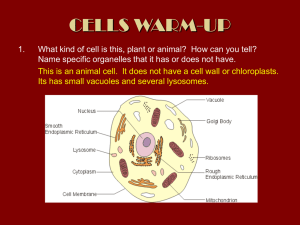
lysosomes
advertisement

Sub-cellular Pathology
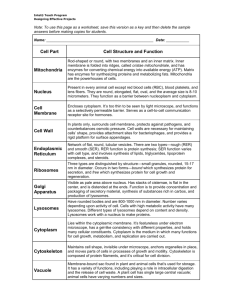
CELL ORGANELLES
AND DISEASE
Fiona McKie-Bell
BOD
Subcellular Pathology
- ‘Identification of the primary
lesion in any pathological
process in terms of the
organelles and metabolic
processes that are involved’
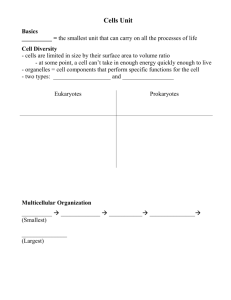
Contents
•
•
•
•
Endocytosis and lysosomes
Organelle disorders
Named diseases
Exam questions
Disorders
• PM
– Permeability
– Enzymes
– Cytolysins
– C’
– Inherited Disorders
• Nucleus
– Chromosomal
abnormalities
– Single gene defects
– Toxic damage
– Nutritional deficiencies
•
•
•
•
Mitochondrion
Endoplasmic reticulum
Cytoskeleton
Lysosomes
– General sig. In pathology
– Resistance
– Inappropriate cellular
release (intra and extra)
– Storage diseases
Differential Centrifugation
•Involve stepwise
increases in the speed
of centrifugation.
•At each step, more
dense particles are
separated from less
dense particles
•Successive speed of
centrifugation is
increased until the
target particle is
pelleted out.
The Plasma Membrane
• 'Fluid mosaic model’
• Chemically distinct from most other membranes
in the cell
– contains more sphingomyelin and cholesterol.
• Many extrinsic proteins have carbohydrate
moieties attached to them
– important in determining antigenicity of cells e.g.
blood group antigens
Structure of a typical cell membrane
Figure 10.10: (Mathews, Van Holde Biochem 3rd ed)
Effects on Permeability of the
Plasma Membrane
– Affect the sodium/potassium ATPase (sodium pump)
• Maintains electrolyte balance
– Ouabain (a plant glycoside) Digitalis (a plant steroid),
Tetrodotoxin, (puffer fish) Saxitoxin (microscopic algae - 'the red
tide')
• Can be used in the treatment of cardiac conditions
– Increase the force of contraction of heart muscle by altering
the excitability of the tissue (a function of the sodium and
potassium concentrations across the membrane).
– http://highered.mcgrawhill.com/sites/0072495855/student_view0/chapter2/animation
__how_the_sodium_potassium_pump_works.html
Effects on Permeability of the Plasma
Membrane
– Binds to the sodium
channel in the plasma
membrane and blocks
ion movement.
– Tetrodotoxin neurotoxin found in
some organs of the
puffer fish
– Saxitoxin is produced
by microscopic algae
('the red tide')
• One of only two
naturally occurring
toxins to be classified
as a Schedule 1
Chemical Warfare
agent
...and the waters that were in the river were turned to blood. And the fish that were
in the river died; and the river stank and the Egyptians could not drink of the water of
the river... Exodus 7: 20-21
Chemical & biological warfare
• 1950s – US experiments with saxitoxin as
chemical weapon
• 1000x more toxic than the nerve gas, sarin
• Used as suicide pill for U-2 spyplane pilots
• 1970 – Richard Nixon ordered destruction of all
stocks
• Now used in research into sodium ion channels
and nervous disorders
Effects of Enzymes on the
Plasma Membrane - Antigenicity
• Affecting antigenicity of cells by removing
components from the extracellular surface of the
plasma membrane e.g.
