Reading Guide
advertisement

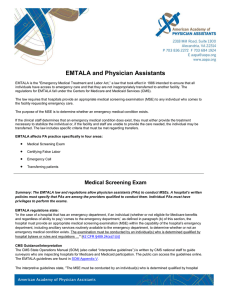
CHAA EXAM Reading Guide Pre-Encounter Part II Pages 33-41 A. CUSTOMER EXPECTATIONS 1. Customers are physicians, other departments and fellow employees, visitors, third party payers, etc. _______________ are very special healthcare customers. 2. Traditional Concerns – waits and delays in service, proper room and food temperature, noise levels, pleasant smiles are all factors that affect customer satisfaction. 3. However, according to a Press-Ganey study, staff ____________ has a major impact on a patient’s impression of a hospital. Patients may put up with ________________ amenities, but they have a low tolerance for ______________________ or _________________ care. 4. CUSTOMERS EXPECT: A. Staff Members to be caring and compassionate B. To be kept ______________ about procedures, tests, treatments, etc according to HIPAA guidelines. C. Staff members to be technically competent D. Staff to be _____________ to the inconvenience and stress that result from health problems E. Privacy is ________________ and individual __________ are anticipated and fulfilled. F. Staff to communicate with them in a language they understand. G. CLINICAL CONCERNS AND PATIENT NEEDS 1. While patients come to the hospital with many concerns, be sure to answer questions related to your ________ _____________ only and refer patient to appropriate staff for additional concerns. 2. General Questions are: Name, address, phone number, primary physician, specialists, etc. Insurance information, Medical problem or what procedure they are having. Any prep information provided by the physician. Last visit information. Financial responsibility for deductibles and co-pays, etc. Special needs according to ADA (American with Disabilities Act) guidelines. Language barriers. B. FINANCIAL CONCERNS AND PATIENT NEEDS 1. Hospitals provide care regardless of race, creed, color, sex, national origin, sexual orientation, disability, age, or ability to pay. Staff should be experienced in working with insurance companies and government agencies and should assist patients in determining how accounts are to be ________. 2. Medicare/Medicaid – patient should present ________. Information can also be obtained via the website. If patient is not enrolled, but thinks they are eligible, staff should __________ them to proper officials. C. INSURANCE 1. Patients with insurance should present their card at time of registration/admission. They may not be familiar with the specifics of their policy, so they will depend on you to verify ______________, check _____________, and to verify cost if hospital is ________________. 2. Patients without insurance may contact Patient Financial Services ________________to arrange monthly payments and look into financial assistance. D. CUSTOMER LITERACY AND COMPREHENSION 1. Ask questions to ensure patient understanding: “How can I make things clearer?” “Can you tell me what you understand so far?” 2. Some patients may nod in agreement or say they understand when they really ____________. Ask them to repeat statement in their _______ _______. 3. Patients should demonstrate understanding in co-payments, deductibles, and other financial issues as well as know where to get _______________ ______________________ if required. RESOURCE SCHEDULING A. AVAILABILITY 1. Coordinate with individual departments to assist them in _______________ their department productivity by managing their schedule accordingly. 2. Be familiar with medical tasks and procedures your facility provides as well as referral options available in your _________________. 3. Acknowledge all walk ins, even if you are with another patient. Give them an approximate _______ ________ of when you will be able to assist them. Inform them if it changes. B. SCHEDULING 1. The goal is to ensure there is ___________, ___________, and _______________ available to meet patient’s needs and to: a. Achieve maximum patient ______ and to minimize ______ time b. Ensure patient’s old chart is available if needed c. Make sure longer __________ time is scheduled if patient is coming for first time d. Obtain insurance information if prior approval is necessary e. Inform patient that Prep time is needed and they need to arrive early to be ready at procedure time f. Be sensitive to patients coming to hospital from out of town. g. Take care of the patient’s welfare and comfort. If they have fasting tests, schedule appointments early in the morning. C. DOCUMENTATION 1. Advise patients to bring any required documentation (insurance cards, ID, physician referrals) 2. Repeat appointment date and time to confirm. 3. Note special circumstances such as, “Patient will need assistance standing or “Patient requests test results be faxed to Dr. Maloy @...” 4. DOCUMENT, DOCUMENT, ________________________. If it is NOT documented, it did not ______________. D. DO’S AND DONT’S 1. See list of DO’s on page 29. 2. Don’t abbreviate or use short hand. 3. Do not record Second Hand INFORMATION, unless it’s critical. In that case, use quotations. On 3/10/10, nurse Johnson said, “Dr. Smith said to medical override patient Jones for this procedure.” E. COMMUNICATION 1. Your interaction time with the patient is short, but the information you must communicate is critical. Therefore, you need to communicate ___________ making the best use of your time. 2. To do so, you must make the necessary adjustments in your _____________________ _________________ to accommodate today’s more ____________________ style of care. F. BASIC COMMUNICATION SKILLS 1. Listen empathetically, pay attention to nonverbal behaviors, and give wellreasoned explanations. Do not take shortcuts. 2. Do not omit ____________________. 