Document
advertisement

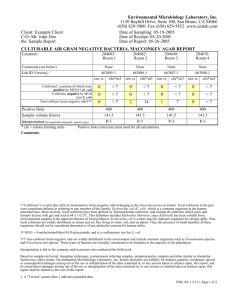
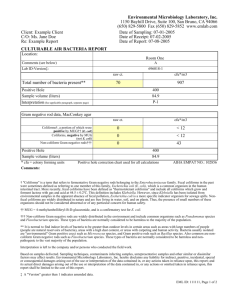
Microbiological Quality of Water Microbial Indicators of Fecal Contamination • Approach used to evaluate the quality of water for human use • Quantification of bacteria normally found within the intestines of warm blooded animals • High numbers is an indication of the presence of pathogens Criteria for an Ideal Indicator of Fecal Contamination • Applicable to all water sources • Present in stools, sewage water, and water samples that contain pathogens Criteria for an Ideal Indicator of Fecal Contamination • Number correlated to level of fecal contamination and to number of pathogens • No growth in the environment • Survival/persistence that is longer than that of pathogens • Easily detected and quantified • Numbers associated to the risk of consumers of contracting enteric diseases Ideal Indicator • Ex: Mooney’s Bay water quality warnings based on E.coli levels • Representative of ALL potential sources • To date no single indicator meets all the criteria Indicators of Fecal Contamination • Coliform bacteria : – Bacteria of the Enterobacteriaceae family – Includes 4 genera • Enterobacter, Klebsiella, Citrobacter, and Escherichia – Present in the intestine of most warm blooded animals (humans) – Gram negative rods, non-sporulating • Ferment lactose with acid and gas production in 48 hours at 37°C Fecal Coliforms • Subset of total coliforms • Escherichia coli (E. coli) • Thermotolerant coliforms • Grow and ferment lactose at 44oC • Source: Fecal material only – Exception the tropics Fecal Streptococci • Gram positive • Mainly associated with animal intestines – S.faecalis, S.faecium • Longer survival time than coliforms • Survive broad range of environmental conditions ex: temperature, pH, salt • The ratio between coliforms and Streptococci is used to confirm a contamination from human sources – Ratio Escherichia/Streptococci greater than 0.7 Tests for Fecal Contamination • Selective media – Allows the growth of certain genera • Differential media – Allows the visual discrimination of different genera Methods • Presumptive tests – MPN • Viable counts Presumptive Tests • Makes use of differential/selective media to detect characteristics common to indicator microorganisms – Positive test= presence suspected – Negative test = absence • Most probable number (MPN) – Probable number based on a statistical point of view Lactose Broth A B C A. Negative test; No acid or gas B. Negative test; Acid no gas C. Positive test; Acid + gas Gas • Presumptive test for total coliforms – Differential medium • Allows to detect lactose fermentation • pH and gas indicators Presumptive Test for S. faecalis (Enterococcus) • Selective medium – Contains azide – Selective for Enterococcus A B • Differential – Fermentation of glucose A. Negative; no acid B. Positive; presence of acid Food Microbiology Concerns • Provide clean, healthy, and safe foods to consumers • Prevent and retard spoiling • Prevent food associated diseases • Preservation and production of foods – 1/3 of all foods are lost because of spoilage Sources of Bacteria in Foods Sources of Bacteria in Foods • Soil and water • Plants • Equipment for the treatment and manipulation of food products • Humans and Animals (Natural flora) • Compost (fertilizer) • Air/dust Spoilage • Considerations: – Organoleptic properties • Taste • Smell • Texture • Appearance Bacteria Associated with Food Spoilage • Meats – Enteric bacteria • Escherichia coli • Salmonella • Milk products – Lactic bacteria Gram (-), short rods, facultative anaerobes Gram (+), short rods, non-spore forming • Lactobacillus • Fruits and vegetables – Pseudomonas Gram (-), short rods, strict aerobes Types of Food Borne Diseases • Food infections – – – – – Usually associated with endotoxins Requires ingestion of pathogen Requires growth of pathogen in host Appearance of symptoms between 24-72 hours Often aggravated by the use of antibiotics • Bacteriolytic antibiotics are not recommended • Bacteriostatic antibiotics can help Types of Food Borne Diseases (Cont’d) • Food intoxications – – – – – Usually associated with exotoxins No infection Appearance of symptoms between 1-3 hours Antibiotherapy useless in the absence of infection Use of anti-toxins recommended Bacteria Associated with Food Infections • E. coli O157:H7 – Mostly associated with meats from beef and pork – Normal inhabitant of the natural flora of the intestine • Absent in muscles • Contamination is usually the result of inappropriate manipulations – Utensils – Opening and spilling of intestines – Skin of employees – Endotoxin A (lipid A of LPS layer) E. coli O157:H7 (Cont’d) • Can be associated with fresh vegetables • Can be associated to products said to be “organic ” – Contamination by animal and human compost • Can be associated with water ex: Walkerton, ON Salmonella sp. • Mainly associated with the intestines of poultry and pork • Can also be found on fresh vegetables just like E.coli • Very low infectious dose – < 10 cells Bacteria Associated with Food Borne Intoxications • Clostridium perfringens – Gram Positive rods – Spore former sometimes used as indicator – Natural constituent of the natural flora of mammals (including humans) and birds – Also found in soil and water – Intoxications associated with foods prepared a few days in advance – Intoxication caused by an enterotoxin • Stomach aches and diarrhea Bacteria Associated with Food Borne Intoxications • Clostridium Botulinum – Gram Positive rods – Spore former found in soil and water – Intoxications associated with poorly sterilized cans of fruits and vegetables – Also associated with food prepared a few days earlier – Intoxication caused by a neurotoxin • Flaccid paralysis, double vision, speech impediment, difficulty to swallow • Death due to paralysis of respiratory system