Discussion of SP Case
advertisement

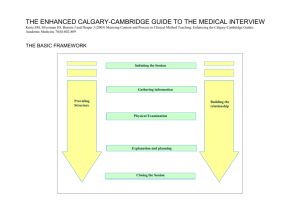
Discussion of SP Case Agenda Discussion of SP case Review key principles of clinical medicine Andrea Milam: Moral reasoning, course/program evaluation, research Course evaluation: Defining issues test The Medical Interview Not a one-way interrogation It is a two-way collaborative and dynamic interaction The Medical Interview Most important part of the medical encounter Functions Structure, content, process Requires communication and interpersonal skills What are the functions of the medical interview? Functions of the Medical Interview Build the relationship Assess the patient’s problems Manage the patient’s problems (education, negotiation, motivation) What is the basic structure of the medical encounter? Structure and Tasks of the Medical Encounter Initiate the session Gather information Explaining and planning Closing the session Building the relationship Provide structure to the encounter Initiating the Session Gathering information Providing Structure Building the relationship Physical Examination Explanation and planning Closing the Session Initiating the Session: Students How did you initiate the session? What were you trying to accomplish? What steps did you take? Initiating the Session: SPs How did they do? Initiating the Session Preparation Establishing initial rapport Identifying the reason(s) for the encounter Preparation Puts aside last task, attends to self comfort Focuses attention and prepares for this encounter Opening the Interview Objectives Establish supportive environment and initial rapport Awareness of pt’s emotional state ID all pt’s issues/problems he/she wishes to address Negotiate agenda for encounter Develop partnership with pt Opening the Interview Convey Respect Empathy Support Non-judgmental/unconditional positive regard Interest in the patient as an individual Opening the Interview Greet the patient Verify/obtain pt’s name Introduce self and clarify role and goals of interview Obtain pt’s consent for interview Attend to patient’s comfort Initial rapport-building skills Identify the reason(s) why the patient came to the doctor Negotiate priorities Elicit the patient’s expectations Opening the Interview Greet the patient Verify/obtain pt’s name Introduce self and clarify role and goals of interview Obtain pt’s consent for interview Attend to patient’s comfort Initial rapport-building skills Identify the reason(s) why the patient came to the doctor Negotiate priorities Elicit the patient’s expectations Initial Rapport Building Skills Initial non-verbal communication Respect Attending to patient’s comfort Engage the patient Initial Rapport Building Skills Initial non-verbal communication Respect Attending to patient’s comfort Engage the patient What percent of communication is non-verbal? What percent of communication is non-verbal? Around 80% Nonverbal Communication Facial Expressions Physical Environment Territory and Interpersonal Space Body Language Paralanguage Touch Nonverbal Communication “You’re my doctor???!!” Rapport Rapport Rapport is one of the most important features or characteristics of human interaction. It is commonality of perspective, being in "sync", being on the same wavelength as the person you are talking to. What Are Rapport Skills? Start with greeting and getting to know the pt or checking how the pt is doing Many are nonverbal expressing interest and concern “Positive talk” personally supportive Avoiding “negative talk” criticism, blaming, arrogance Lang Rapport: Pros Shows interest in the pt as a person Initial non-clinical talk helps calibrate the future communication style, language, spontaneity For non-emergent care in an emergency setting, pts still frequently appreciate personal interest at the beginning of the interview Lang Rapport: Cons On occasion, a pt in an ambulatory setting will want to “get right down to business” Frequently in emergency situations pts want their disease taken care of first If insincere or overdone, positive talk can appear like “kissing up” Lang Barriers to Use of Rapport Building In an effort to be “professional”, some students may avoid a relaxed, personally interested posture Gender issues may create a fear that personal interest may attract unwanted personal advances The interviewer may have negative personal feelings or experiences with regards to the pt or clinical situation (counter-transference) Lang Genuineness and Respect are the Key Genuineness - "Be truthful about who you are personally and professionally. Learn to compartmentalize your personal and professional selves." Respect - "Be nonjudgmental. Convey unconditional positive regard. Value the other person as an individual even if you don't like them." Bayer Initial Rapport Building Skills Initial non-verbal communication Respect Attending to patient’s comfort Engage the patient Rapport Building Skills: Engage the Patient Engage Defined A connection which continues throughout the encounter Person-to- person Professionally, as partners Bayer Engagement: Techniques Join the patient Use the first few minutes to build rapport Use a pleasant, consistent tone of voice Bayer Engagement: Techniques Be as curious about the person as you are their medical condition “Care more particularly for the individual patient than for the special features of the disease” Sir William Osler Examples of “Non-Medical” Conversation Topics Begin the interview with a personal inquiry, for example: Ask about something in the patient’s background that catches your interest Identify a shared interest, experience, or background Engage in small talk Ask about demographic data, such as name, age, occupation, and marital status Ask about the patient’s general health before asking the reason for the visit. Find something you like about each patient (Billings and Stoeckle,1999) Building Rapport New patient: “Before we begin, tell me something about yourself.” Return patient: Mention something personal from a previous visit Opening the Interview Greet the patient Verify/obtain pt’s name Introduce self and clarify role and goals of interview Obtain pt’s consent for interview Attend to patient’s comfort Initial rapport-building skills Identify the reason(s) why the patient came to the doctor Negotiate priorities Elicit the patient’s expectations Identify the Reason(s) why the Patient came to the Doctor Students Why did the patient come to the doctor? Identify the Reason(s) why the Patient came to the Doctor SPs Why did you come to the doctor? Identify the Reason(s) why the Patient came to the Doctor Most patients have more than one concern (mean around 3 concerns) The first concern may not be the most important to the patient Identifying all pt’s concerns allows for time allocation Skills: Identifying the reason(s) for the patient’s visit The opening question: identifies the problems or issues that the patient wishes to address (e.g. “What would you like to discuss today?”) Listening to the patient’s opening statement: listens attentively without interrupting or directing patient’s response Skills: Identifying the reason(s) for the patient’s visit Screening: checks and confirms list of problems or issues that the patient wishes to cover (e.g. “so that’s headaches and tiredness, is there anything else you’d like to discuss today as well?”) Agenda setting: negotiates agenda and format of interview taking both patient’s and physician’s needs into account Initiating the Session Gathering information Providing Structure Building the relationship Physical Examination Explanation and planning Closing the Session Gathering Information Students Tell us about the patient’s abdominal pain Tell us what information you gathered on this patient’s past and current ongoing medical problems What other information about this patient you feel is pertinent? Gathering Information SPs How did the students do? Did they miss any pertinent information? Did they gather information to understand your perspective? Content of the Medical History Chief complaint and survey of problems History of present illness Past medical history Family history Patient profile and social history Review of systems Chief complaint and survey of problems The one or more concerns causing the patient to seek care. Encourage the pt to tell you all of his/her concerns. You may negotiate what will be covered due to time limitations History of Present Illness Amplifies each of the patients concerns. Includes the patient’s thoughts and feelings about the illness. The narrative thread History of Present Illness Seven content items: 1. Location: Where does it hurt? 2. Quality: What does it feel like? 3. Severity: How bad is it? 4. Timing: When did it start? How long does it last? 5. Context: What were you doing when it first began? 6. Modifying factors: Does anything make it better or worse? 7. Associated symptoms: What other symptoms are associated with this problem History of Present Illness Patient’s perspective of the illness FIFE F = Function: How has this affected you? I = Ideas: What do you think caused this problem? F = Feelings: What concerns you about this problem? E = Expectations: How to you hope we can help you with this problem? Past Medical History An exploration of the person’s overall health before the present problem, including all past medical and surgical experiences. Past Medical History Hospitalizations Surgeries Illnesses Trauma Medications Allergies Pregnancies Transfusions Exposures Past Medical History Health Maintenance Periodic health examinations Immunizations Injury prevention Exercise Family History An exploration of a family’s health, past medical experiences, illnesses, social experiences, deaths, and genetic and environmental circumstances Family History Current health of parents, siblings, and children History of significant illnesses in the family, such as hypertension, diabetes, coronary artery disease, etc. Social History Information that helps in the understanding of the patient as an individual Helps to begin to get a view of the patient’s illness in the context of his/her life Social History Patient profile Place of birth and upbringing, education, military, occupations, hobbies Living situations, family, and relationships, residence Impact of illness on life Health-risk behaviors Life-stress and satisfaction Review of Systems Assesses for the presence or absence of common symptoms related to each major body system Review of Systems General/constitutional Skin Eyes ENT Pulmonary Cardiovascular Digestive Genitourinary Hematological Immune Endocrine Musculoskeletal Neurological Psychiatric History of Present Illness Students: For this patient Seven content items: 1. Location: Where does it hurt? 2. Quality: What does it feel like? 3. Severity: How bad is it? 4. Timing: When did it start? How long does it last? 5. Context: What were you doing when it first began? 6. Modifying factors: Does anything make it better or worse? 7. Associated symptoms: What other symptoms are associated with this problem History of Present Illness SPs Seven content items: 1. Location: Where does it hurt? 2. Quality: What does it feel like? 3. Severity: How bad is it? 4. Timing: When did it start? How long does it last? 5. Context: What were you doing when it first began? 6. Modifying factors: Does anything make it better or worse? 