Development of Therapeutics for Haemophilia A
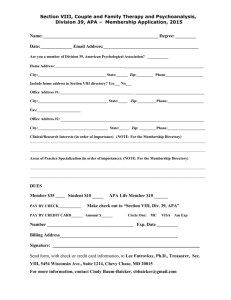
advertisement

Therapeutics for Hemophilia A – Where we are, how we got there and where I think we are going* Roger L. Lundblad, Ph.D. Consultant in Biotechnology Chapel Hill, North Carolina http://www.lundbladbiotech.com And Adjunct Professor, Department of Pathology, University of North Carolina, Chapel Hill, North Carolina Hemophilia in 1960-1970 • University of North Carolina Experience – 53 hemophilia A patients with 91 bleeding episodes; 13.3 units plasma/episode – Roberts, H.R., Graham, J.B., Webster, W.P., and Penick, G.D., Plasma transfusion therapy in hemophlila, in The Hemophilias, ed. K.M.Brinkhous, University of North Carolina, Chapel Hill, NC, USA, 1964 • Therapeutics Costs – 10 to 20 cents a unit – Green, D., Therapeutic materials, in Hemophilia, ed. D.Green, C.C. Thomas, Springfield, IL, USA,. 1972 Hemophilia A – A Statement of the Problem -2012 • • • • • Hemophilia A is a congenital disorder affecting 1 in 10,000 males associated with the absence of factor VIII activity (severe, moderate, mild) – severe is less that 1% factor VIII with major problems – raise level to 5% (moderate) and the clinical picture is markedly improved; thought leaders are moving toward prophylactic therapy (Berntorp, E and Shapiro, A.D., Modern haemophilia care, Lancet, in press, 2012). With a world population of 6 billion, there should be some 600,000 individuals with hemophilia A – my best guess is that there are likely 150,000 individuals being treated with high purity or ultrahigh purity products. Recombinant products are the therapy of choice but cost containment may drive use of the less expensive plasma-derived product (Andrew Pollock, States seek to curb patient bills for costly drugs, New York Times, April 13, 2010). The dominant cost in the treatment of hemophilia A is the cost of therapeutic product – in the US, this is approximately $100,000 (US)/year – thus, despite a somewhat small consumer base, it is business with a cash flow of approximately 2.0 billion U.S./year – and this does not consider products such as FEIBA™ or NOVOSEVEN™ which are used to treat factor VIII inhibitors. There are a number of recombinant and plasma-derived therapeutic products; All products appear to be effective in providing hemostasis. Viral safety, while a risk factor with the plasmaderived products ( Modrow, S., Wenzel, J.J., Schimanski, S., et al., Prevalence of nucleic acid sequences specific for human parvoviruses, hepatitis A and hepatitis E viruses in coagulation factor concentrates, Vox Sang. 100, 351-238, 2011) does not appear to be a significant problem with the use of plasma-derived products. A greater concern appears to be inhibitor development (Mannucci, P.M.,Mancuso, M.E., and Santagnostino, E., How we choose factor VIII to treat hemophilia, Blood, in press, 2012). The development of inhibitors is the greatest risk factor in treatment of hemophilia A but there is substantial progress in tolerization ( Auerswald, G.,Bidlingmaier, C., and Kurnik, K., Early prophylaxis/FVIII tolerization regimen that avoids immunological danger signals is still effective in minimizing FVIII inhibitor developments in previously untreated patients – long term follow-up and continuing experience, Haemophilia 18, e18-e20, 2012). Factor VIII Products -2012 • • Treatment of hemophilia A is somewhat unique in that there are no competing technologies other than replacement therapy with factor VIII protein. – The downside to this is that there are no “niche” markets for factor VIII use in other disease states. Factor VIII protein may be obtained by recombinant DNA technology or derived from plasma fractionation. – Other products from plasma such as IVIG and albumin support factor VIII manufacture from plasma (see Grifols, V., Financing plasma proteins: unique challenges, in Blood, Plasma and Plasma Proteins: A Unique Contribution to Modern Healthcare, ed. J.L. Valverde, IOS Press, Amsterdam, Netherlands, 2006 (Pharmaceuticals Policy and Law 7, 185-198, 2005-2006). – This is not different from the petrochemical industry (see Curran, L.M., Waste minimization practices in the petrochemical refining industry, J.Hazardous Mater. 