3. Do not appear ____________. 4. Keep conversations on ____________. 5. Listen without ________________. 6. Relate with your _______________. 7. Ask _______ ___________ questions. 8. Know your patient. _________________who were able to ask questions and offer opinions about the treatment process were found to report better customer service. 9. _________________ your patient by encouraging them to ask questions. 10. Manage Patient Expectations. Be prepared for a long list of concerns. 11. Provide more information in less time through _________________ education materials. 12. Go the ____________ ____________. 13. The patient will judge you (and the entire facility) based on their ____________ with you. G. SCHEDULING SYSTEM APPLICATIONS 1. Know your facilities requirements, hours of operation, and allotted time for each procedure. PRE-REGISTRATION A. REGISTRATION SYSTEMS 1. Registration systems vary from facility to facility. 2. Name 5 data elements that might be required in the registration system. See complete list p. 32. B. Medical Record Initiation 1. Medical Record number is assigned on _______ _______ to facility. 2. The MR number is used to coordinate the electronic or standard Medical Record for the patient on the initial and all subsequent visits. 3. Medical Records must be maintained for a minimum of _______ years. 4. Patient can request copies _______ __________. 5. Medical Information should be protected and may require patient ____________ for release to others. C. RESPECT FOR THE PATIENT’S NEEDS 1. Does the patient have special requests of dietary requirements? Do they require special equipment? A translator? 2. It’s important to finalize this info at pre-reg so that ___________ goes well at check-in/encounter. It’s important to remember patient values and preferences, recognize hospital’s responsibilities to provide considerate care, inform patient of their responsibilities in the care process, manage the hospital’s relationship with the patients and the public in an ethical manner. D. PATIENT AND FAMILY EDUCATION 1. Wayfinding-directions, parking, maps, drop off and pick up. 2. Make sure patient and family get understandable information about their healthcare environment, illness, treatment, and recovery process. E. CLINICAL PRE-REQUISITES 1. We need to give the patient a list of pre-requisites for their visit as well as a list of do’s and don’ts for their procedures. 2. Testing and Procedure Prequisites – (e.g., blood work, fasting or stop medication) 3. Reviewing Service/Procedure Information with patient. Whenever possible try to explain the procedure to reduce anxiety. Keep conversation in scope to your position. Tell them how long it will take, it will be cold, we have blankets but you might want to bring a sweater, wear comfortable shoes for stress tests, etc. F. FINANCIAL CLEARANCE 1. Also knows as “financial pre-determination” where provider identifies payment sources to assist the patient in determining their expected out of pocket costs, reimbursement, and alternative funding sources. 2. Patient must understand their financial obligation or portion of the final bill ____________ to receiving services. Avoiding financial ___________ promotes customer service. 3. This may be a good time to collect co-pays or deposits. G. POINT OF SERVICE COLLECTION 1 This refers to collection of patient portion of bill at the time ______________ is rendered. There are very few restrictions on asking patients for money at the time of registration. These restrictions are: a. EMTALA – patients in the ED must be medically _______________ and in a _____________ condition before asking for payment. This prevents discrimination of treatment based on _________________ status. We can ask a patient if they have insurance and make a copy of the card prior to screening/stabilization, but you cannot discuss _______________ or ____________. We cannot even accept payment prior to treatment even if patient volunteers. Doing so can result in fines and lawsuits. b. Third-Party Payers – always discuss payment with the patient or spouse, unless guarantor has given ______________________ ____________________ to discuss payment with a third party (insurance company). c. Medicare - CMS guidelines mandate that collection policies for Medicare patients be consistent with the policies for all other ____________. 3. Point of Service Non-Negotiables: Select the correct __________ and ________ number when posting payments. All payments must be posted on daily cash sheets. Patients must receive a ___________ after paying. Relevant comments must be noted on account (Patient was notified of other balances). Access Reps are responsible for collecting co-pays and deductibles whenever possible. This may be our only opportunity to speak with the patient in order to verify ____________________ information. a. Ask questions to patients who cannot pay their portions at time of service. Make every effort to collect ________ payment before offering ___________________. For those truly in need, have them fill out a financial assessment statement or charity application to assist them in determining if they are eligible for such programs. H. Regulatory Requirements 1. EMTALA – patients in the ED must be medically _______________ and in a _____________ condition before asking for payment. This prevents discrimination of treatment based on _________________ status. We can ask a patient if they have insurance and make a copy of the card prior to screening/stabilization, but you cannot discuss _______________ or ____________. We cannot accept payment prior to treatment even if patient ___________. Doing so can result in __________ and ___________. 2. EMTALA affects patients who are in ____________ _____________.