– Neuraminidase (removes carbohydrate sialic acid
groups)
• Influenza (H1N1) Haemaggluttinin, Neuramaminidase -plays its
major role after virus leaves an infected cell - ensures virus doesn't
get stuck on the cell surface by clipping off the ends of these
polysaccharide chains.
– Trypsin (removes glycopeptides).
Effects of enzymes on the
plasma membrane - Lysis
• Phospholipases
– Hydrolyse phospholipid components of the plasma
membrane
– Lead to the formation of lysophosphatides (very
potent surfactant molecules)
– Cell lysis occurs
– Found in snake venoms, some cytolytic pathogenic
bacteria (e.g.Clostridium perfringens.)
• Cytolysin e.g. Streptolysin O
– toxin produced by Streptococci
– A cholesterol-dependent cytolysin (CDC)
– causes cell lysis by interacting with the cholesterol of
the host plasma membrane, disrupting the membrane
and forming a large pore
Membrane Phospholipids
Sphingosine
– alcohol
amine
Action of Phospholipases
Found in
Snake Venoms
Complement-related membrane
injury
• When complement
becomes bound to a
cell surface, its
activation leads to the
formation of a
'membrane attack
complex'
• Causes lysis of the cell
– e.g. red cells in
incompatible blood
transfusions
Inherited membrane disorders
• Familial Hypocholesterolaemia (see later)
• Hartnup Disease
– defect in the transport proteins for uptake of the
essential amino acid tryptophan by intestinal epithelial
cells.
– Trp is an important precursor of the vitamin nicotinic
acid
• clinical signs of Hartnup disease are similar to those of the
vitamin deficiency disease, pellegra (3Ds)
• (Dementia, Dermatitis, and Diarrhoea)
Cystic Fibrosis
• Due to an inherited defect in the cystic
fibrosis trans-membrane conductance
regulator (CFTR)
• CFTR is involved in chloride ion transport
across the plasma membrane
• Important in creating sweat, mucus and
digestive juices.
• Multiple theories on Cl transport changes
and symptoms
Damage to the plasma membrane diagnostic aspects
• Changes in the permeability of the plasma
membrane can be detected by
– histochemical methods
– biochemical methods
• very useful in the diagnosis of certain diseases
The Nucleus
• Contains the genetic material of the cell
• DNA can be affected in a number of ways.
– Chromosomal abnormalities
– Single gene defects
– Toxic damage
– Nutritional deficiencies
Chromosomal abnormalities
• Alteration in the diploid number
– e.g. Down syndrome (trisomy 21) - congenital
abnormalities
• Chromosomal breakages
– e.g. ataxia-telangiectasia syndrome
– ATM Gene regulates cell cycle checkpoints, repair dsDNA, regulating
p53, BRCA1 and CHEK2, telomere repair
– Symptoms
• Dysfunction of the cerebellum
• ataxia (unsteadiness or incoordination of limbs, posture, and
gait)
• telangiectasia of the eyes and skin (a complex of abnormally
and permanently dilated blood vessels)
• severe immunological deficiency
• ‘radiosensitivity’ leading to leukaemia
Down’s Syndrome
Trisomy 21
Single Gene Defects
•
No obvious morphological abnormality
in the nucleus or chromosomes
•
Mutation (even single aa change)
– e.g. PKU, SCD (val-glu sub.)
