Family - Society of Critical Care Medicine
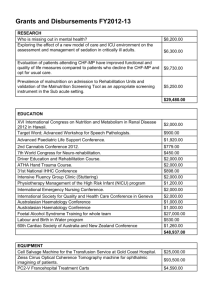
advertisement

Moderator Maurene Harvey, MPH, MCCM Critical Care Educator and Consultant Past President SCCM Lake Tahoe, Nevada, USA The AACN Clinical Scene Investigator (CSI) Academy is a 16month nursing leadership and innovation training program to empower hospital-based staff nurses as clinician leaders and change agents whose initiatives measurably improve patient outcomes and hospital bottom line Devin Bowers RN, MSN, NE-BC CSI Program Manager AACN Copyright © 2014 American Association of Critical-Care Nurses The CSI Academy seeks to enable participants to: Demonstrate the components of innovative project management Develop, plan, and implement an innovative project that targets a patient or organizational outcome on the unit Create measurable improvements in patient or organizational outcomes Copyright © 2014 American Association of Critical-Care Nurses Project Dispatch Society of Critical Care Medicine Project Dispatch is focused on patient-centered outcomes research and aims to provide clinicians with information on how to adapt and adopt successful interventions in their own ICU. Thank you to all for joining us… Submit questions throughout the presentation using the Question box located on your control panel. Today’s presentation will also include an interactive audience poll. Answer by clicking the bubble next to your choice. http://www.iculiberation.org #ICULib Presenters on Today’s Webcast Erica Edwards, RN, MSN, CCRN-CMC, CHFN Attending RN, Cardiac Intensive Care Unit Massachusetts General Hospital No disclosures Alicia Sheehan, RN, BSN Staff Nurse, Cardiac Intensive Care Unit Massachusetts General Hospital No disclosures Creating and Sustaining a Culture of Family Engagement and Empowerment in the ICU Erica Edwards, RN, MSN, CCRN-CMC, CHFN Attending RN, Cardiac Intensive Care Unit Massachusetts General Hospital Objectives • Identify factors described in the literature about the importance of family engagement • Describe the background of family inclusion in the cardiac ICU • Discuss the implementation of family engagement and empowerment in the ABCDEF bundle Poll Question Which of these statements are true as it pertains to families where you practice? Select all that apply. A. Families are considered an important part of the patient care team. B. Families are encouraged to visit daily. C. Families are coached to be active participants in achieving patient goals. D. An interprofessional approach is used to support families. MGH CSI Team Background • F for family added to ABCDE bundle for AACN CSI process improvement project “Massachusetts General Hospital Collaborate to Extubate – A Needs Assessment and Educational Program on the ABCDEF Bundle” • Participants: Erica Edwards, RN, Alicia Sheehan, RN, Norine O’Malley-Simmler, RN, and Lisa O’Neill, RN • Coaches: Colleen Snydeman, RN, and David Hanson, RN Definition of family • “Family” refers to two or more persons who are related in any way – biologically, legally, or emotionally. Patients and families define their families. (Institute for Patient and Family – Centered Care, 2010) “Significant others” may also be used. • If the patient is awake and able to answer – the family is whoever the patient designates • If the patient is unable to answer – how do we know? • Health Care Proxy • Documented in a previous admission • Who accompanied with the patient? • Why is this important? This will determine who is going to support and/or assist in decision making. Family needs • Families experience stress and anxiety when a loved one is admitted to the ICU. • Many studies have identified the needs of families of critically ill patients and nurse interventions that may decrease this stress. • In 1979 Molter conducted a study to identify specific needs of significant others. The top five needs were to: • • • • • have hope feel that the hospital staff cares for the patient be near the patient be informed of any change in the patient status know the staff (Molter, 1979) Family needs Critical Care Family Needs Inventory (CCFNI) identified five concept areas: • Proximity • Assurance • Information • Support • Comfort (Leske, 1992) Consequences of unmet needs • Anxiety and Fear (Simon, Phillip, Badalamenti, and Ohlert, Krumberger , 1997) • Depression • Post traumatic stress syndrome • Concerns that not everything possible was being done (Meyers, Eichhorn, Guzzetta, 2000) Clinical practice guidelines for support of the family • A shared decision-making model • Early and repeated care conferences • Honoring cultural requests • Spiritual support • Family presence at rounds and during resuscitation Clinical practice guidelines for support of the family • Open visitation • Family-friendly signage • Family support before, during, and after a death • Staff education and debriefing (ACCM Task Force of the SCCM, 2007) AACN