29, 189-197, 1992) Concept in Hemophilia Treatment -2012 • Home Treatment – Pipe, S., Visions in haemophilia care, Thromb.Res. 124 (Suppl 2, S2-S5, 2009. – Mondorf W, Siegmund B, Mahnel R, Richter H, Westfeld M, Galler A, Pollmann H. Haemoassist--a hand-held electronic patient diary for haemophilia home care. Haemophilia. 2009 Mar;15(2):464-72. – Baker, J.R., Riske, B., Voutsis, M., et al., Insurance, home therapy, and prophylaxis in U.S. youth with severe hemophilia, Am.J.Prev.Med. 41 (Suppl. 4), S338-S345, 2011. • Group Medical Treatment – Lock, J., De Bruin, A., Scholten, M., et al., The group medical appointment (GMA) in haemophilia and von Willebrand’s disease: a new development in outpatient paediatric care, Haemophilia, in press, 2012. Recent Advances in Factor VIII • Development of products with extended circulatory half-life (see Sheridan, C., Hemophilia market awaits next-generation therapies, Nature Biotechnol. 29, 960, 2011). – Pegylated Factor VIII • Coupling to inserted surface cysteine • Coupling to lysine residues • Glycopegylation – Fusion protein with Fc domain – Factor VIII bound to PEGylated liposomes – Engineered single chain factor VIII (Schulte, S., Pioneering designs for recombinant coagulation factors, Thromb.Res. 128 (Suppl 1), S9-S12, 2011). Pegylated Factor VIII • Advantages and Disadvantages – Pipe, S.W., The hope and reality of long-acting hemophilia products, Am.J.Hematol., in press, 2012. – PEG can act as an hapten (Knop, K., Hoogenboom, R., Fischer, D., and Schubert, U.S., Poly(ethylene glycol) in drug delivery: pros and cons as well as potential alternatives, Angew.Chem.Int.Ed.Engl. 49, 6288-6308, 2010). – Clinical data is not yet available Factor VIII Engineered for Extended Half-Life • • Concept of Fc fusion protein with prolonged half-life based on binding to neonatal Fc receptor (Suzuki, T., Ishii-Watabe, A., Tada, M., Importance of neonatal FcR in regulating the serum half-life of therapeutic proteins contains the Fc domain of human IgG1: a comparative study of monoclonal antibodies and Fc-fusion proteins to human neonatal FcR, J.Immunol. 184, 1968-1976, 2010. Factor VIII-Fc fusion protein has demonstrated extended half-life in a clinical trial (Powell, J.S., Josephson, N.C., Quon, D., et al., Blood, in press, 2012. – – Inhibitor formation was not observed. Approximate 1.5 – fold extension of therapeutic half-life. Gene Therapy for Hemophilia A • Promise remains to be delivered • Immunological reactions to either vector or expressed product is a potential problem – Scott, D.W. and Lozier, J.N., Gene therapy for haemophilia: prospects and challenges to prevent or reverse inhibitor formation, Br.J.Haematol. 156, 295-203, 2012 • There has been some progress with hemophilia B – High, K.A. and Skinner, M.W., Cell phones and landlines: the impact of gene therapy on the cost and availability of treatment for hemophilia, Mol.Ther. 19, 1749-1750, 2011. Biomarkers for Factor VIII • A biomarker is defined as “a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacological responses to a therapeutic intervention.” Downing, D.O. for the Biomarkers Definitions Working Group, NIH, Bethesda, MD, USA, Biomarkers and surrogate endpoints: Preferred definitions and conceptual framework, Clin.Pharmacol.Therapeutics 69, 89-95, 2001. See also DeCaprio, A.P., Introduction to Toxicological Biomarkers, in Toxicological Biomarkers, ed. A.P. DeCaprio, Taylor & Francis, New York, NY, USA, 2006 • The major biomarker for hemophilia A is the activated partial thromboplastin time • Clinical endpoint = stopping of bleeding Assay of Factor VIII • Factor VIII is a cofactor (with apologies to hard-core biochemists) for the activation of factor X by factor IXa in a reaction which also requires calcium ions and platelets. • The partial thromboplastin time (PTT) (developed in Chapel Hill) is likely the most reliable assay. • There are all sorts of chromogenic assays which measure color and may or may not measure factor VIII. • The assay is very important since factor VIII is “sold” by the unit • Lundblad RL, Kingdon HS, Mann KG, White GC. Issues with the assay of factor VIII activity in plasma and factor VIII concentrates. Thromb Haemost. 