Toxic Damage
• Chemical carcinogens
– e.g. alkylating agents such as the nitrogen
mustards
• Cancer chemotherapy
– e.g. 5-fluorouracil, methotrexate - interfere
with synthesis of DNA precursor
– vincristine - damages the mitotic spindle (not
DNA)
Nutritional Damage
• Folic acid or Vitamin B12
– deficiencies of these vitamins affect DNA
synthesis
• result in large nuclei, but with less DNA content
than optimal for mitosis
• mainly evident in red cell precursor cells in bone
marrow
The Mitochondrion
• Prime target in cellular damage caused by
hypoxia
• Affected by ‘uncouplers' of electron
transport such as dinitrophenol
• The enzymes of the electron transport
chain are inhibited by poisons such as
rotenone and cyanide
Mitochondrial diseases
• Can affect any organ at any age
• Severely debilitating and often fatal
• In USA, 50 million adults suffer from diseases involving
mitochondrial dysfunction
– Cancer, infertility, diabetes, heart disease, blindness,
deafness, kidney disease, liver disease, stroke,
migraine
– Ageing, Parkinson’s disease, Alzheimer’s disease
• Of 4 million children born in US per year, 4,000 develop
mitochondrial disease
• Many diseases still being discovered
• No cure
Mitochondrial DNA
• The mitochondrion is the only organelle apart
from the nucleus that contains DNA
• Circular DNA (linear in nucleus)
• Mitochondrial DNA maternal inheritance
– important implications in genetic analysis involving
family histories
Disorders of mitDNA
• Some inherited diseases are due to defects in
genes in mitochondrial DNA
• e.g. Leber's Hereditary Optic Neuropathy
(LHON).
– Rare disease - results in blindness (by 15-35 years)
– Due to defect in the NADH dehydrogenase (in the
electron transport chain).
– Reduced ATP formation.
LHON
•
•
•
•
Rare disorder - maternal transmission
Males never transmit LHON to offspring
Females less frequently affected than males
Results in degeneration of the optic nerve
– (nerves very dependent on ox phos)
• Main mutation in the NADH dehydrogenase
gene is at bp11778
• his - arg mutation in the enzyme
The Endoplasmic Reticulum
• Smooth endoplasmic reticulum is the site of
cytochrome P450 mixed function oxidase (CYP)
– enzyme essential in the detoxification of many
substances.
• Exposure of liver cells to certain drugs can result
in proliferation of the SER
• This can have serious consequences for
individuals who are taking more than one drug.
Induction of CYP
• CYP in the SER can be induced by several
substances
– ethanol, acetone, polycyclic hydrocarbons, and
phenobarbital
• May give rise to an increased rate of
hydroxylation and subsequent excretion of
therapeutic drugs
• Induction of CYP by one drug may stimulate the
metabolism of other drugs that are also
substrates for the enzyme
Example 1
• Rifampicin (anti-tuberculosis agent)
– induces CYP
– Increases clearance of oral contraceptives
• Increased incidence of pregnancy in
women given both drugs.
Example 2
• Phenobarbital (a barbiturate) induces CYP
• Warfarin (anticoagulant) require caution with
other meds.
• V sensitive to being metabolised rapidly by
induced CYP
• If CYP- Inducing drugs are withdrawn, CYP
levels fall
• If the warfarin dose is not also reduced
– Haemorrhage
– In some cases DEATH!
The Cytoskeleton
•
•
•
•
Microtubules (20 – 25 nm diameter)
Actin filaments (6 – 8 nm)
Myosin filaments (15 nm)
Intermediate filaments (10 nm)
Cytoskeletal Lesions
• Defects in proteins of the cytosleleton affect • Cell locomotion
– e.g. leukocyte migration
– Phagocytosis
– sperm motility (leading to infertility)
• Movement of intracellular organelles
– e.g. Chediak-Higashi syndrome, in which there is
impaired fusion of lysosomes with phagosomes
containing bacteria.
Accumulations/Disorders of
cytoskeletal proteins
• Alzheimer’s disease
– neurofibrillary tangle - composed of
neurofilaments and microtubular proteins
• Mallory body is characteristic of Alcoholic Liver
Disease.
