Associated Conditions
advertisement

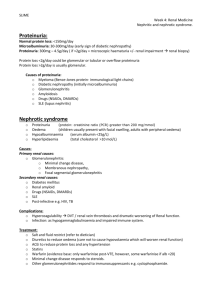
KIDNEY DISEASES Developmental disorders Glomerular diseases Tubulo-interstitial diseases Urinary stones Obstructive uropathy Tumors LUPUS GLOMERULONEPHRITIS GN-Common feature of SLE Immune complex-deposition -in situ formation Associated with deposits in -blood vessels -tubular BM -interstitium Complementinflammation LUPUS GLOMERULONEPHRITIS I: No lesion II: Mesangial III: Focal proliferative IV: Diffuse proliferative V: Membranous VI: Chronic PATHOLOGY OF SLE GN Highly variable Immune complexes vary in/size/location • Subendothelial • Intramembranous • Subepithelial • Mesangial Proliferation of Mes, End, Ep cells; PMN and MACROPHAGES Fibrinoid necrosis IF-”full house” (ML Ig) KIDNEY ANATOMIC COMPARTMENTS Glomerulus Tubules Blood vessels Interstitium Collecting system (Callices & Pelvis) COMPONENTS OF THE GLOMERULUS Capillary basement membrane Mesangium Bowman capsule Cells • Endothelial • Epithelial • Mesangial THE JUXTAGLOMERULAR APPARATUS Afferent arteriole Macula densa – ascending loop of Henle Lacis cells - Renin CONGENITAL RENAL ANOMALIES Agenesis – Potter syndrome Ectopia Fusion Dysplasia Polycystic kidney disease POLYCYSTIC KIDNEY DISEASE Autosomal dominant (adult) (1:1,000) Autosomal recessive (infantile (1:30,000) Medullary cystic disease complex (1:10,000) Medullary sponge kidney Acquired cystic renal disease AUTOSOMAL DOMINANT POLYCYSTIC KIDNEY DISEASE Common kidney disease (1:1,000) 10% of all transplant/dialysis patients ADPKD-1 gene (polycystin) mutation 85% Bilaterally enlarged kidneys (>3,000g) Symptoms appear in adult life Renal failure 5-10 years thereafter ADPKD Associated Conditions Liver cysts (30%) Splenic cysts (10%) Pancreatic cysts (5%) Cerebral aneurysms (20%) Diverticulosis coli GLOMERULAR DISEASES Asymptomatic hematuria/proteinuria Nephrotic syndrome Nephritic syndrome Rapidly progressive glomerulonephritis Chronic nephritis KIDNEY DISEASES (MNEMONIC “ANNURIC”) A N N U R I C Asymptomatic hematuria/proteinuria Nephrotic syndrome Nephritic syndrome Urolithiasis Rapidly progressive glomerulonephritis Interstitial and tubular diseases Chronic renal disease CHRONIC RENAL FAILURE (UREMIA) General symptoms – weakness, fatigue Cardiovascular – hypertension, pericarditis G.I. – nausea, vomiting, diarrhea CNS – lethargy, confusion, coma Muscles – twitching, weakness Bones – osteodystrophy Metabolic – acidosis, PK, BUN, Cr. Endocrine - parathyroids NEPHROTIC SYNDROME Proteinuria (“nephrotic range” >3.5g/24h) Hypoalbumimenia Edema Hyperlipidemia Lipiduria CAUSES OF NEPHROTIC SYNDROME Disease Children(%) Minimal change GN Adults(%) 75 20 5 40 MPGN I 5 5 Other GN 5 20 Membanous GN NEPHRITIC SYNDROME Hematuria Proteinuria Hypoalbuminemia Oliguria (GFR, Cr, BUN) Edema (salt and water retention) Hypertension DIAGNOSTIC FEATURES OF GLOMERULAR DISEASES Light microscopy • Cellularity • Extracellular matrix Special stains (PAS, amyloid) Immunofluorescence microscopy (Linear, granular, mesangial, irregular deposits) Electron microscopy (deposits of immune complexes, BM changes, amyloid) MINIMAL CHANGE GLOMERULOPATHY Most common cause of nephrotic syndrome in children E/P: unknown (?immune) Path: normal by LM and IF EM: fusion of foot processes CL: Nephrotic sy – responds to steroids Dd: FGS FOCAL SEGMENTAL GLOMERULOSCLEROSIS Def: 15% of all nephrotic syndromes; heterogenous group of diseases E/P: unknown-circulatory glomerular injury (?) HIV, I-V drug abuse CHD, obesity, sickle-cell disease Path: focal and segmental glomerular hyalinosis “Collapsing” pattern (e.g. HIV) Trapping of serum proteins (IF and EM) Clin: Nephrotic syndromeESKD (5-20y) If HIV relatedESKD (1 year) MEMBRANOUS NEPHROPATHY Def: Most common cause of nephrotic syndrome in adults (40%) Immune complexBM thickening E/P: Primary (unknown) Secondary (SLE, HBV, drugs, cancer) Path: Subepithelial deposits of immune complex