2000 Dec;84(6):942-8. Development of Concept of Blood Transfusion • Development of transfusion medicine was critical to hemophilia therapy • Direct donor to recipient – Pope Innocent vii (1406) donors and recipient expired, physician left the country • 1628 – William Harvey, Concept of Circulation • 1665 – Richard Lower – Blood Transfusion in dogs • 1818 – James Blundell – first successful blood transfusion – Transfusion is species specific – Blood may be transfused directly from vessel to vessel – Blood may be passed into an intermediate container and remain for a short period of time before infusion into the recipient First Treatment of Haemophilia A • Lane, S., (1840), Lancet I, 185-188 – Treatment was reactive to a surgical procedure. – Use of Whole blood – Blood collected from a donor into a funnel/syringe device – 4-6 ounces – 100 – 250 mL – Within the scope of the article, the patient recovered and did reasonably well Technology Advances Required for the Use of Blood for Haemophilia A • J. Braxton Hicks – 1869 – use of sodium phosphate as an anticoagulant – although mechanism not understood. It was not very successful – Hicks, J.Braxton, Cases of transfusion with some remarks on a new method of performing the operation, Guys Hospital Reports, Series 3, Volume 14, 1-14, 1869 • Compared phosphate with whipping to remove fibrine. • Transfusion used basin to collect blood and funnels for transfer. • Low success rate – use of phosphate was based on the development of salt solutions for infusion. • Duncan, J., On re-infusion of blood on primary and other amputations, Brit.Med.J. I, 192, 1886 • Cotterill, J.M., Severe injury from dynamite, tranfusion of blood, four times, recovery, Brit.Med.J. ii, 630, 1886 Technology Advances Required for the Use of Blood in the Treatment of Haemophilia A • The development of anticoagulants for blood – As noted by P.L. Mollison in an excellent review, the use of citrate allowed the separation of donor and recipient in space while the use of glucose enabled separation in time. – Mollison, P.L., The introduction of citrate as an anticoagulant for transfusion and of glucose as a red cell preservative, Brit.J.Haematol. 108, 13-18, 2000. – Boulton, F., A hundred years of cascading – started by Paul Morowitz (1879-1936), a pioneer of haemostasis and transfusion, Transfusion Medicine 16, 1-10, 2006. Factor VIII Therapy – 1936 Status • 1840 – Lane (London) – Successful transfusion of whole blood for hemophilia • 1886 – Contrill (Edinburgh)-Phosphate anticoagulant • 1900 – Landsteiner - ABO blood grouping • 1911 – Addis – Defective prothrombin conversion in hemophilia • 1911 – Todd and White – Citrated blood for transfusion • 1915 – Ottenberg – Citrated blood for transfusion in hemophilia – correction for several days • 1916 – Addis – blood (phosphate) and serum corrected hemophilia for 24 hrs • 1916 – Rous and Turner – sucrose and citrate • 1936 – Blood bank at Cook County Hospital Nonparenteral Therapy for Hemophilia – Eley, R.C., Green, A.A., and McKhann, C.F., The use of a blood coagulant extract from the human placenta in the treatment of hemophilia, J.Pediat. 8, 135-147, 1936. • Alkaline (pH 8.5) dilute salt extract, pH adjusted to 5, ppt. collected which contained coagulant activity – Poorly soluble in pH 7.5 saline – Removed by Seitz filtration – Activity lost on oxidation, aging, and in the presence of serum • Oral administration preceded by fasting – Clotting time decreased from greater than an hour to approximately 600 seconds – effect persists for several days – Improvement of clinical signs • IM injection also showed promise – effect is delayed compared to oral administration Nonparenteral Therapy for Hemophilia – Bendien, W.M. and van Creveld, S., Investigations on Hemophilia, .J.Dis.Children 54, 713-725, 1937. • Globulin(with fibrinogen) with “activity precipitated from plasma (sodium sulfate precipitation); not obtained from serum • However, serum does have activity; activity not obtained from hemophilic serum • Showed some clinical effect with bovine serum globulin (oral administration) Cohn Fractionation • Developed by E.J. Cohn and others at Harvard University in the late 1930’s • Major emphasis during WWII • Fractionation of plasma by organic solvents, pH, and ionic strength • Still forms the basis for most human plasma fractionation • Blombäcks developed derivatives of Cohn Fraction I such as I-0 • Pavlovsky used tannic acid precipitation to prepare derivatives of Cohn Fraction I Early Development of Plasma Protein Therapeutics • • • • • • • • • • Dried Plasma – 1941 Formalin-stabilized plasma – 1942 