7. Associated symptoms: What other symptoms are associated with this problem History of Present Illness Students: For this patient Patient’s perspective of the illness FIFE F = Function: How has this affected you? I = Ideas: What do you think caused this problem? F = Feelings: What concerns you about this problem? E = Expectations: How to you hope we can help you with this problem? History of Present Illness SPs Patient’s perspective of the illness FIFE F = Function: How has this affected you? I = Ideas: What do you think caused this problem? F = Feelings: What concerns you about this problem? E = Expectations: How to you hope we can help you with this problem? Gathering Information Skills Skills: Gathering information: Exploration of Problems Encourages the patient to tell story (narrative) Uses open-ended and closed-ended questions, appropriately moving from open-ended to closed, non-directive to directive Avoids or explains jargon, avoids other language “pitfalls” Listens attentively, allowing patient to complete statements without interruption and leaving space for patient to think before answering or go on after pausing Listening Listening “Listening to a patient narrative is also observing. Here, what the patient actually said and the exact manner - words, pausing, pitch, emphasis, and so on - in which it is said is the observation that must be separated from what the listener thinks the patient meant” Eric Cassell, MD Listening Doctors hope they are good listeners already. But how often do we really listen? How often do we anticipate what is going to be said next, and jump in with our thoughts and ideas as soon as there is a pause? Listening Listening is an art, a skill, and needs to be learned and practiced. As listeners we need to be warm, caring and non-judgmental. We need to make a special effort to tune in to the person’s feelings, and have a genuine respect for the person calling. Effective listening There are three components in effective listening: Attending behavior Effective use of silence (wait time) Active listening Listening: Attending Behavior Eye contact Body language Tone of voice Following the conversation This means that you do not interrupt, or change the subject or introduce new topics. Attending well will mean that the patient does most of the talking, and that you don’t lecture.. Active Listening Facilitation - encourage client to continue; “uhhuh” Clarification - obtain more info; “What do you mean by -------- ?” Restatement - repeating what was said using different words Active Listening Reflection - repeating what the patient just said to encourage elaboration Interpretation - used to share a conclusion drawn from data Summary (checking)- condenses & orders data for sequencing events Listening With Empathy Empathy is understanding Empathy is not sympathy Sympathy is an expression of one’s own feelings about another’s predicament Empathy is an attempt to fell with another person, to understand their point of view. Skills: Gathering information: Exploration of Problems Facilitates patient’s responses verbally and nonverbally (use of encouragement, silence, repetition, paraphrasing) Clarifies patient’s statements which are vague or need amplification (e.g. “Could you please explain what you mean by ‘lightheaded’?” Checks with patient to insure understanding Helps the patient organize the narrative thread, checks dates, helps establish chronology, directs Skills: Gathering information: Understanding the patient’s perspective Function: determines how each problem affects the patient’s life Ideas: determines and acknowledges patient’s ideas (i.e. beliefs regarding cause) regarding each problem Feelings and thoughts: encourages expression of the patient’s feelings (i.e. worries) Expectations: determines the patient’s goals, what help the patient had expected for each problem Cues: picks up on verbal and non-verbal cues (body language, speech facial expressions, affect); acknowledges and checks out as appropriate FIFE Function Ideas Feelings Expectations FIFE Function Ideas Feelings Expectations Patient’s presents problem Gathering Information Parallel search of two frameworks Illness framework Patient’s agenda Disease framework Doctor’s agenda ideas concerns expectations feelings thoughts effects symptoms signs investigations understanding pathology Understanding the Patient’s unique Experience of illness Differential Diagnosis Integration of the 2 frameworks Explanation and planning: shared understanding and decision-making Initiating the Session • preparation • establishing initial rapport • identifying the reason(s) for the consultation Gathering information Providing • exploration of the patient’s problems to discover the: Structure biomedical perspective • making organisation overt Building the relationship the patient’s perspective background information - context • using appropriate non-verbal behaviour • developing rapport • involving the patient Physical examination • attending to flow Explanation and planning • providing the correct amount and type of information • aiding accurate recall and understanding • achieving a shared understanding: incorporating the patient’s illness framework • planning: shared decision making Closing the Session • ensuring appropriate point of closure • forward planning AN EXAMPLE OF THE INTER-RELATIONSHIP BETWEEN CONTENT AND PROCESS Gathering Information Process Skills for Exploration of the Patient’s Problems patient’s narrative question style: open to closed cone attentive listening facilitative response picking up cues clarification time-framing internal summary appropriate use of language additional skills for understanding patient’s perspective Content to Be Discovered the bio-medical perspective (disease) sequence of events symptom analysis relevant systems review the patient’s perspective (illness) ideas and beliefs concerns expectations effects on life feelings background information - context past medical history drug and allergy history family history personal and social history review of systems Patient's Problem List Exploration of Patient's Problems Medical Perspective – disease Sequence of events Symptom analysis Relevant systems review Patient's Perspective - illness Ideas and beliefs Concerns Expectations Effects on life