Indicator Microorganisms
advertisement

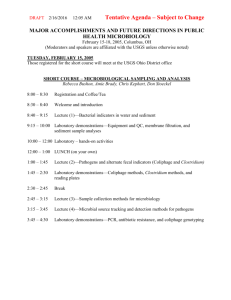
Lecture 2 Microbial Indicators of Fecal and Other Types of Environmental Contamination ENVR 421 Mark D. Sobsey Microbial Indicator Concepts and Purposes • Many diverse types of pathogens can contaminate water, food, air and other environmental media; many different ones. • Measuring all of these pathogens routinely for determining presence or absence or acceptable concentration is not possible. – Methods are not available to recover and measure some, – Methods are available for others; they are technically demanding, some are slow to produce results and their costs are high. • Alternative approach: measure something other than a pathogen that is indicative of contamination, predicts pathogen presence and estimates human health risks. What is Measured as Microbial Indicators and Why? • Microbial indicators have been used for >100 years (since late 1800s) to detect and quantify fecal contamination in water, food and other samples – Concerns were for bacteria causing water-and foodborne illness, such as: • Salmonella typhi: causes typhoid or enteric fever • Vibrio cholerae: causes cholera • Shigella dysenteriae and other Shigella species: dysentery • Focus was and still is on detecting primarily human (or maybe animal) fecal contamination as source of these and other enteric bacterial pathogens • Detect fecal contamination by measuring: – common enteric bacteria residing in the gut and shed fecally – Chemicals associated with the gut or with anthropogenic fecal contamination – Something else associated with and predictive of fecal contamination What is Measured as Microbial Indicators and Why? • Microbial indicators are used to indicate other conditions, unrelated to fecal contamination, such as : – Food spoilage bacteria and molds – Excessive microbial growth in water and biofilms that cause appearance, taste and odor problems: – “red water” from iron biofouling – blooms of algae and cyanobacteria (blue-green algae) » Some of the organisms harbor or release toxins (harmful algal blooms or “red tides”) • Excessive bacterial release from biological filters used in water treatment What is Measured as Microbial Indicators and Why? • Airborne contamination: – From wet buildings: molds and actinomycetes – From industrial processes: • bacterial endotoxins from cotton dust, solid waste and other sources • Microbial allergens from manufacturing processes (aerosols and dusts) – total airborne microbe concentrations • In health care facilities • In “clean room” manufacturing environments for electronics and pharmaceuticals • From composting operations – Salivary bacteria from dentistry activities Fecal Microbial Indicators: Background and Rationale Besides nutrients and organic matter, human and animal fecal wastes contain large numbers of microbes (~100 billion/gram). Constitute ~1/3rd the mass of human fecal matter Most are beneficial or essential in the gut; not pathogens Some gut microbes are human pathogens; they cause disease. – Human pathogens can be shed in human and animal feces. – Humans and animals harbor pathogens some of the time; infection – Enteric pathogens are transmitted by the fecal-oral route; often 106-109 pathogens/gram of feces of an infected person – Ingested with fecally contaminated water, food, objects, or by direct and indirect personal contact. Limitations in Detecting Enteric (Fecal) Pathogens and their Indicators • Some enteric pathogens have environmental origins besides feces; environmental reservoirs • Some microbial indicators of fecal contamination have both fecal and non-fecal environmental sources • Some fecal indicator microbe tests also detect similar non-fecal microbes; tests are not perfect in detecting microbes of fecal origin Pathogen Detection and Monitoring • Pathogen detection – technically demanding, – often tedious, – slow to produce results, – Often unreliable – expensive. • Done routinely in the health care field (clinical diagnostic microbiology): – often essential to patient treatment and care – provides national surveillance of infectious disease epidemiology Pathogen Analysis, Monitoring and Surveillance • Until recently, rarely done for managing food quality – Salmonella and E. coli O157:H7 are now monitored in meat and poultry; Listeria monocytogenes monitoring also being done • Sometimes done for monitoring or managing water quality – pathogen occurrence surveys and special studies: • survey (18 months) for Giardia, Cryptosporidium and enteric viruses in larger drinking water supplies using surface water sources: ICR (Information Collection Regulation) • enteric virus survey in ground water sources of drinking water – Data base for Ground Water Disinfection Rule – investigation of waterborne outbreaks – Technology verification/performance evaluation • Pilot/in-plant studies – Pathogen monitoring sometimes done for biosolids (Class A) • Salmonella, viable Ascaris ova, culturable enteric viruses Microbial Indicators of Fecal Contamination Traditional approach to protect/assess the "sanitary" quality of water (food) with respect to fecal contamination. Quantify bacteria commonly present in intestines of warm blooded animals high numbers easy to measure surrogates for pathogens Developed when bacterial pathogens were recognized in late 1800s and early 1900s Salmonella, Shigella, V. cholerae, etc. Criteria for Reliable Indicators of Fecal Contamination Applicable to all types of water (and other relevant samples). Present in feces, sewage and fecally contaminated samples when pathogens are present; numbers correlate with amount of fecal contamination; outnumber pathogens No "aftergrowth" or "regrowth" in the environment Survive/persist > than or = to pathogens. Easily detected/quantified by simple lab tests in a short time. Constant characteristics Harmless to humans and other animals Numbers in water (food, etc.) are associated with risks of enteric illness in consumers (dose-response relationship) Dose-Response Relationship Between Indicator Density in Vehicle (Water) and Risk of Illness in Exposed Individual or Population: Hypothetical Example Illness Risks Indicator Concentration Systems and Technologies for Microbial Indicator Monitoring • Static laboratories – Lab infrastructure, expensive equipment, consumable supplies and trained staff, QA/QC – Potentially long chain to get samples from field to lab – Routine in developed world but rare in developing world • Field labs / portable labs – Simpler and cheaper • Integrated systems – Colilert system, DelAgua and Millipore test kits – Still need knowledgeable and trained staff; relatively expensive • Disposable tests – Petrifilm, Presence/absence test for H2S-producing bacteria – Still relatively expensive (>$1); minimal training needed Desirable Properties of Diagnostic Tests for Developing World • • • • • • • Affordable by those at risk Sensitive (low false-negatives) Specific (few false positives) User-friendly (simple to perform) Rapid and robust; easy to store Equipment-free (ideally no electricity) Delivered to those who need it (Urdea et al ‘Requirements for high impact diagnostics in the developing world’ Nature S1, 73-79 (23 Nov 06) Current Options for Fecal Bacteria Testing by Culture Methods • Liquid quantal (MPN and P-A) assays: – Defined substrate technology (e.e. Colilert – Other chromogenic/fluorogenic broths – Less specific broths followed by biochemical confirmation (e.g., urease test) • Membrane filter methods – Chromogenic/fluorogenic media • Pour and spread plates – e.g., pectin gel media:Coliscan Easygel • PetriFilm and other films; as culture plates Current Bacterial indicators of Fecal Contamination Total coliforms: • drinking, bathing and shellfish water standards • not feces-specific (environmental sources). Fecal ("thermotolerant") coliforms (FC): • detect by growing at elevated temperature of 44-45oC • ditto total coliforms, but less so E. coli: the "fecal" coliform • Detect and distinguish from other total and fecal coliforms by Betaglucuronidase activity • may occur naturally in tropical environments (and possibly elsewhere) Fecal streptococci (FS): • Mostly Lancefield group D (and some group Q) streptococci and enterococci • not feces-specific. Enterococci: • More feces-specific sub-set of FS: Enterococcus faecalis & E. faecium • EPA guideline for bathing water quality Relationships among Total and Fecal Coliforms and E. coli Total Coliforms Fecal Coliforms Escherichia coli • All total and fecal coliforms and E. coli possess Beta-galactosidase; they can hydrolyze and and ferment lactose • E. coli also possesses Betaglucuronidase and hydrolyzes glucuronide substrates Some Other Bacterial Indicators of Fecal Contamination Clostridium perfringens: – – – – spore-forming anaerobe feces-specific? very (too?) resistant spores (can persist for decades of centuries!) may be an indicator for protozoan cysts Bacteroides spp. and