– composed of intermediary filaments (mainly
prekeratin)
• DMD
– Gene (1987) ‘Dystrophin’
– Structurally related to spectrin
– Plays key role in anchoring cytoskeleton to
extracellular matrix
– Such anchorage may enable the plasma
membrane to withstand the stress of muscle
contraction
LYSOSOMES
• Structure and formation
• Enzymes
• Mechanisms
– Heterophagy
– Exocytosis
– Autolysis
– Crinophagy
• Sig. in pathology
– Toxin
– Micro-organisms
– Inappropriate release and disease states
– Storage disorders
See also lysosome slides
Lysosomes
• Vesicle surrounded by single membrane
– Distinct from mitochondria and microbodies
• Isolated by differential centrifugation
• Over 60 hydrolytic enzymes (acid pH optima)
known to be lysosomal in origin. Include –
–
–
–
–
–
–
Peptide hydrolases
Glycosidases
Nucleases
Phospholipases
Phosphatases
Sulphatases
Lysosomal enzymes
• Most are glycoproteins with acid pH optim
– Some (e.g. cathepsin G, and elastase) are active at
neutral pH
• The bacteriocidal enzymes lysosyme and
myeloperoxidase are found in
polymorphonuclear leucocytes
• Lysosomes - capable of degrading almost any
material of biological origin
Lysosomal membrane
• Contains cholesterol and sphingomyelin
• Also present in the plasma membrane
– but not to any extent in other membranes in
the cell
• Reflects exchange of material between the
lysosomal amd plasma membranes during
endocytosis and exocytosis
Origin of lysosomes
• Synthesis of lysosomal protein takes place in the
rough endoplasmic reticulum
• The enzymes are packages into vesicles by the
Golgi apparatus and become PRIMARY
LYSOSOMES
• Primary lysosomes fuse with vesicles of various
origin to become SECONDARY LYSOSOMES
Secondary lysosomes
• Fusion of a primary lysosome with a vesicle
containing material to be digested means that
the hydrolytic enzymes are not released into the
cytoplasm (where they could cause damage)
• Secondary lysosomes have a heterogeneous
appearance because of the variety of material
contained in endocytotic vesicles or
phagosomes
Mechanisms involving lysosomes
• Heterophagy
– Breakdown of extracellular material taken up by
endocytosis or phagocytosis
• Exocytosis
– Release of the contents of an intracellular vesicle
without loss of cytoplasm (reversal of endocytosis)
• Autophagy
– Digestion of intracellular material (cytoplasm and
organelles) within a secondary lysosome
• Crinophagy
– Disposal of excess secretory proteins
Importance of
Lysosomes in Pathology
• Lysosomes have particular importance in
pathology because they are:
– involved in reactions to toxic substances
– involved in digestion of foreign
microorganisms
– contain many hydrolytic enzymes,which, if
released inappropriately may cause both
intracellular and extracellular damage
1. Autolysis of Tissues
• a) Programmed Cell Death (Apoptosis)
– interdigital cell death in foetus - resulting in 5
fingers
– involution of the uterus and ovaries post
menopause
– atrophy of breast tissue following weaning
Role of Lysosomes in Autolysis
• b) Cell Death
• Autolysis = digestion of cell contents
• Stages
– rupture of lysosomes (as a secondary
response to the primary injury)
– release of hydrolytic enzymes into the cytosol
– digestion of intracellular material
2. Turnover of Cell and Tissue
Components
• Turnover = constant synthesis and
degradation of tissue components
• Circumstantial evidence that lysosomes
may be involved in turnover
– The necessary degradative enzymes are
present
– autophagy can be observed.
Lysosomes in Turnover?
• Some observations do not support
lysosomal involvement in turnover
– i.e. most proteins have different turnover rates
and it is difficult to account for this if there is
random uptake of proteins by autophagy.
3. Heterophagy
• Heterophagy = Intracellular digestion of
potentially pathogenic microorganisms
• Bacteria, viruses, and fungi are ingested
by macrophages and neutrophils.
Lysosomes in Neutrophils
• The neutrophil is packed with large numbers of
lysosomal granules
– rich in enzymes capable of digesting both cells and
extracellular matrix materials.