Feelings Background Information - Context Past Medical History Drug and Allergy History Family History Personal and Social History Review of Systems Physical Examination Differential Diagnosis - Hypotheses Including both disease and illness issues Physician's Plan of Management Investigations Treatment alternatives Explanation and Planning with Patient What the patient has been told Plan of action negotiated Diagnosis of Abd Pain What are possible causes of abd pain in this patient? What is you number 1 candidate? What would you expect to find on physical exam? What further diagnostic tests are indicated if any? What would you tell the patient? What are your treatment options? How would you treat this patient? Putting Clues Together "Medicine is a science of uncertainty and an art of probability." Sir William Osler Hypothetico-deductive method Initial Clues/Initial Hunches Inquiry Differential diagnosis Hypothesis Generation Case Building Hypothesis Evaluation Diagnostic Decision Therapeutic Decision Epidemiology Does this patient have any risk factors to predispose to a cause of abdominal pain? Describe the patient’s abdominal pain? Where is it located? Differential Diagnosis Location of pain Differential Diagnosis Epigastric pain Peptic ulcer disease Gastroesophageal reflex disease Gastritis Pancreatitis Myocardial infarction Ruptured aortic aneurysm Describe the patient’s abdominal pain? Location, radiation Quality Severity Timing: onset, duration, frequency Setting or context Modifying factors: aggravating, alleviating Associated symptoms Diagnosis Epidemiology Etiology Presentation Physical examination Peptic ulcer May be associated with Helicobacter pylori infection. Risk factors include COPD, NSAID use, tobacco and alcohol use. Nonradiating epigastric pain that starts 1–3 hours after eating and is relieved by food or antacids. Pain frequently awakens patient at night. Epigastric tenderness without rebound or guarding. Perforation or bleeding leads to more severe clinical findings Occur in all age groups. Peak at age 50. Men affected twice as much as women. Severe bleeding or perforation in less than 1% of patients. Pathophysiology of Peptic Ulcer Disease Is this the whole story of abdominal pain in this patient? Describe this patient’s peptic ulcer disease “illness” Make a Problem List for This Patient Make a Problem List for This Patient Peptic ulcer disease Stress Depression Insomnia Back pain Smoking Alcohol problem Other Aspects of Encounters With This Patient Depression Diagnosis Therapy Office-based counseling Medications Refferal Stress Negotiation Other Aspects of Encounters With This Patient Rapport and trust Empathy Dealing with emotions Health behavior change Smoking cessation Alcohol Determine degree of problem: CAGE Alcohol counseling Prevention and health promotion End of Case Discussion Questions? Comments? Evolution of a Physician: How Do We Get There? First-Year Medical Student Practicing Physician Where You Are Now Knowledge Skills Attitudes Experiences Personal development Where do you want to be? Evolution of a Physician: How Do We Get There? Professional Development •Knowledge •Skills •Attitudes First-Year Medical Student Practicing Physician Who are physicians accountable to? Who are physicians accountable to? Patients Other healthcare professionals Communities Accreditation boards and medical societies Healthcare system Society in general Themselves and their families What do these stakeholders expect of physicians? That we are competent Defining Professional Competence The habitual and judicious use of communication, knowledge, technical skills, evidence-based decision-making, emotions, values and reflection to improve the health of the individual patient and the community. Epstien What Patients Want Most patients take our technical expertise for granted. What they evaluate, however, is the art of the care, the human side of how the care is delivered, and the compassion and concern for their welfare exhibited by physicians. John J. Gartland, MD “Mastery of the broad spectrum of knowledge, skills, and attitudes necessary to accurately and compassionately perform our role defines what it means to be a physician and not just a technician.” Trainer and Kirug ACGME Competencies Patient care Medical Knowledge Interpersonal and communication skills Professionalism Systems-based practice Practice-based learning and improvement Where You Want to Be Component in: Patient care Medical Knowledge Interpersonal and communication skills Professionalism Systems-based practice Practice-based learning and improvement The Evolution of a Physician is Never Complete ? “The hardest conviction to get into the mind of a beginner is that the education upon which he is engaged is not a college course, not a medical course, but a life course, for which the work of a few years under teachers is but a preparation.” Sir William Osler Questions What is the most powerful diagnostic and therapeutic tool in medicine? Healthcare Professionals Healthcare Professionals Teams are more effective than individuals Must exhibit professionalism Questions What is the most crucial knowledge one needs in medicine? Self-Knowledge Self-assessment What you know and what you don’t know What you know about the way you make decisions: moral reasoning Biases Life-long learning and improvement Reflection Questions What is the most important skill one needs in medicine? Communication Communicating with patients and their families Communicating about the patient Oral and written communication Team communication Communicating about medicine and science Teaching Questions What is the one most important attitude one needs in medicine? Caring “One of the essential qualities of the clinician is interest in humanity, for the secret in the care of the patient is caring for the patient.” Francis W. Peabody, MD. JAMA, March 19, 1927