Practice Alerts • AACN Practice Alert: Family presence during resuscitation and procedures. (2010) aacn.org • AACN Practice Alert: Visitation in the adult ICU. (2011) aacn.org How to add family (F) into ABCDE bundle Questions: • How can we engage families in activities that benefit the patient? • What effect does engaging families in patient activities have on the family? Advantages to family engagement For patients: • Decreases anxiety, confusion and agitation (Hupcey, 1999) • Reduces cardiovascular complications (Fumigalli, Boncinelli, Lo Nostro, et al., 2006) • Decreases the ICU LOS (Davidson, Powers, Hedayat, et al. 2007) • Makes the patient feel more secure • Increases patient satisfaction • Promotes quality and safety Family contributions • “Active presence” to facilitate communication and what is known about the patient’s condition • “Protector” creates sense of safety by having a family member at the bedside to watch over and advocate for them • “Historian” provides information about patient’s medical history and personal preferences Family contributions (cont) • Facilitators” to maintain meaningful relationships • “Coaches” to provide encourage and inner strength • “Voluntary caregiver” assists in providing actual care (McAdam, Arai, and Puntillo, 2008) Family contributions to patient recovery As part of the care team, families can assist with: • Being present during SATs • Delirium assessment and interventions • Early mobilization • Your thoughts? Engaging the family • Provide education • What to expect • Family roles • Model caring behaviors • Support • Encouragement Google images, 2015 Engaging the family in the MGH Cardiac Intensive Care Unit Alicia Sheehan, RN, BSN Massachusetts General Hospital The culture of family centered care in MGH Cardiac Intensive Care Unit Fostering a change in culture • Unrestricted visiting hours • Volunteer liaison in waiting room • Cots in rooms • Comfort cart (meals provided during EOL care) • “Moment of Silence” Moment of Silence Script We would like everyone here to join in remembering ___(name)___ who was entrusted to our care. He/she was a daughter / son wife / husband mother/ father Some thing(s) we got to know about her/him were: Something(s) I will remember about her/him are: Let’s join in a moment of silence to remember her/him and to reflect on her/his life and death, and what we did to help her/him. (pause 30 seconds or more) Thank you. Fostering a change in culture • Family presence during resuscitation and procedures • Family presence at rounds • Interprofessional access available to family including social worker, chaplain, nutritionist, PT, OT, RT, case manager Innovations creating a culture change Responsible Decision Making Rounds • Complex patients are discussed • Occurs weekly • Uses interprofessional approach • Right care, right time, right patient Innovations creating a culture change Attending Nurse: New Role at MGH • Assists with patient’s journey through the hospital stay, including discharge • In the ICU, focuses on patient and family needs for communication, education, support • Facilitates daily interprofessional rounds and long term rounds Organizational core values Incorporated into the values of the Massachusetts General Hospital Patient Care Services is the statement of recognition of the importance of patients and their families in the decisions affecting their care This value extends throughout the life cycle, including the end of life. The family is viewed as an extension of the patient and therefore should be considered in all aspects of the patient’s care. (Patient Care Services, 2009). Families of critically ill patients and the effect of nursing interventions. • This article reviewed the evidence related to family needs • Listed implications for practice: • • • • • • • Encourage more family visitation Encourage child visitation Explore animal visitation Facilitate nurse-family interactions Allow family presence during procedures and resuscitation Refer families to support or educational groups Use hospital volunteers for waiting area (Gavaghan, Carroll, 2002) Visiting preferences of patients in the intensive care unit and in a complex care unit • The purpose of this study was to describe patient preferences for family visiting in an ICU and in a complex medical care unit. Patients described: • Visiting was a non-stressful experience • Having visitors offered moderate levels of reassurance, comfort and calming • Valued the fact that visitors could interpret information • That visitors could provide information to assist health care providers’ understanding of the patient • Were very satisfied with a visiting guideline that is flexible enough to meet their needs and those of their family members (Gonzalez, Carroll, Elliott, 2004) Changes in provider perceptions of family presence during resuscitation and invasive procedures. Purpose: to measure changes in perceptions