Products from human placenta - 1952 Stable plasma protein fraction (PPF) –1952 Cohn Fraction I – 1958 Commercial IVIG – 1962 (although there were some studies in the 1940’s Cryoprecipitate – 1963 Commercial Factor VIII Preparations-1965 Rh IgG – 1968 Factor IX Concentrates – 1970 (also inhibitor products) Economic “Drivers” for Plasma Fractionation • • • • 1940 – 1960 - Albumin 1960 – 1990 - Factor VIII 1900 – Present - IVIG Recognize that, from the plasma protein perspective, plasma is a little bit like oil – there is a fixed cost for procurement unrelated to process cost/product sales. Development of Modern Factor VIII Therapeutics • Despite the advances in chromatography, plasma fractionation was (and for that matter with one exception) is still dominated by precipitation technologies. • Chromatography did have an effect on plasma-derived therapeutic products until 1985 and that was immunoaffinity chromatography; immunoaffinity chromatography was developed in 1975 and successful in this context required the production of monoclonal antibodies. • Introducing chromatography into a plasma fractionation facility is a disruptive innovation – see Govindarajan, V. and Kopalle, P.K., The Usefulness of Measuring Disruptiveness of Innovations Ex Post in Making Ex Ante Predictions, J.Prod.Innov.Manag. 23, 12-18, 2006. Development of Modern Factor VIII Therapeutics • • • • Various groups continued to attempt make more effective derivatives of Cohn Fraction I. – Jorpes, J.E., Blomback, B.,Blomback, M., and Magnusson, S., A pilot plant for the preparation of a human plasma fraction containing the human antihemophilic factor A (factor VIII) and v. Willebrand’s factor, Acta Med. Scand. Suppl. 379, 7-21, 1962 – Steinbuch, M., Precipitation methods in plasma fractionation, Vox Sang. 23, 92-106, 1972 – Newman, J., Johnson, A.J., Karpatkin, M.H., and Puszkin, S., Methods for the production of clinically effective intermediate- and high-purity factor VIII concentrates, Brit.J.Haematol. 21, 1-20, 1971 – Brinkhous, K.M., Wagner, R.H., Roberts, H.R., and Webster, W.P., Use of aliphatic amino acid precipitated antihemophilic factor in therapy of hemophilia, Bibl.Haemtol. 29, 1104-1108, 1968 Judith Pool - 1965 – Cryoprecipitate – Pool, J.G. and Robinson, J., Observations in plasma banking and transfusion procedures for haemophilic patients using a quantitative assay fo antihemophilic globulin (AHG), Brit.J.Haematol. 5. 24-30, 1959. – Pool, J.G., Hershgold, E.J, and Pappenhaggen, A.R., High-potency antihemophilic factor concentrate prepared from cryoglobulin precipitate, Nature 203, 312, 1964. – Bennett, E., Dormandy, K.M., Churchill, W.G.L., Coward, A.R., Smith, M., and Cleghorn, T.E., Cryoprecipitate and the plastic blood-bag system: Provision of adquequate replacement therapy for routine treatment of haemophilia, Brit.Med.J. 2, 88-91, 1967. – This enabled every blood bank to produce an effective therapeutic for hemophilia A. – It was not possible to scale up the cryoprecipitate step for commercial fractionation, it was possible to include a “cold drop” at the start of the conventional plasma fractionation process as the cryosupernatant fraction could be taken through the Cohn Fractionation process. – Still a useful approach (Kasper, C.K., Products for clotting factor replacement in developing countries, Semin.Thromb.Haemost. 31, 507-512, 2005) Immunoaffinity Chromatography – Pedro Cuatrecasas – 1960’s – Livingston, D.M., Immunoaffinity chromatography of proteins, Methods Enzymol. 34, 723-731, 1974 – Application to Factor VIII – 1982 – Baxter and Aventis Recombinant DNA technology – Stanford recombinant DNA – Cohen-Boyer patent • Hughes, S.S., Making dollars out of DNA. The first major patent in biotechnology and the commercialization of molecular biology, 1974-1980, Isis 92, 541-575, 2001 – Cutter/Genentech and Baxter/Genetics Institute Factor VIII Concentrates 1960-1983 • Kenneth Brinkhous, Harold Roberts, Gilbert White set the standards for hemophilia A care for several decades. – Hemophilia dog colony • Robert Wagner and colleagues at UNC-CH – Amino Acid Precipitation – Method IV Factor VIII • Alan Johnson at NYU – PEG precipitation • Virus Problems • Hougie, C., Thrombosis & Bleeding: an era of discovery, Trafford Publications, Victoria, BC, 2004 Development of Ultrahigh Purity Concentrates • Drivers for