Bifidobacteria spp.: – – – – – most plentiful in feces (100X more than FC, FS and E. coli) strict anaerobes poor survival in the presence of air (oxygen) poor detection methods: requires strict anaerobic conditions Some Bacteroides species may be human-specific Rhodococcus coprophilus: – plentiful in feces of some animals – possible animal fecal contamination indicator BACTERIA ARE NOT ALWAYS GOOD INDICATORS OF VIRUSES AND PROTOZOANS ! Methods to Detect Bacterial Indicators: Quantal Methods • Inoculate multiple sample volumes usually into broth culture medium, incubate and score each volume as positive or negative for indicator growth – Positive cultures in differential/selective medium or based on characteristic appearance • Results for numbers of positive and negative cultures are used to estimate bacterial density – Usually based on a maximum likelihood estimate – Expressed as a Most Probable Number or MPN Methods to Detect Bacterial Indicators: Enumerative Methods • Agar media methods – Inoculate sample onto/into differential/selective agar medium – Pour, spread or spot plate methods • Membrane filter methods – Filter a sample volume through a membrane filter that retain bacteria and place membrane on a differential/selective medium • Incubate • Count numbers of characteristic bacterial colonies on/in agar plates or on membrane filters and compute colony forming units (CFU) per unit volume CANDIDATE VIRAL INDICATORS OF FECAL CONTAMINATION OF WATER Coliphages: viruses (bacteriophages) infecting E. coli and perhaps other coliforms; attach directly to cell wall (somatic) heterogeneous group; may not be feces-specific; hostdependent detection Male-specific (F+) coliphages: coliphages infecting "male" strains of E. coli (posses pili); may be feces-specific May distinguish human from animal fecal contamination by group classification (II & III human; I & IV animal); but, pigs may harbor groups II & III, too Bacteroides fragilis phages: may be human feces specific; USA studies do not show human-specificity; concentrations too low Salmonella phages: in human and animal feces; may indicate presence of Salmonella bacteria; concentrations too low Male-specific and Somatic Coliphage Hosts and Phages Male-specific host E. coli Famp F+ Somatic host E. coli C F+ Coliphage Somatic Coliphage Methods to Detect Coliphages in Water • Direct Plating Methods: water + host + medium – Enumerative: Double or Single Agar Layer : 0.1-1 ml (DAL) or 10-100 ml SAL • “pour plate” or plaque assay for development of phage “plaques” – Quantal: Enrichment culture: 100-1,000 ml; confirm by lysis of host on “lawn”. • Filter Adsorption-Elution Methods: – filter 100-1000s of mls through electropositive filter • (or add divalent cations and filter through cellulose membrane) – elute adsorbed phages – plaque assay or other assay on host bacteria by other methods • Direct Membrane Filter Method: – add divalent cation to water; filter through cellulose ester membrane – place membrane face down on agar medium-host lawn – incubate, and count plaques. Single Agar Layer Plaque Assay Combine: Sample + Host + Molten Agar Mix Pour in plate Incubate Count plaques Indicators of Protozoan Parasites • Currently, there is no universally reliable indicator of enteric protozoan parasites • Candidate indicators are bacterial spores: – Spores of Clostridium perfringens (a gut anaerobe); fecal indicator; also used as enteric virus indicator; indicator of occurrence, survival and treatment – Aerobic endospores (primarily spores of Bacillus species); ubiquitous environmental indicators of water treatment efficacy for Giardia, Cryptosporidium – Microalgae: candidate water treatment indicators; some are the same size and shape as protozoan pathogens; some also have similar surface properties Microbial Source Indicators: Microbial Source Tracking Indicators and Methods • Standard indicators and methods are unable to identify specific fecal sources impacting water and other environmental media; need advanced methods • Phenotypic: antimicrobial resistance patterns, sourcespecific microbes (Rhodococcus coprophilus for animals vs. Bacteroides/Prevotella species like fragilis, thetaiotaomicron, etc. for humans, fecal sterols, etc. • Molecular methods: human vs. animal F+ RNA coliphages, Bacteroides/Prevotella species (16S rRNA), multilocus PCR and nucleotide sequencing of specific bacteria, virus or parasite genes or loci, ribotyping, pulse field gel electrophoresis, etc.