of healthcare providers (HCPs) in the cardiac intensive care unit (CICU) before and after an implementation of an educational program that included approval of a unit-based guideline for family presence (FP) during resuscitation and invasive procedures. Result: the educational program and the approval of a unitbased guideline improved HCPs' perception of risk and benefit of FP during resuscitation and the actual presence of family during resuscitation. (Edwards, Despotopulos, Carroll, 2013) Narratives • Culture of narrative writing • Grounded on the work of Benner • Focus is on patient and family centered care • Highlights excellence in practice • All members of the Patient Care Services (nursing, PT, OT, RT, SLP, SW, chaplain) Nurses perceived barriers to family involvement • Assessing appropriateness • Respecting unit culture/boundaries • Overstaying • Clutter in room/safety issues • Need for limit setting • Balancing patient privacy • Patient and family specific Families as active members of the patient care team Families in the CICU: • Provide a patient history • Provide a HCP document • Identify spokesperson • Educate staff on cultural and spiritual needs • Active presence for the patient • Assist with language and communication barriers Families as active members of the patient care team • Assist to calm patient during vent wean • Identify changes in patient’s condition and behavior (aids with delirium assessment) • Encourage or coach patients during PT or procedures • Advocate for the patient • Reduce need for restraints Benefits of family engagement far outweigh perceived barriers A team approach is needed to support, educate and communicate with families. • Involvement of interdisciplinary team is critical to the success of family engagement • Demonstrated in our project logo CSI logo Interprofessional Collaboration Nurses Chaplain Physicians Patient & Family Respiratory Care Dietician Physical Therapist Social Worker Engaging families in the ICU In summary: • Family engagement and empowerment is fostered by the culture of the unit. • A multidisciplinary approach is necessary to support family engagement. • Families can be included in many aspects of patient care and that benefits both patient and family. Acknowledgements • Jeanette Ives Erickson, RN, DNP, FAAN • Theresa Galvin, RN, MS • Vivian Donahue, RN, MSN • Susan Stengrevics, RN, MSN • Colleen Snydeman, RN, PhDc • Susan Lacey, RN, PhD • Dave Hanson, RN, MSN References • AACN Practice Alert: Family presence during resuscitation and procedures. (2010) aacn.org • AACN Practice Alert: Visitation in the adult ICU. (2011) aacn.org • Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force (2007). Davidson, J. et al. Crit Care Med 35(2) 605-23 • Edwards, E., Despotopulos, L., Carroll, D. (2013) Changes in provider perceptions of family presence during resuscitation and invasive procedures. Clinical Nurse Specialist Volume 27(5). 239-44 References • Fumigalli, S., Boncinelli, L., Lo Nostro, A. , et al. (2006) Reduced cardiocirculatory complications with unrestricted visiting policy in an intensive care unit: results from a pilot, randomized trial. Circulation 113, 946-52 • Gavaghan, S., Carroll, D. (2002) Families of critically ill patients and the effect of nursing interventions. Dimensions of Critical Care Nursing Volume 21(2). 64-71 • Gonzalez, C., Carroll, D., Elliott, J., Vallent, H. (2004) Visiting preferences of patients in the intensive care unit and in a complex care unit. American Journal of Critical Care 13(3) 194-8. References • Davidson JE, Powers K, Hedayat KM, et al. (2007) Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004-2005 Crit Care Med. 35(2) 605-22 • Leske, J. S. (1992). Needs of adult family members after critical illness: a prescription for interventions. Critical Care Nursing Clinics of North America. 4, 587-96 • McAdam, JL., Arai,S. and Puntillo, KA. (2008). Unrecognized contributions of families in the intensive care unit. Intensive Care Med. 34, 1097-1101 • Meyers TA, Eichhorn DJ, Guzzetta CE, et al. Family presence during invasive procedures and resuscitation: the experiences of family members, nurses, and physicians. Am J Nurs. 2000;100(2): 32-42 References • Rukstele, C., Gagnon, M. (2013) Making strides in preventing ICU acquired weakess: involving family in early progressive mobility. Crit Care Nursing Quarterly 36(1), 141-7 • Simon SK, Phillip K, Badalamenti S, Ohlert J, Krumberger J. (1997) Current practice regarding visitation policies in critical care units. Am J Crit Care. 6(3):210-217. • Hupcey JE. (1999) Looking out for the patient and ourselves—the process of family integration into the ICU. J Clin Nurs. 8(3):253 Questions/Comments Erica Edwards, RN, MSN, CCRNCMC, CHFN Attending RN, Cardiac Intensive Care Unit Massachusetts General Hospital Alicia Sheehan, RN, BSN Staff Nurse, Cardiac Intensive Care Unit Massachusetts General Hospital