• Neurophils can actively digest pathogens, which
are then destroyed– by the generation of FRs and hypochlorous acid
– by lysosomal enzymes.
Neutrophils
• Neutrophils have membrane receptors
– for the Fc portion of antibodies
– for complement components bound to foreign
particles
– to bacterial polysaccharides.
• Foreign material is targeted
• Neutrophils do not take up material to which they
do not bind.
• Phagosomes (containing internalised material)
fuse with primary lysosomes, and digestion of
the foreign material ensues
Resistance to lysosomal digestion
• In some bacterial infections, the lysosomal system is the
vehicle by which the infection is propagated.
• The bacteria resistant to lysosomal digestion include:
• Mycobacterium tuberculosis, M. leprae, M.Brucella
• Legionella pneumophilia
• Salmonella typhi
• Listeria monocytogenes
• Shigella flexneri
• These microorganisms can survive and multiply in the
lysosomes of phagocytic cells, and as a result are
spread throughout the body (and may produce toxins).
Mechanisms of resistance
• M.tuberculosis, M.leprae, Legionnela
pneumophilia
– Inhibit fusion of phagosome with primary lysosome
• Salmonella typhimurium
– Cell wall resists digestion by lysosomal enzymes
• Listeria monocytogenes, Shigella flexneri
– Lyse the phagosome membrane
4. Intracellular release of hydrolases
producing cellular damage
• This occurs in mineral-induced lung
disease (pneumoconiosis) such as
silicosis and asbestosis.
Pneumoconiosis
• Arises from exposure to several minerals.
– Coal dust
• relatively inert
• large amounts must be deposited in the lungs
before the onset of disease.
– Silica and asbestos are more reactive and
result in fibrosis of the lung at lower levels of
exposure.
Silicosis
• Silica makes up the greater part of the
earth's crust.
• Various forms
– sand
• too coarse to pass into the periphery of the lung
• represents little danger to humans
– silica dust (2-3m diameter) is very
dangerous
High risk occupations
• Mining, quarrying, tunnelling, sandblasting,
etc.
• About 10 years exposure required for
silicosis to occur.
• In high risk occupations, 10 - 15% are
affected after 30 years.
Cause of silicosis
• Most inhaled dust is removed by
entrapment in mucus
• Followed by expulsion from lung through
ciliary movement
• If some dust reaches the alveolar duct
bifurcations - taken up by macrophages
and accumulates
Involvement of macrophages
• Uptake by macrophages is followed by
– an inflammatory response
– fibroblast proliferation
– collagen deposition (fibrosis).
Involvement of lysosomes
• Inhaled particles that are taken up by
alveolar macrophages enter the lysosomal
system.
• Interactions between the silica particles
and the lysosomal membrane (hydrogen
bonding??) results in
– disruption of the lysosome
– release of hydrolytic enzymes
Cycle of damage
• Release of hydrolytic lysosomal enzymes
results in
– death of the macrophage
– re-release of the silica particles,
• The particles are in turn taken up by other
macrophages.
• This results in another round of damage
Lung damage and fibrosis
• Thus a vicious cycle is set up resulting
– indirect lung damage through lysosomal
enzyme activity and Free Radicals
– fibrosis.
• The lung tissue becomes less elastic and
this impairs gaseous exchange.
5. Extracellular Release of Hydrolases
Producing Damage to Connective Tissue
Matrix
• Rheumatoid arthritis (RA)
• RA is an autoimmune disease that causes
chronic inflammation of connective tissue,
primarily in the joints
Rheumatoid arthritis (RA)
• The first tissue to be affected in RA is the
synovial membrane which lines the joint cavity.
• Eventually, inflammation may spread to
– the articular cartilage
– the fibrous joint capsule
– the surrounding tendons and ligaments
• This causes pain, deformity, and loss of function.
