Vitek 2
advertisement
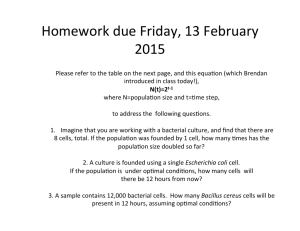
BSAC Standardized Disc Susceptibility Testing Method - User Group Meeting. Cardiff, 13 May 2010 Vitek 2 – A User Experience. Nathan Reading Senior Biomedical Scientist Sandwell and West Birmingham Hospitals NHS Trust 1 Year B.V. (before Vitek....) • Previously.... – Disc susceptibilities for >90% isolates • • • • • Urines Blood Cultures (Direct and Repeats) Respiratory Ocular General – swabs etc – Agar Dilution MIC’s • All Pseudomonads • Resistant gram negatives • Ad-hoc organism/difficult infections – Gradient Tests • Difficult organisms • Adhoc testing/confirmations 1 Year B.V. (before Vitek....) Staffing required.. 1 Senior BMS W.T.E. 2x BMS W.T.E. 0.5 MLA W.T.E. Daily/Weekly Tasks Reading Plates/Setting Up Disc Susceptibility Plates and pouring Agar Dilution Plates/Preparing Antibiotic Stocks and Dilutions/Setting up MIC plates/Reading MIC Plates. Working Day 8am-5pm Weekday 8am-12pm Saturdays (All sensitivities bar MIC’s read, all sensitivities put up bar urinary isolates) 8am-1pm Sundays (Only Blood Culture and MRSA sensitivities setup/read) Sensitivity testing 1 Year AV (after Vitek...) • 1 x Senior BMS WTE • 1x BMS WTE • 0.6 xMLA WTE – Reduced staff overhead – Senior BMS freed to look after our organism collection • All sensitivity testing complete >90% time by 4pm • Sensitivity testing ready for release to clinician by 10-11am • We do not release same day sensitivity testing.... – Do not wish to retract incorrect reports – Our working days structure currently means that cards not going onto Vitek until mid morning earliest Sensitivity testing 1 Year AV • Gram negatives – UTI • Use Chromogenic Media • E.coli – treated as E.coli, Vitek Sens • Coliform group – Vitek Sens and Automated ID also – Systemic -Fermenters • Automated ID and Sensitivity Test – Non fermenters • Automated ID or Basic Manual ID • Automated Sensitivity Test Blood Cultures – Direct disc susceptibility – in-house dilution protocol • Repeats by Vitek Sensitivity testing 1 Year AV • Gram positives – Staphylococci • Vitek Sensitivity • Manual ‘traditional’ ID • API/Vitek GP Card for discrepant organisms – Enterococci • Vitek Sensitivity • Antibiogram/API/Vitek GP card if speciation needed – Beta Haem Streptococci • Vitek (Group B) and Discs (All others) • Fastidious Organisms – Discs! Issues - Flexability Card ‘make up’ will never perfect for every user – Bespoke cards can be made for individuals For our UTI’s No Amikacin on UTI card – only Gent We now disc test Amikacin on Gent I/R Aminoglycoside rules cant work properly No Mecillinam Our clinicians want Mecillinam on all Trim R isolates of E.coli/Kleb/Proteus can be 30% isolates! Issues – Antibiotic Concentrations • Rifampicin – Card tests at 0.25,0.5 and 2mg/L – Calling range 0.25-4mg/L – EUCAST/BSAC ‘S’ cut off = 0.06mg/L ‘I‘= 0.12-0.5 ‘R’ =>0.5 – Card does not test low enough to determine S using BSAC/EUCAST breakpoints • Recent card revision did not solve this • Now need to disc test on ad-hoc basis if clinicians require result Issues – Antibiotic Concentrations • Mupirocin – Card tests 1mg/L • Calling range 2-8mg/L! BSAC ranges S= ≤4 I= 8-256 R >256 – Need to disc test to differentiate I from R • Mupirocin decolonisation may still work if Intermediate • Recent revision to cards did not solve this..... Detection of resistance • Detection of Hyperproduction of K1 enzyme in Kleb oxytoca – No Aztreonam on UTI Card AST N144 – Need to rely on Inhibitor Resistance and Cefotaxime which can be variable – Offline Synergy Test • Cefpodoxime/Cefpodoxime+Clav/Cefpodoxime+Clav+Boronic Acid • Aztreonam disc testing Detection of resistance • Detection of AmpC Detection of AmpC • Cefoxitin Resistant • 3rd Gen Ceph’s = S • Check ID – Some Chromogenic agars mis-identify Citrobacter species (may have natural AmpC) • Check ESBL/Confirmation Test – Cefpodoxime/Cefpodoxime+Clav/Cefpodoxime+Clav+Boronic Acid – If negative synergy – probable impermeability/porin loss – If positive synergy with Boronic Acid/Clav/Cefpodozime = AmpC Detection of Resistance • Detection of ESBL • Compared 296 urinary isolates screened with HMRZ -86 a chromogenic 3rd gen Cephalosporin – Vitek missed 11 ESBL producers out of a total of 42 – Situation improved a little on software update • ?algorithms changed • Still misses some low expression of ESBL Solution ? • All of the missed isolates (ESBL&AmpC) reduced zone to Cefpodoxime 10ug disc • ?Need a Vitek card containing Cefpodoxime • 18 missed isolates E.coli/Klebsiella • 10 ESBL Missed with routine card • 7 AmpC Missed with routine card • 1 K1 K oxytoca (included for interest) Solution ? Cefpod Ceftaz Ceftriax AES Findings Escherichia coli 17 ESBL acquired penicillinase >8 ≤1 ≤1 ESBL Escherichia coli 10 AMP C acquired penicillinase >8 ≤1 ≤1 Inconsistent Escherichia coli 14 ESBL acquired penicillinase 2 ≤1 ≤1 Acquired Penicillinase Escherichia coli 15 ESBL acquired penicillinase 0.5 ≤1 ≤1 Acquired Penicillinase ≤1 ≤1 Acquired Penicillinase Isolate ID CPD Routine Zone/ Method mm Findings AES Findings ACQ Penicillinase + Impermeability (Cephamycins), <0.25 Impermeability (Cephamycins) Klebsiella pneumoniae 14 AMP C Escherichia coli 11 amp c acquired penicillinase >8 ≤1 ≤1 Inconsistent Klebsiella oxytoca 18 ?K1 hyper high level natural penicillinase 2 ≤1 <1 ESBL (ctx-m), high level natural penicillinase Escherichia coli 21 amp c ACQ Penicillinase 2 ≤1 ≤1 Acquired Penicillinase Escherichia coli 13 ampc Acq Penicillinase >8 ≤1 ≤1 Inconsistent Escherichia coli 18 esbl Acq Penicillinase 4 ≤1 ≤1 Acquired Penicillinase Escherichia coli 18 AMP C Acq Penicillinase 2 ≤1 ≤1 Acquired Penicillinase Escherichia coli 12 AMP C Acq Penicillinase >8 ≤1 ≤1 Inconsistent Escherichia coli 15 ESBL Acq Penicillinase >8 ≤1 ≤1 ESBL Escherichia coli 14 ESBL Acq penicillinase 2 ≤1 ≤1 Acquired Penicillinase Escherichia coli 14 ESBL Acq penicillinase 4 ≤1 ≤1 Acquired Penicillinase Escherichia coli 14 ESBL Acq penicillinase 2 ≤1 ≤1 Acquired Penicillinase Escherichia coli 17 ESBL Acq penicillinase 2 ≤1 ≤1 Acquired Penicillinase Escherichia coli 16 ESBL Acq penicillinase 2 ≤1 ≤1 Acquired Penicillinase • *BSAC Cefpodoxime ‘S’ cut off 1mg/L Solution ? • 16/18 isolates all had MIC for Cefpodoxime >1mg/L (BSAC breakpoint) • Include Cefpodoxime on card? – With or without CAZ,CTX? Detection of Resistance • What is this isolate? • System highlights MRSA as possible mechanism – changes Cefoxitin result from Negative to POSITIVE Solution ? • All isolates showing this change – PBP 2’ Latex (Oxoid/Mast) • 20 minute test – If +ve therefore MRSA – If –ve need to rule out MRSA still. • Cefoxitin 10 disc on IsoSensitest • MecA PCR • Our own mini study – partially complete – 20 isolates Oxacillin ‘R’ / Cefox Screen Changed to +ve – 10 strains MecA negative (Internal control Nuc +ve = S.aureus) – All 10 PBP 2’ Latex Negative Difficult isolates • Mucoid isolates – esp Pseudomonads – Difficult to get a smooth inoculum – May give false resistance/susceptibility – Need a plan B • MIC? • Gradient Test? • Discs? More areas to investigate? 14 Vitek 2 Implentaton 12 Percentage 10 8 6 4 2 0 PERCENTAGES %I-Gent PERCENTAGES %R-Gent Software upgrade New Cards Gentamicin and E.coli %I and %R Jan 08-Current New and Emerging Phenotypes • July 2009 • Our first Isolate of NDM-1 Carbapenemase in Klebsiella pneumoniae – Detected by Vitek 2 • Subsequent challenge with further strains from other centres also detected as expected • Isolates with VIM,IMP and KPC isolates also detected. • Carbapenemases, the new ESBL? Summary • Automated systems not panacea for solving lack of AST knowledge within laboratory. – Some users may find more questions than answers • BSAC method still required to fill in the gaps – Not just fastidious organisms • Some areas could be optimised to enhance detection of important isolates • Some cards need to be improved for UK/EUCAST breakpoints Summary – the positives • Reduction of staff overhead • Improved speed of results – We at City dont make best use of all benefits of automation • Can be used to upskill knowledge of AST and mechanisms of resistance • Simple to use and well supported by the company.