CL: Nephrotic syndrome (25% recover, 50% persist, 25% progress) DIABETIC GLOMERULOSCLEROSIS Def: Diabetes caused BM thickening Proteinuria renal failure (leading cause in US) E/P: BM synthesis , nonenzymatic glycation (?) Path: Diffuse global thickening of BM Nodular sclerosis (K-W) Arteriolosclerosis Trapping of serum proteins Clin: Proteinuria (in 50% diabetics) ESKD (30% all in the US) DIABETIC KIDNEY DISEASES Glomerulosclerosis Arteriolosclerosis Hypertension Pyelonephritis Papillary necrosis AMYLOIDOSIS AA amyloid – systemic disease AL amyloid – multiple myeloma Deposits of amyloid – glomeruli (mesangial) - arterioles - tulular BM Nonselective proteinuria – nephrotic sydrome (60%) renal failure (with large kidneys!) ACUTE POSTINFECTIOUS GN Def: Acute nephritic syndrome 1-2 weeks after infection E/P: immune response to A -hemolytic streptococci (other infections Staph, malaria, HBV less common) Path: Acute glomerulonephritis Clin: Childhood nephritic syndrome 90% recover 9% presistent hematuria/proteirunria 1% chronic renal disease PATHOLOGY OF ACUTE POSTINFECTIOUS GN LM: hypercellularity (endo + MES + PMN) IF: Irregular deposits of Ig, Compl. EM: Deposits (mesang + BM) “HUMPS” MEMBRANOPROLIFERATIVE GLUMERULONEPHRITIS Type I Def: Immune mediated presistent GN Mesangiocapillary cell proliferation and BM reduplication E/P: Immune comples deposition in glomeruli •Primary (unknown cause) •Secondary (SBE, chronic infection, HCV, cryoglobulinemia, cancer) Path: Lobular gromerulonephritis Clin: Older children/young adults Nephritic or nephrotic syndrome Progressive – 50% ESKD (10 years) MEMBRONOPROLIFERATIVE GLOMERULONEPHRITIS Type II Def: Immune mediated persistent GN Dense deposits in GBM E/P: C3 nephritic factor (IgG) Stablizes the activated C3 convertase Path: Similar by LM to MPGN-I EM-shows linear dense deposits in GBM RENAL BIOPSY IN SLE To determine 1. Category (class) 2. Activity 3. Extent 4. Chronicity Note: Class IV-worst prognosis Class V-no response to steroids IgA NEPHROPATHY (BERGER) Most common form of GN Young adults (15-30 years) Pathology: IgA deposits in mesangium -varied severity Clin: Protean manifestations 40% asymptomatic microscopic hematuria 40% bouts of macro hematuria 10% nephrotic syndrome 10% renal failure ANTI-GBM ANTIBODY GN RPGN mediated by antibody Antibody to collagen IV Linear IF Fibrinoid necrosis of GBM Crescentic GN Goodpasture syndrome CRESCENTIC GLOMERULONEPHRITIS 1. Anti-GBM glomerulonephritis (inc. Goodpasture syndrome) 2. ANCA granulonephritis (inc. Wegener granulomatosis, micr. polyangitis, Churg-Strauss syndrome) 3. Immune complex glomerulonephritis (inc. Henoch-Schonlein purpura, cryoglobulinemia) 4. Non-immune ANCA GLOMERULONEPHRITIS Necrotizing and crescentic ANCA (PMN myeloperoxidase, proteinase 3) No immune deposits in glomeruli Respond to immunosuppresion (25% pregress) Associated with small vessel polyangiitis (75%) Pulmonary-renal vasculitic syndromes SMALL VESSEL VASCULITIS AFFECTING KIDNEYS Henoch-Schonlein purpura-children, IgA Cryoglobulinemic vasculitis-HCV, MPGN-I Wegener GR.-upper slower respiratory tract Churg-Strauss-eosinophilia, asthma Microscopic polyangiitis-multiple organs, lungs (-) NEPHROSCLEROSIS Benign – sustained mild hypertension – hyaline arteriolosclerosis – arterial fibrosis – glomerular hyalinization, tubular atrophy Malignant-BP>125 mm/Hg, retinal hemorrhage, papilledema, renal dysfunction – fibrinoid necrosis of arterioles – myxoid intimal expansion of arteries – microthrombi THROMBOTIC MICROANGIOPATHY Morphologic finding in several diseases Assoc: microangiopathic hemolytic anemia E/P: HUS TTP Malignant nephrosclerosis Systemic sclerosis RENAL INFARCTS Thromboemboli •Mural thrombi (M.I., atrial fibrillation) •Endocarditis •Aortic thrombi (atherosclerosis) Cholesterol emboli RENAL CORTICAL NECROSIS Cortical ischemia: thrombi, vasospasm Complication of shock • Abruptio placentae • Endotoxic