something better than high purity concentrates – Product safety –”non-A,non-B hepatitis” –was not solved by heat treatment – Fibrinogen overload – German regulatory agency – The circulatory half-life of factor VIII is approximately 14 hours; fibrinogen half-life is 4 days! Development of Ultrahigh Purity Concentrates • Immunoaffinity Chromatography – Isocratic method – best fit to manufacturing – Antibodies to factor VIII – Antibodies to von Willebrand Factor – Concomitant development of solvent/detergent technology at New York Blood Center. Manufacture of Monoclonal-Purified Factor VIII Frozen Plasma Thaw at 2-4oC/centrifuge Cryoprecipitate Supernatant Fraction to Cohn Cold Precipitate Fibrinogen and Other Stuff Supernatant Fraction to MAB-Affinity step The highly purified factor VIII preparations no longer are effective for the treatment of von Willebrand Disease – the high-molecular weight vWF is found in the cold precipitate. Aronson (Aronson, D.L. and Chang, P., Ultracentrifugal analysis of factor VIII and von Willebrand factor in therapeutic preparations, Vox.Sang.69, 8-13, 1995) suggests that the interaction is complex with data suggesting while infused factor VIII associated randomly with vWF while material purified from plasma using vWF affinity is unique Recombinant DNA Technology and Factor VIII Cutter/Genentech – Kogenate® • Baxter/Genetics Institute – Recombinate® – Advate® • Pharmacia/Wyeth(Genetics Institute) – ReFacto® (B-domainless factor VIII) Future Directions for Factor VIII Therapeutics • Oldenburg, J., Dolan, G., and Lemm, G., Haemophilia care then, now and in the future, Haemophilia 15 (Suppl 1, 2-7, 2009 – Life expectancy have moved from 11 years in 1939 to 68 years in 1980 – Prophylactic use to prevent joint bleeding – Delivery of therapy • Gene therapy • Improved product Future Directions for Factor VIII Therapeutics • Current market is almost commodity in nature – Growth through product enhancement – Factor VIII as a biopharmaceutical • Growth into developing markets is constrained by infrastructure • Market needs – – – – Product Safety Product efficacy Therapeutic effect driven by clinical endpoint While a great product requires great science, great science does not make a great product Future Directions for Hemophilia A Therapy Delivery • “Cure” – Gene Therapy • Gene Fixing • Gene Augmentation • Delivery of current product (avoid venipuncture) – – – – – Transdermal Oral Pulmonary Nasal Continuous infusion • Implantable pumps – Formulation issues – Stability issues • Modified Product (fraught with technical challenges) – Engineered – Chemically Modified Gene Therapy for Hemophilia A • Why has this not happened?? – Incredibly attractive commercial target for “proof of principle” for a technology – However, given the above, what is the “bottle?” – Is gene therapy a product or a service? – Despite all of our knowledge, we still don’t understand gene expression?? – Addition cis-factors and trans-factors?? – Unknown epigenetic factors?? – Is there a specific cell type such that, for example, you cannot get sustained expression in muscle. – Is the expression of factor VIII and von Willebrand Factor linked?? Gene Therapy for Hemophilia A • Linkage of vWF and Factor VIII – Fricke, W.A. and Yu, M.Y., Characterization of von Willebrand factor in factor VIII concentrates, Am.J.Hematol. 31, 41-45, 1989. • Highly purified factor VIII from plasma associated with a small vWF multimer • Highly purified factor VIII preparations do not correct von Willebrand disease. – Montgomery, R.R. and Gill, J.C., Interactions between von Willebrand factor and Factor VIII: were did they first meet?, J.Pediatr.Hematol.Oncol. 22, 269-275, 2000. Gene Therapy for Hemophilia A • Co-expression of VIII and vWF required? • Need different approach • Gene Therapy needs a business model – is it a service, a drug, a combination product – in some ways, has the same business issues as stem cells. • Someone will make it work because – Great target – clear clinical endpoint and several animal model systems – Great “proof-of-principle” such that company does not have to make money off success as it would validate a platform technology for a larger clinical target. Future Directions for Hemophilia A Therapeutics • Drug Delivery – Needle-less delivery (See Prabhu, S., et al., Needles and needleless devices for infusion of anti-hemophilic factor concentrate: impact on protein structure and function, Haemophilia 12, 58-61, 2006) – Infusion pumps – problems with long-term product stability – if this was easy, it would have happened for insulin. – Need a new paradigm for this problem Future Directions for Hemophilia A Therapeutics – Modified Proteins • Saenko, E.L. and Pipe, S.W., Strategies towards a longer acting factor VIII, Haemophilia 12(suppl. 