Incidence of RA
• RA affects 1 - 2% of adults
• Like most autoimmune diseases, is most
frequent in women (3:1).
Aetiology of RA
• Despite intensive research. the cause of RA
remains obscure.
• It is probably a combination of genetic,
environmental, hormonal, and reproductive
factors.
Leukocyte infiltration
• The synovial fluid may become turbid due to the
number of cells neutrophils and macrophages
present
• These phagocytes ingest the immune
complexes
• In the process of digestion, hydrolytic enzymes
are released
• These enzymes degrade synovial tissue
• Blood vessels become occluded
Involvement of lysosomes
• Occlusion of blood vessels decreases blood flow
to the synovial tissue
• This results in hypoxia and metabolic acidosis.
• The reduction in pH results in the release of
hydrolytic lysosomal enzymes from the synovial
cells into the surrounding tissue
• This initiates erosion of the articular cartilage.
Evidence for involvement of
lysosomes in RA
• Lysosomal enzymes can be detected in synovial
fluid
• RA-like symptoms can be produced if lysosomal
enzymes are injected into joints
• Vitamin A renders lysosomal membranes
unstable. Rabbits injected with Vit.A lose their
ability to prick up their ears due to loss of
proteoglycan from the ear cartilage.
Evidence for involvement of
lysosomes in RA
• Digestion of limb bone cartilage in tissue
culture can be inhibited by an antibody to
Cathepsin D (a lysosomal protease)
• Several agents used in therapy of RA (e.g.
gold, hydrocortisone) are known to have
direct effects on the function and stability
of the lysosomal membrane.
6. Lysosomal Storage Diseases
• Pompes disease
– A glycogen storage disease
• Due to inherited deficiency of 1-4 glucosidase (acid
maltase).
– Glycogen that has been ingested by autophagy
cannot be degraded, and accumulates in the
lysosomes.
– Cell death and degeneration of tissue occurs due to
release of hydrolytic enzymes from lysosomes that
have disrupted due to overloading
Lysosomal storage diseases
• Tay-Sachs Disease
– absence of -N-hexosaminidase involved in
glycolipid metabolism
• Metachromatic Leukodystrophy
– absence of arylsulphatase A, leading to
accumulation of sulphatides in the brain
Gaucher’s Disease
• The most common lysosomal storage disease
• Failure to degrade a substance normally subject
to lysosomal digestion
• Results in an accumulation of substance
• Increase in the size and number of lysosomes
• Leads to cellular malfunction and effects on
organs
Gaucher’s disease
• Incidence = 1:2,500
• Three types
– Type 1 (most common- found mainly in Jews)
•
•
•
•
Spleen enlargement
Bone lesions
CNS not involved
No serious symptoms and normal lifespan
– Type II
• Extensive CNS involvement and early death
– Type III
• Intermediate between I & II
• Dementia and spasticity by 10 years
Cause of Gaucher’s disease
• Deficiency of glucocerebrosidase
• Degrades the glycolipid glucocerebroside to
glucose and the lipid, ceramide
• Gene cloned in 1985
– 30 different mutations
– Severity predicted by nature of the mutation
• Ser for asn Type I
• Pro for leu Type II or III
Type I
• Macrophages are the only cells affected
• Macrophages in human spleen and liver
degrade 1011 red blood cells per day
• In Gaucher’s disease the greatest effect of
undigested glucocerebroside is seen in
these tissues
Treatment
• Enzyme replacement therapy
– Often impractical because of problems with
impermeability of cell membranes to extracellular
protein
• Feasible in GD because macrophages can take
up exogenous protein (e.g. glucocerebrosidase
from placenta)
– If the enzyme is modified to expose mannose
residues, this increases uptake (macrophages
recognise mannose)
Treatment
• Treatment of GD with placental enzyme
costs £250,000 per annum
• Costs may fall if genetically engineered
enzyme becomes available
• Gene therapy is a possibility