shock • Hypotensive shock Cortex pale – medulla spared Massive tubular necrosis CAUSES OF ACUTE TUBULAR NECROSIS Ischemia (hypoperfusion) • Hypovolemic shock (e.g. bleeding) • Sepsis • Burns • Prolonged surgical operations Nephrotoxins • Toxic chemicals (e.g. CCl4) • Heavy metals (e.g. Hg) • Drugs (e.g. cisplatin) Heme proteins • Myoglobin (e.g. rhabdomyolysis) • Hemoglobin (e.g. hemolysis) PATHOLOGY OF ACUTE TUBULAR NECROSIS Cortex> medulla Necrotic tubular cells slough off Intratubular cast in medulla Regeneration of tubules occurs fast CLINICAL ASPECTS OF ATN The most common cause of acute renal failure “Dirty” brown casts in urine Oliguria anuria polyuria • Azotemia • Acidosis, K • Fluid retention Recovery 1-2 weeks ACUTE PYELONEPHRITIS Bacterial infection (E. coli 80%) Ascending > hematogenous Lower UTI precedes renal infection Fever, flank pain, neutrophilia Leukocyte casts in urine Healing - recurrence chronic pyelonephritis PATHOLOGY OF ACUTE PYELONEPHRITIS Unilateral> bilateral Focal PMNs in tubules interstitium Abscesses with tissue destruction PYELONEPHRITIS PREDISPOSING CONDITIONS Urinary stones Hydronephrosis Cystitis Prostatic hyperplasia Tumors Pregnancy Vesico-ureteric reflux External ureteric compression (e.g. fibrosis) PREDISPOSITION TO PYELONEPHRITIS (MNEMONIC URINE) U Urolithiasis R Reflux (vesico-ureteric) I Infections of lower UT N Neoplasms (e.g. ureteric, vesical, prostatic) E External compression (e.g.) pregnancy retroperitoneal fibrosis CHRONIC PYELONEPHRITIS PATHOLOGY Destruction of renal tissue and fibrosis • Cortical scars • Loss of papillae • Ectasia of calices • Hydronephrosis Irregularly shrunken small kidney Histology: Chronic inflammatory infiltrates •Tubular atrophy with casts (“thyroidization”) DRUG INDUCED RENAL DISEASES 1. Acute tubular necrosis(toxic) 2. Acute tubulointerstitial nephritis (allergic) 3. Analgesic nepropathy (phenacetin dose-related) METABOLIC TUBULAR INJURY Multiple myeloma – light chain casts Hyperuricemia (gout) – urate nephropathy Hypercalcemia – uric acid stones Hypercalciuria – nephrocalcinosis – calcium stones CAUSES OF HYPERCALCEMIA – HYPERCALCIURIA Primary (increased intestinal absorption of Ca) • Idiopathic (most common) • Milk-alkali syndrome • Vitamin D excess • Sarcoidosis Secondary (release of Ca from bones) • Renal osteodystrophy • Hyperparathyroidism • Osteolytic metastases (e.g. breast cancer) • Paraneoplastic syndromes (PTrP) RENAL STONES (NEPHRODITHIASIS) 1. Calcium oxalate or phosphate (75%) 2. Uric acid (15%) 3. Struvite (magnesium ammonium phosphate) and calcium phosphate (8%) 4. Cystine (1%) RENAL TUMORS Benign – oncocytoma, angiomyolipoma, fibroma (rare!) Renal cell carcinoma (most common – adults) Wilms tumor (childhood) Transitional cell carcinoma of renal pelvis RENAL CELL CARCINOMA Most common renal tumor Peak age – 60y M:F = 2:1 Incidence increasing world wide Risk factors: Tobacco; genetics (vHL-gene, familial cases) RENAL CELL CARCINOMA PATHOLOGY Yellow orange on cut surface Partially encapsulated Extends into renal vein Histology: tubular clear cell (77%) papillary (15%) granular, chromophobe, sarcomatoid (5%) RENAL CELL CARCINOMA CLINICAL ASPECTS Classical triad (hematuria, flank pain, mass) (<10%) Hematuria (50%) most common symptom Metastases-hematogenous and local abdominal Paraneoplastic syndromes (PTH, Epo, amyloid) 5 year survival = 40% WILMS TUMOR Childhood tumor (peak age 2 years) 98%< 10 years Most common abdominal solid tumor in childhood Sporadic (90%) Familial syndromic (5%) (WAGR syndrome – WT1 tumor suppressor gene Beckwith – Wiedemann syndrome – WT2) Familial nonsyndromic (5%) Unilateral (90%) Bilateral more common in familial cases (20%) WILMS TUMOR CLINICAL – PATHOLOGIC FEATURES Lobulated tumors mass – usually encapsulated Histology: mixture of immature cells metanephic, stromal, tubular Chemotherapy + surgery = 5 years = 90% Children< 2 years better prognosis