxalic acid calcium oxalate

![On Mapping Public Rhetoric [powerpoint]](http://s3.studylib.net/store/data/009200433_1-48e72679ada1cc1e8817e00918caa980-300x300.png)