3), 42-51, 2006 – PEG Modification (Baxter and Nektar) • Kingdon and Lundblad worked on this at UNC in the 1970’s with a total lack of success • Modification of lysine with small reagents results in factor VIII inactivation and the one published study on PEG modification does not provide optimism – Manning, F., et al., Effects of chemical modification on recombinant factor VIII activity, Thromb.Res. 80, 247-254, 1995 – Röstin, J., et al., B-domain deleted recombinant coagulation factor VIII modified with monomethoxy polyethylene glycol, Bioconjug.Chem. 11, 387-386, 2000 – PEGylated lipsomes (Bayer/Zilip (Amsterdam)/UC-Davis) – Engineering to Improve Stability • Pipe (Michigan) • Lollar (Emory) Future Direction for Hemophilia A Therapeutics • Peptide Analogues – Approaches based on known contact areas between factor VIII and factor IXa/factor X • Lenting, P.J., et al., Ca2+ binding to the first epidermal growth factorlike domain of human blood coagulation factor IX promotes enzyme activity and factor VIII light chain binding, J.Biol.Chem. 271, 2533225337, 1996 • Fay, P.J., et al., The A1 and A2 subunits of Factor VIIIa synergistically stimulate factor IXa catalytic activity, J.Biol.Chem. 274, 15401-15406, 1999 • Kolkman, J.A., et al., Regions 301-303 and 333-339 in the catalytic domain of blood coagulation factor IX are factor VIII-interactive sites involved in stimulation of enzyme activity, Biochem.J. 339, 217-221, 1999 • Bajaj, S.P., Factor IXa:Factor VIIIa interaction. Helix 330-338 of factor IXa interacts with residues 558-565 and spatially adjacent regions of the A2 subunit of Factor VIIIa, J.Biol.Chem. 276, 1630216309, 2001 Future Direction for Hemophilia A Therapeutics • Peptide Analogues – Solubility issues – 1-5% activity depending on phase of moon, Santa Ana winds, and sense of urgency – Not dependent on platelets – Not subject to APC control – Possibly promoting thrombosis – Similarity to poly-lysine effect? – Success depend on continuous as opposed to discontinuous site(s) – Antibody binding - Scheiflinger F, Dockal M, Rosing J, Kerschbaumer RJ. Enhancement of the enzymatic activity of activated coagulation factor IX by anti-factor IX antibodies. J Thromb Haemost. 2008 Feb;6(2):315-22. Future Directions for Hemophila A Therapeutics • Carbohydrate Modification – Is carbohydrate heterogeneity a problem? • Carbohydrate Engineering – Dwek, R.A. et al., Targeting glycosylation as a therapeutic approach, Nat.Rev.Drug Disc. 1, 65-75, 2002 – Jones, J., Controlling N-linked glycan site occupancy, Biochim.Biophys.Acta 1726,121137, 2005 Some Basic Questions about Factor VIII • • • • Why is proteolysis associated with secretion? Why is factor VIII so big? Why is circulatory half-life dependent on von Willebrand factor? Why is half-life so short ? – Hours instead of days? • Why is there is a free sulfhydryl group? • Why is copper bound? – does bound copper have anything to do with the free sulfhydryl group? • What is the role of factor VIII in the activation of factor X by factor IXa? – Factor IXa as a regulatory protease – what are factors involved in the increase in V? • Is binding to platelets unique? Walsh PN, Camp E, Dende D. Different requirements for intrinsic factor-Xa forming activity and platelet factor 3 activity and their relationship to platelet aggregation and secretion. Br J Haematol. 1978 Oct;40(2):311-31. Why is secretion of factor VIII associated with proteolysis? • Activity (or lack thereof) of single chain material – Would single-chain material be a better product? • ReFacto™ • Why is thrombin activation required for normal factor VIII function? • Is inactivation by activated protein C necessary? • You need the answers to these questions when you consider engineered/modified factor VIII • Factor VIII as a thrombotic risk factor – Pabinger I, Ay C. Biomarkers and venous thromboembolism. Arterioscler Thromb Vasc Biol. 2009 Mar;29(3):332-6.